Clinical characteristics and surgical outcomes of congenital inferior rectus palsy with compensatory head posture of facial rotation
Xuzhou Municipal Hospital Affiliated to Xuzhou Medical University; Xuzhou No.1 People’s Hospital; Xuzhou Eye Hospital, Xuzhou 221001, Jiangsu Province, China
Abstract
INTRODUCTION
Limited literature exists about isolated inferior rectus (IR) palsy, especially congenital origin. In 1991, von Noorden[1]made a report on 21 patients with congenital, traumatic, vascular, and myasthenic unilateral isolated IR palsy and described the clinical manifestations and surgical treatment effect on these patients. In 2012, Awadein[2]described the clinical findings, orbital imaging, and intraoperative findings of 28 patients with isolated IR muscle palsy caused by orbital wall fracture, iatrogenicity, tumor, and other health conditions. Recently, Akbarietal[3]reported successful surgical treatment of 22 patients with isolated IR palsy. Among these cases, 54.5% was traumatic, 40.9% was congenital, and 4.5% was vascular.
In 1953, Warwick[4]observed that the IR subnucleus is in an unique area, which is at the rostral level of the oculomotor nucleus complex that allows for the possibility of the IR to be affected independently and without the paralysis of other muscles innervated by the oculomotor nerve. Recently, Tsudaetal[5]also put forward this point. In this article, we introduce the clinical features and surgical effect of 15 patients with congenital isolated IR palsy with compensatory head posture of facial rotation in detail.
SUBJECTS AND METHODS
The study and data collection were approved by the Research Ethics Committee of Xuzhou Municipal Hospital Affiliated to Xuzhou Medical University and followed the tenets of the Declaration of Helsinki. Patients with abnormal facial rotation position and hypertropia from May 2014 to July 2018 were retrospectively identified through the review of clinical manifestations. Informed consent was obtained from all patients. The patients included in this study showed a congenital isolated IR muscle underaction with a deficiency of depression in the abduction and hypertropia of largest angle in the action of the IR muscle. Exclusion criteria included traumatic extraocular muscle paralysis, inflammatory myopathy, the paralysis of other extraocular muscles, mechanical restriction by orbital wall fracture, myasthenia gravis, and so on.
Age, sex, affected eye, medical history, and time to presentation were reviewed. Deviations at the near (33 cm) and far (6 m) distance fixation were measured with prism and alternate cover test was performed when a prism in front of paretic eye was observed. The measurement of the deviation of vertical and horizontal misalignments was done in primary position before and after surgery, and the deviations were also measured in eight diagnostic positions of gaze. If a refractive error was present, it was completely corrected to fully control the accommodation. Stereopsis was tested with the Titmus test.
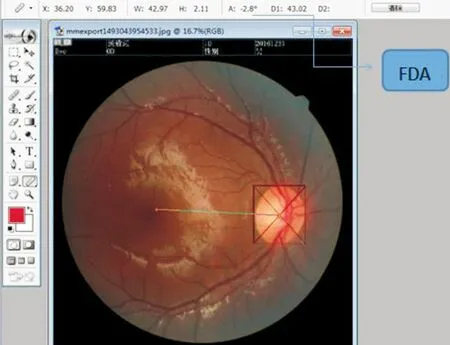
The objective evaluation of eye torsion was assessed by fundus photography before and after surgery. The head of the patient was stabilized in the chin and forehead rests. Thus, the patient’s head was straight while being photographed. Meanwhile, the eye being examined focused on the light mark in the fundus camera. The image obtained was used to measure the torsion angle with software for image processing (Photoshop 7.0). Four lines were drawn tangent to the upper, lower, medial, and lateral extremities of the optic disc, forming a rectangle. Then, the intersection of the two diagonal
Figure1Imageobtainedwasusedtomeasurethetorsionangle(FDA)withPhotoshopsoftwareforimageprocessing.
lines is the center of the optic disc. Thus, the angle[6]formed by the horizontal line and the line connecting the center of the optic disc to the center of the fovea can objectively evaluate ocular torsion called “torsion angle” or fovea-disc angle(FDA). The angle below the horizontal line through the center of the optic disc was positive angle. The above angle was negative (Figure 1). According to the experience summed up by former scholar[7], the FDA is from 5.6°-7.0° with the fovea below the centre of the optic disc.
