Bilateral Peripheral Facial Paralysis Combined with HIV Meningitis During Acute HIV-1 Infection: A Case Report
Yan Wu , Ge Song, Chunbo Wei Wenhui Lun *
1Department of Dermatology and Venereology, Beijing Ditan Hospital Affiliated to Capital Medical University, Beijing 100015, China 2Infectious Disease Center, Peking University Ditan Teaching Hospital, Beijing 100015, China
Key words: human immunodeficiency virus; acquired immune deficiency syndrome;acute human immunodeficiency virus-1 infection; peripheral facial paralysis
Abstract Here we reported a Chinese case of bilateral peripheral facial paralysis (PFP) in human immunodeficiency virusc (HIV) infected population. A 38-year-old homosexual male patient was referred to our hospital for bilateral facial paralysis. 21 days prior to admission he had developed high fever, chills, headache, fatigue, general malaise,nausea and vomiting. Neurological examination revealed bilateral ptosis of lower lip and cheeks, as well as failure of bilateral eyes closure. Analysis of cerebrospinal fluid (CSF) revealed pleocytosis, a marked rise of micro total protein and a marked rise of intrathecal lgG synthesis. The result of HIV-1 serology was positive by ELISA and that was confirmed by western blot. His CD4+ cell count was 180 cells/mm3. HIV-1 viral load in CSF was almost 10 times higher than that in plasma. The patient’s condition improved steadily and experienced complete resolution of bilateral PFP after 2 months.
A ppROXIMATELY 70% population of human immunodeficiency virus (HIV) infection develop neurologic complications.[1]Facial nerve is most susceptible to HIV among cranial nerves. However, peripheral facial paralysis (pFp)in patients infected with HIV, which was first reported by Snider et al. in 1983,[2]seems uncommon compared with other types of HIV-related peripheral neuropathy.Bilateral pFp, appearance of paralysis of the contralateral facial nerve within 30 days of the onset on the first side, is a very rare clinical manifestation happened on HIV infected patients, only occurring in 0.3% to 2.0%of facial paralysis cases.[3]And there are only 27 cases having been reported so far.[3-27]Here, we reported a Chinese bilateral pFp case who also had acute retroviral syndrome (ARS) and aseptic meningitis with high HIV-1 viral load in cerebrospinal fluid (CSF).
CASE DESCRIPTION
On April 3, 2018, a 38-year-old homosexual male patient was referred to our hospital for bilateral facial paralysis. He had been in his normal state of health till 21 days prior to admission. He developed high fever (up to 39°C), chills, headache, fatigue, general malaise, nausea and vomiting, but without cough, nasal congestion, runny nose or sore throat. Amoxycillin and traditional Chinese medicine was used in initiating treatment, but did not relieve his symptoms. Ten days prior to admission, he firstly experienced peripheral numbness, and then he was suddenly struck by loss of the right facial movement, failure of both eyes closing and difficulty in sucking, smiling and talking. Three days later, the left-sided facial nerve was involved.
On physical examination at admission, the patient presented with fever (37.5°C) and had cervical, axillary,and groin lymphadenectasis. Neurological examination revealed bilateral peripheral facial palsy, bilateral ptosis of lower lip and cheeks, as well as failure of bilateral eyes closure. The results of other physical and neurological examinations were normal.
Blood biochemical tests showed a slight rise in white blood cell count and alanine transaminase. Analysis of CSF revealed a pleocytosis, an obvious increase of micro total protein and a decrease of chloride level. The oligoclonal bands in both blood and CSF were negative.A noticeable rise was observed in intrathecal lgG synthesis and lgG index of CSF, as well as permeability of blood-brain barrier. Myelin basic protein (MBp) level was high in CSF, but normal in blood. MBp autoantibodies and myelin oligodendroglia glycoprotein autoantibodies both in blood and in CSF were normal. Other examined indicators were within the normal limits. (Table 1)
Serological test for HIV-1 with ELISA analysis showed positive, but showed suspected positive result with western blot. CD4+cell count was 180 cells/mm3and CD8+cell count was 1454 cells/mm3, with a marked decrease in CD4/CD8 ratio of 0.12. In plasma viral load was 9903 copies/ml, while in CSF taken 10 days before blood collection that was 95 575 copies/ml.(Table 1)
Head CT and MRI did not reveal any abnormality.Chest radiographs were normal. Tuberculin test was negative.
Considering that his symptoms improved after he was transferred from other hospital, instead of treating him with steroids we just gave him some neurotrophic drugs (VitB1, 100 mg and VitB12, 1 mg, once daily, intramuscular injection) for two weeks. After a few days of unsteadiness, an improvement was noted. And 15 days after the first serological test we took blood sample again to detect HIV-1 antibodies with western blot,and the result became positive.
One month later his CD4+cell count improved to 466 cells/mm3, meanwhile HIV-1 viral load fell to 9895 copies/ml in blood sample and only 260 copies/ml in CSF sample (Table 1). His health condition gradually improved and achieved complete resolution of bilateral pFp after 2 months. Since there was no evidence of any other underlying systemic illnesses, the diagnosis of bilateral pFp combined with HIV-1 men-ingitis associated with acute retroviral syndrome was made. Given that the patient was going abroad, he did not accept antiretroviral therapy during hospitalization.
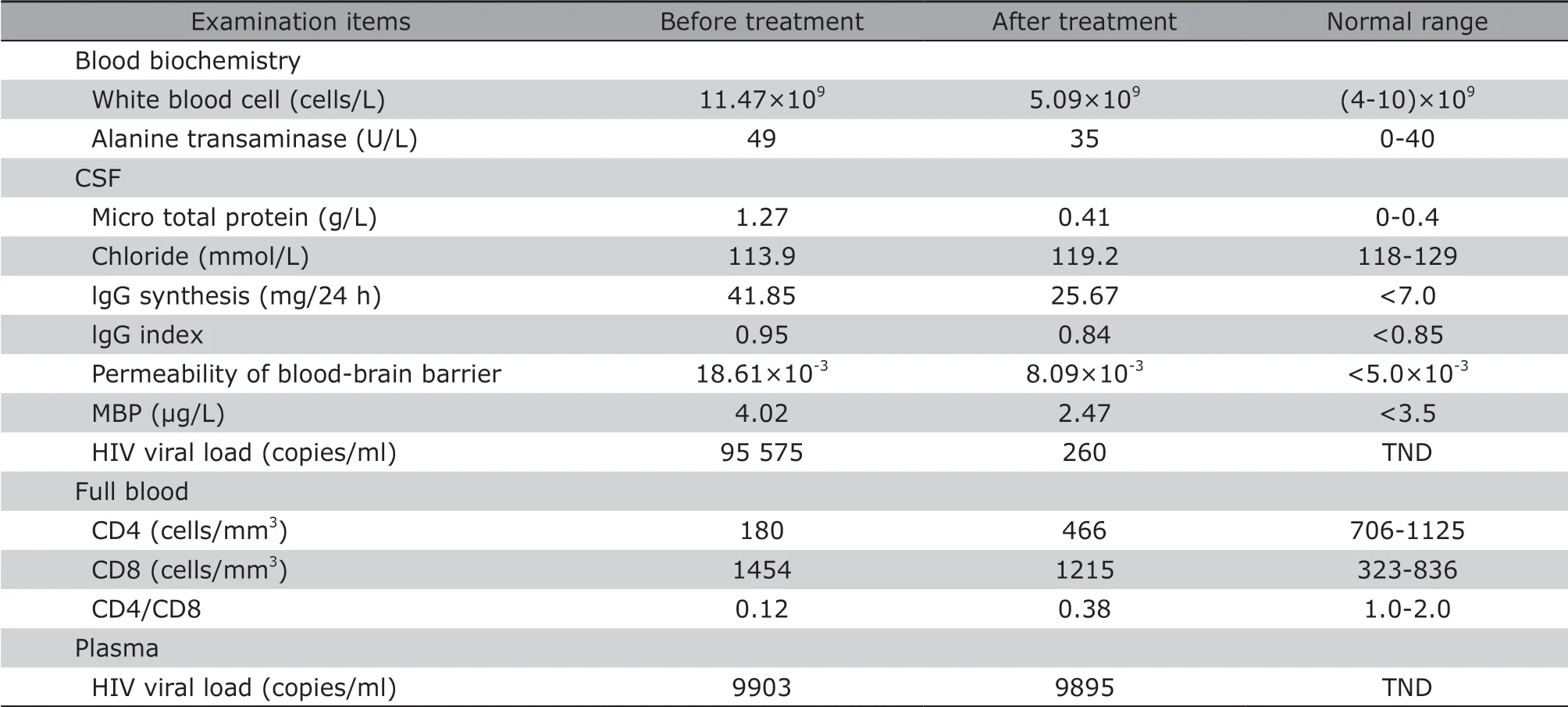
Table 1. patient’s abnormal examination results before and after treatment
DISCUSSION
Acute HIV-1 infection (AHI), an early stage of HIV-1 infection, is defined as the clinical course from the initial HIV-1 infection to the completion of seroconversion. It is estimated that 40%-90% of patients with AHI developed an acute retroviral syndrome,[28]characterized by fever, myalgia, rash, headache, and lymphadenopathy and so on.[3]Usually the clinical manifestations of AHI are nonspecific and could be resolved without any treatment. So an early diagnosis of HIV infection can be a challenge as it is easily mistaken for influenza, mononucleosis or other acute illnesses,[28]if without a high index of suspicion. Occasionally,neurologic complications occur in association with AHI.In 1983, Snider et al.[2]firstly reported 4 patients with transient aseptic meningitis during AHI, 2 of whom developed unilateral pFp. The previously reported cases[3-27]confirm that pFp can be the first symptom of HIV-1 infection, therefore, the high index of suspicion of acute HIV-1 infection is required for clinician when the patients presented with pFp and a recent flu-like illness, especially for those with high risk behavior or those in the endemic HIV areas.