Any abnormal head posture was recorded by orthopedics goniasmometer. The abnormal head position includes the abnormal variation along the horizontal axis, vertical axis, and longitudinal axis. In this study, the abnormal head posture of these patients mainly manifested as facial rotation along the vertical axis. When the subjects were asked to sit upright, one arm of the goniasmometer was perpendicular to the body. The other arm was perpendicular to the face (Figure 2). Then, the angle formed by arms can be read from the goniasmometer to reflect the degree of compensative facial rotation posture.
Both axial and coronal computed tomography images were obtained with 2-mm slice thickness in five patients of 12 subjects toexclude intracranial lesions.
The versions and ductions of all those patients were analyzed. The eye movement examination to determine the underaction of the IR muscle was combined with forced duction test in the operation to exclude other extraocular muscle dysfunction and restrictive strabismus. Forced duction testing was performed on both eyes intraoperatively under general anesthesia, and the tightness and fibrosis of extraocular muscles were also recorded.
All surgeries were done by one of the authors and performed through fonix incisions. The resection of the IR was lonely performed when the vertical deviation in primary position between 10 and 35 prism diopter (PD). The IR muscle resection combined with superior rectus recession was performed in one patient whose vertical deviation in primary position was 40 PD. Considering the over correctness in primary position after the surgery of vertical muscle, the inferior oblique muscle myectomy was carried out in two patients with the vertical deviation in primary position of 6 and 8 PD.