However, even among patients with AHI, bilateral pFp is extraordinarily rare, as only 17 cases (including present case) have been reported worldwide during the last 30 years.[3-6,8,10-19]Bilateral pFp has never been described before during acute course of HIV infection in Chinese patients. To the best of our knowledge, this is the first report of simultaneous ARS, bilateral pFp and aseptic meningitis with high viral load of HIV-1 in CSF. This diagnosis could be made as the result of serological confirmation testing for HIV infection changed from suspected positive to positive, all symptoms resolved spontaneously, and the extensive search for other causes got negative results.
The pathogenic mechanisms of pFp in AHI patients are not well understood. A nerve lesion directly results from HIV-1 or an immunologically mediated inflammatory polyradiculopathy have been proposed.[4-5]In our present patient, bilateral pFp occurring in the early stages of the disease, with lymphocytic pleocytosis, increased proteins and high viral load of HIV-1 in CSF, supports the hypothesis of a direct lesion.It is interesting that the HIV-1 viral load in CSF was almost 10 times higher than that in plasma which was taken 10 days behind (95 575 copies/ml to 9903 copies/ml). The reason has not been completely clarified. One possible explanation is that CSF viral load is transient and it went down behind plasma viral load during AHI, it fell to 260 copies/ml rapidly accompanied with the clinical condition improvement after one month. Normally, plasma HIV viral load is higher than CSF HIV viral load.[29]Canestri et al.[30]have found that some patients who had been receiving stable combination antiretroviral therapy had CSF viral load>1 log higher than their plasma viral load because of resistance-associated mutations in CSF. In all the aforementioned 27 cases, no CSF viral load has been detected except the present report. In fact, HIV-1 could be detected by pCR in 90% of CSF specimens from HIV-1 infection subjects, and could be isolated from 80% of these patients. CSF viral load has a strong correlation with neurological symptoms, but plasma viral load alone does not correlate or predict neurological involvement.[29]And, the plasma viral load does not seem to correlate with CSF viral load.[31-32]It has been proven that patients with neurological manifestations of primary infection have an increased risk of disease progression compared with those without any clinical manifestations.[33]Unfortunately,further investigation and follow-up for this case is not available.
The clinical presentation of pFp seems highly variable in HIV-infected patients. During seroconversion,aseptic lymphocytic meningitis is commonly associated with a marked pleocytosis and rise in protein in CSF.[6-7]pFp patients with HIV infection usually present immunological meningitis,[8]which corresponds to the association of intrathecal IgG synthesis with an alteration of blood-brain barrier.[34]
Treatment of pFp in HIV-infected patients has not been systematically illuminated. Famciclovir or a highdose Acyclovir may be beneficial.[35]A short course of corticosteroids could be administered during early HIV-1 infection, especially in the cases of bilateral pFp.Researches have shown that corticosteroids use is controversial and should be reserved for the treatment of immunosuppression hosts. However, in case of bilateral involvement, steroids should be administered at least for a short period of time because of the potential ophthalmologic complications. In our opinion, this patient should be given corticosteroids treatment for a short period of time, and maintain antiviral treatment after the disease improved.
In general, HIV-related pFp is a self-fading condition, although the symptoms and signs caused by bilateral pFp are dramatically more severe than those caused by unilateral paralysis, most pFp regress within 15 days to 6 months.[8-9,35]
Conflict of interest statement
The authors have no conflict of interest to disclose.
 Chinese Medical Sciences Journal2019年1期
Chinese Medical Sciences Journal2019年1期
- Chinese Medical Sciences Journal的其它文章
- Vertebral Artery Dissection Probably Caused by Massage: A Case Report
- Successful Treatment of Severe Heparin-induced Thrombocytopenia with Intravenous Immunoglobulin, Platelet Transfusion and Rivaroxaban: A Case Report
- Prediction of Hidden Blood Loss During Posterior Spinal Surgery
- Value of Magnetic Resonance Imaging Texture Analysis in the Differential Diagnosis of Benign and Malignant Breast Tumors
- Value of Texture Analysis on Gadoxetic Acid-enhanced MR for Detecting Liver Fibrosis in a Rat Model
- MRI Histogram Texture Feature Analysis of the Optic Nerve in the Patients with Optic Neuritis