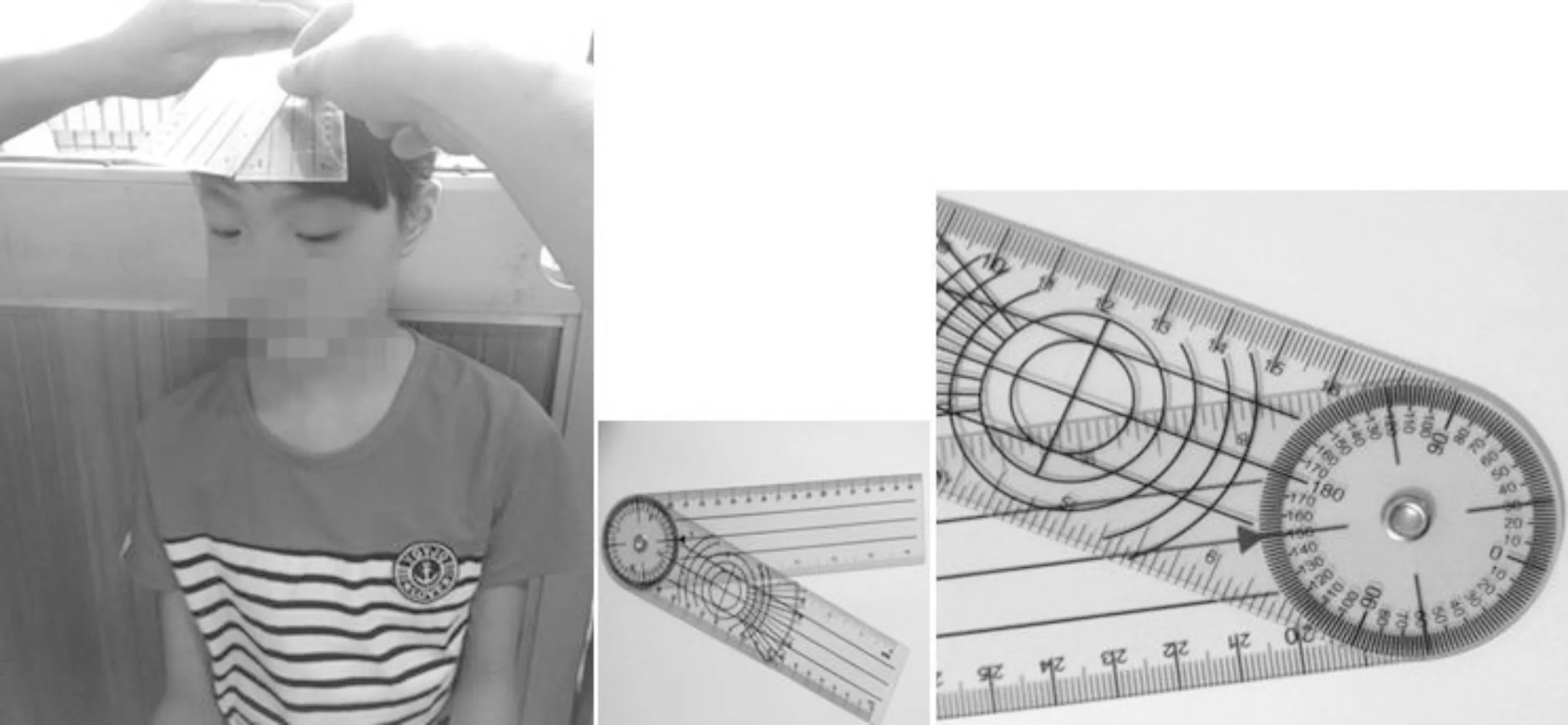
Figure2Onearmofgoniasmometerwasperpendiculartothebody,theotherarmwasperpendiculartotheface.Theangleformedbyarmsreflectedthedegreeofcompensativefacialrotationposture.
Table1Changesoffacialrotation,cyclotropia,andverticalandhorizontaldeviationinpatientsbeforeandafteroperation
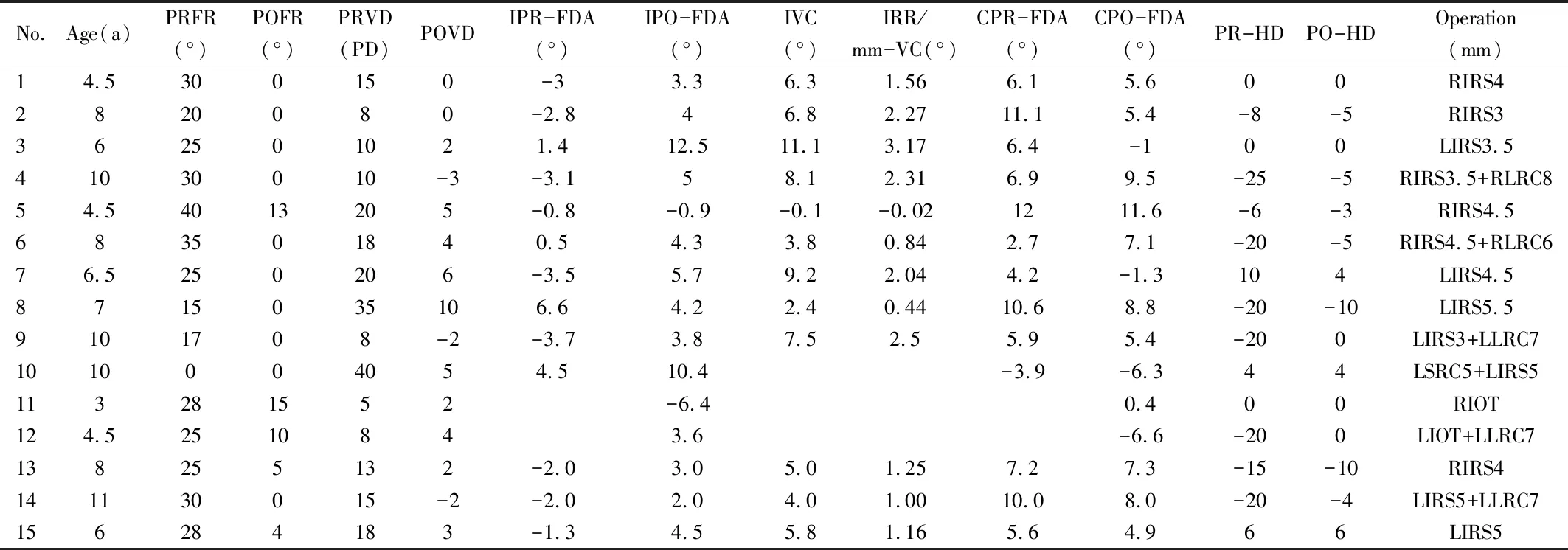
No.Age(a)PRFR(°)POFR(°)PRVD(PD)POVDIPR-FDA(°)IPO-FDA(°)IVC(°)IRR/mm-VC(°)CPR-FDA(°)CPO-FDA(°)PR-HDPO-HDOperation (mm)14.5300150-33.36.31.566.15.600RIRS42820080-2.846.82.2711.15.4-8-5RIRS3362501021.412.511.13.176.4-100LIRS3.541030010-3-3.158.12.316.99.5-25-5RIRS3.5+RLRC854.54013205-0.8-0.9-0.1-0.021211.6-6-3RIRS4.5683501840.54.33.80.842.77.1-20-5RIRS4.5+RLRC676.5250206-3.55.79.22.044.2-1.3104LIRS4.58715035106.64.22.40.4410.68.8-20-10LIRS5.59101708-2-3.73.87.52.55.95.4-200LIRS3+LLRC71010004054.510.4-3.9-6.344LSRC5+LIRS5113281552-6.40.400RIOT124.52510843.6-6.6-200LIOT+LLRC7138255132-2.03.05.01.257.27.3-15-10RIRS4141130015-2-2.02.04.01.0010.08.0-20-4LIRS5+LLRC7156284183-1.34.55.81.165.64.966LIRS5
PRFR: Preoperative facial rotation; POFR: Postoperative facial rotation; PRVD: Preoperative vertical deviation; POVD: Postoperative vertical deviation; IPR-FDA: Ipsilateral preoperative fovea-disc angle; IPO-FDA: Ipsilateral postoperative fovea-disc angle; IVC: Ipsilateral variety of cyclotropia; IRR/mm-VC: Variety of cyclotropia of each 1 mm of IR resection; CPR-FDA: Contralateral preoperative fovea-disc angle; CPO-FDA: Contralateral postoperative fovea-disc angle; PR-HD (PD): Preoperative horizontal deviation (prism degree); PO-HD: Postoperative horizontal deviation; RIRS: Right inferior rectus resection; LIRS: Left inferior rectus resection; RLRC: Right lateral rectus recession; LSRC: Left superior rectus recession; RIOT: Right inferior oblique myectomy.
The subjects were followed up at 1wk and 3-6mo after surgery. The collection of statistical data was based on the return visit of 3-6mo. In every follow-up visit, we recorded changes in vertical and horizontal deviations and eye rotation, including the disappearance of compensative facial rotation position, the improvement in underaction of the IR, and stereopsis in any fixation eye position. At the same time, the patients were questioned about diplopia, especially in the primary position and downward gaze of the reading position and residual abnormal head position. The same examiner, who was masked in the medical history of patients and in the surgical procedure, performed all the measurements. Success was defined as good sensory fusion in the primary and downward positions of gaze with normal head posture. Vertical and horizontal deviation and cyclotropia were all corrected, and anomalous head posture disappeared.
The variables of vertical, horizontal and rotational strabismus before and after operation were all in accordance with normal distribution. The changes of the degree of facial rotation, vertical deviation, and cyclotropia were analyzed by paired T test. The correlation between vertical deviation and facial rotation was analyzed by bivariate correlation analysis. Statistical analysis was performed with SPSS statistics version 22 (SPSS Inc.). The significance level was established less than or equal to 0.05.
RESULTS
In this paper, 15 patients (8 males) were diagnosed with congenital isolated IR muscle palsy, whose onset age ranged from 1-3 years old and without other clear causes. Mean patient age was 7.1±2.4 (range 3-12)years. All patients underwent obvious facial rotation posture as main compensative head position, and all had unilateral IR muscle paralysis. The right eye was seven (50%). In our cohort, the detailed clinical feathers of all patients were summarized in Table 1. All these patients had vertical deviation and different levels of horizontal strabismus and incyclotropia in primary position. With the sound eye fixing, the mean hypertropia in the primary position was 15.83±2.15 (range 4-30)PD, which was decreased to 1.83±1.13 PD after surgery. Variations in horizontal deviation and cyclotropia are described in Table 1. In addition, nine (60%) patients showed exotropia and three (20%) patients showed estropia in horizontal direction in primary position. The remaining (20%) patients showed no misalignment in horizontal direction in primary position.
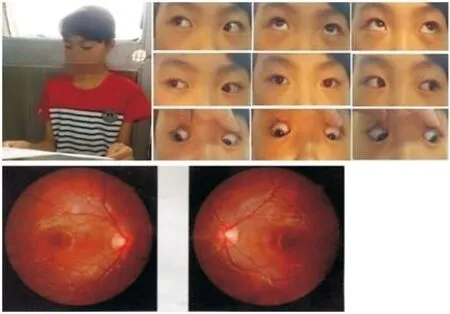
Figure3Preoperation(Case3)
Compensative facial rotation to right 30° along vertical axis, underaction of the right IR muscle. Right eye: incyclotropia. Stereopsis: (Titmus test): 40".
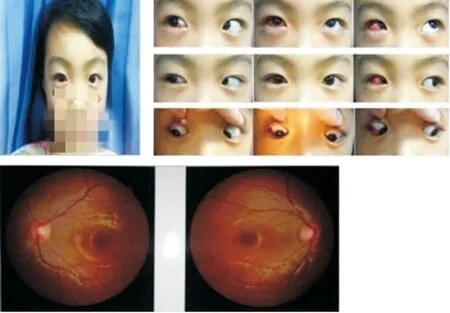
Figure4Postoperation(Case3)
Abnormal head posture and vertical, horizontal, and rotational strabismus were corrected. Stereopsis:(Titmus test): 40".
We performed a detailed statistical analysis of 12 patients (Cases 1-9, Cases 13-15) with the IR resection lonely in paralytic eye. They all had perfect surgical results in which abnormal head posture and vertical, horizontal, and rotational strabismu were corrected (Figures 3 and 4). The mean vertical deviation in the primary position was 15.83±2.15 (range 4-30)PD, which decreased to 2.08±1.10 PD after the only IR resection. The difference was statistically significant (P=0.000,t=10.411). In Case 4 and Case 9, the hypertropia was slightly overcorrected. However, the patients had normal stereopsis and did not experience discomfort. The mean value of FDA changed from -1.14±0.84° (preoperation) to 4.28±0.89° (postoperation) in the paralytic eye. The difference was statistically significant (P=0.000,t=-4.969). In this article, we have drawn the experience that shorting each millimeter of the IR muscle can make 1.54°±0.93° external rotation of the eyeball. The mean value of FDA changed from 7.39°±0.84° (preoperation) to 5.94°±1.11° (postoperation) in the sound eye, and a slight intraocular rotation in the non-paralyzed eye was observed. However, the difference was not statistically significant(P=0.167,t=1.479). Lateral rectus muscle recession was performed in Cases 4, 6, 9, 13, 14 and the horizontal deviation was perfectly corrected. Three patients without horizontal strabismus (Cases 1, 3 and 11) were observed. A decreased tendency of horizontal strabismus was found after performing the only IR resection in the remaining patients (Cases 2, 5, 7 and 8). In these patients (Cases 1-9, Cases 11-15), the mean degree of facial rotation along the vertical axis was 26.67°±2.07°, which decreased to 1.83°±1.13° after surgery. The difference was statistically significant(P=0.000,t=14.380). No statistical significance occurred in the correlation between the degree of facial rotation and the vertical deviation before surgery (P=0.843,r=-0.058).
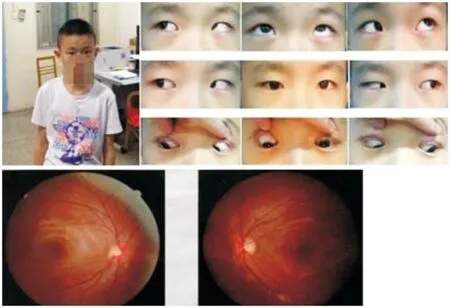
Figure5Preoperation(Case10)
Compensatory head position disappeared. The left eye as the paralytic eye did not show incyclotropia, but the non-paralytic eye showed incyclotropia.
In all 15 patients, except for Cases 11 and 10, stereopsis tests were good (Titmus test: 40-200″). Case 11 was too young (3 years old) to fail to cooperate with stereopsis examination. One year ago, Case 10 had an apparent compensatory head position of facial rotation according to the patient’s mother. However, with the deterioration of the disease, the fusion function in the case of compensatory head position cannot maintain approximate binocular visual function in normal people. That is, a loss of compensation existed, and the compensatory head position disappeared under the circumstances. No stereoscopic vision was found before surgery. Furthermore, the dominant eye of the patient was the left eye of the paralytic eyes. The fundus image examination showed that the left eye as the paralytic eye did not show incyclotropia, but the non-paralytic eye had incyclotropia (Figures 5 and 6).
In Case 11 (Figure 7), at 33 cm distance, the vertical deviation in primary position was right high left (RHL) 6 PD.In the right gaze of 30° direction, the RHL was 12 PD. In the left gaze of 30° direction, the RHL was 4 PD. At the bottom of the right was RHL 12 PD. The fundus photography examination was not performed before the operation. Both macula were located near the horizontal line across the lower boundary of the optic disc through indirect ophthalmoscopy after general anesthesia, which hinted no incyclotropia. Combined with passive traction test in the operation, no apparent fibrosis and tension of the extraocular muscles were observed. Then, the Brown syndrome was excluded. Thus, the patient was diagnosed with congenital superior oblique palsy (SOP) Knapp class V[8-9]. In consideration of RHL 5 PD less than 10 PD in primary position, the myectomy of the right inferior oblique muscle was selected in the case of the overcorrection of vertical strabismus if the resection of the IR muscle was performed. After the surgery (Figure 8), the vertical deviation in primary position was eliminated, but the apparent vertical deviation was RHL 12 PD in the right and down-right gazes. The facial rotation along the vertical axis to the right was apparent. Meanwhile, the image of the fundus was found to be unbelievably an apparent intorsion during the postoperation regardless of the effect of the internal rotation of the eyeball by the inferior oblique tenotomy. Case 12 had the same disease change as in Case 11.
No obvious atrophy, dysplasia, malposition, inflammation, and adhesion of extraocular muscle were found through computed tomography images examination among the five subjects.
DISCUSSION
The IR muscle is innervated by the inferior branch of oculomotor nerve. The oculomotor nerve branches into the inferior and superior divisions through the cavernous sinus and further divides into the fibers of each extraocular muscle in posterior orbit. The oculomotor nerve innervates the four extraocular muscles (medial, superior, and inferior recti, and inferior oblique). Therefore, an obstacle is present during the elevation, adduction, and depression of the eye. In clinical practice, incomplete oculomotor paralysis is more common, that is, previous reports of paralysis of the inferior rectus muscle were mostly accompanied by paralysis of the superior rectus and medial rectus muscles. Incomplete. However, the isolated palsy of single IR muscle especially caused by congenital dysplasia is rare and exist.
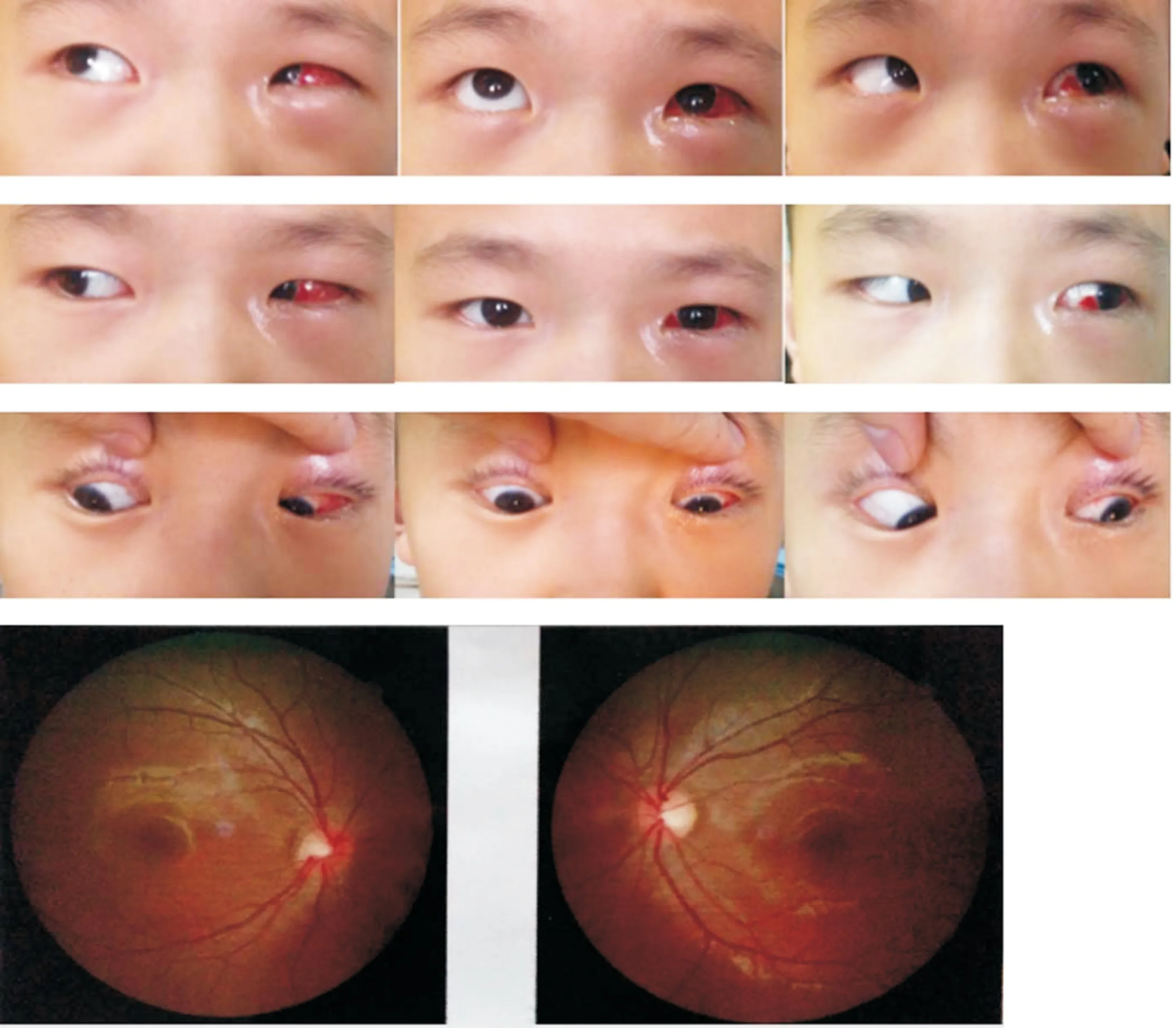
Figure6Postoperation(Case10)
The 5 mm recession of superior rectus muscle of the left eye and 5 mm resection of the IR muscle were performed. With the correction of the vertical strabismus, the underaction of the left IR muscle and the overaction of the superior rectus muscle disappeared in postoperation. Meanwhile, the eye movement coordination and excyclotropia of the left paralytic eye appeared after surgery. However, stereopsis examination is still free.
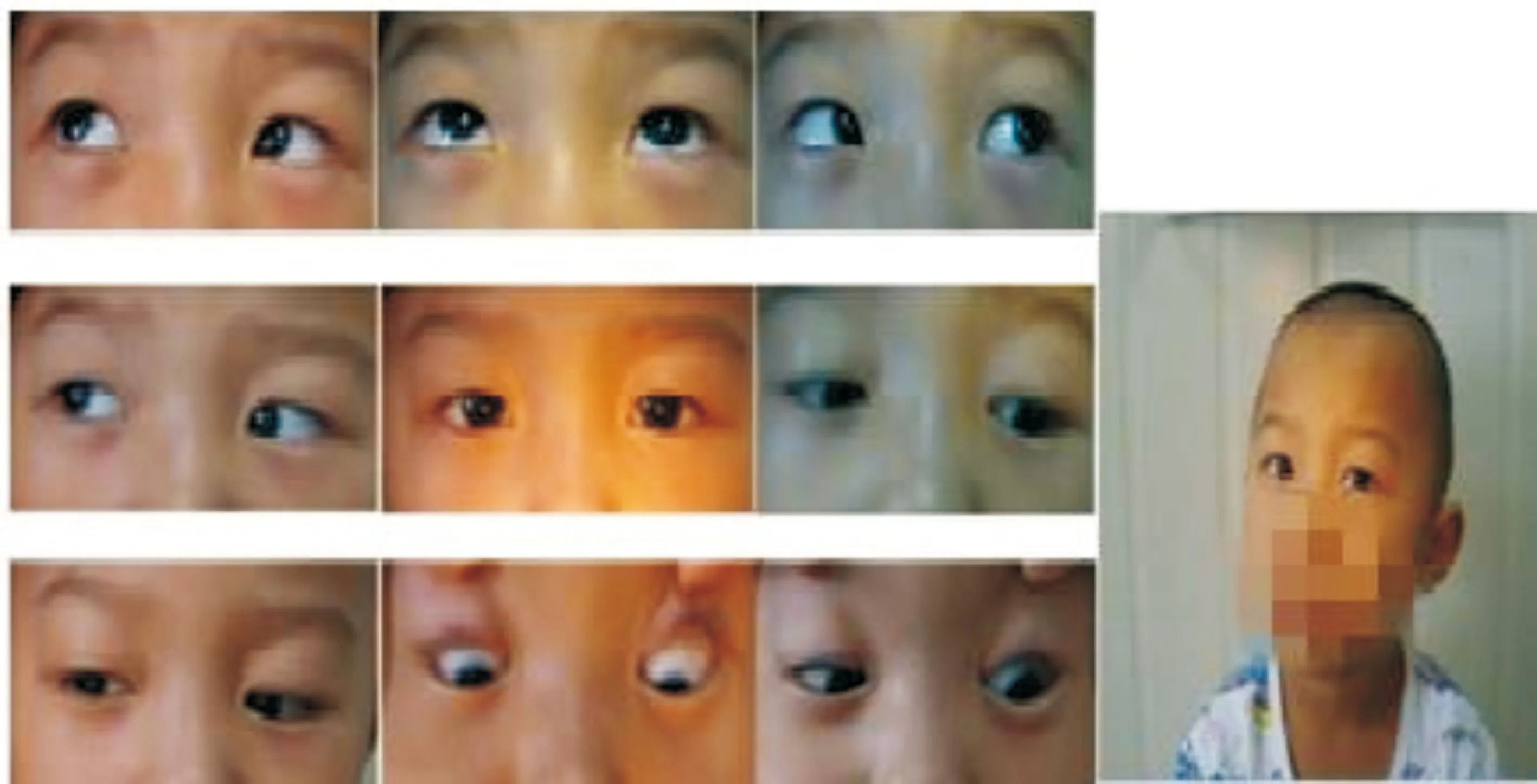
Figure7Pre-operation(Case11)
Both maculae were located near the horizontal line across the lower boundary of the optic disc through indirect ophthalmoscopy after general anesthesia, which hinted no incyclotropia. The patient was diagnosed with congenital SOP Knapp class V, excluding the Brown syndrome.
Choietal[8]reported 44 IR palsy of acquired origin, analyzed, and pointed out that the pathological anatomic site leading to IR palsy may be the prenuclear descending pathway from the rostral interstitial nucleus of the medial longitudinal fasciculus to the ipsilateral IR subnucleus, the IR subnucleus itself, the IR fascicle, the terminal branch of the oculomotor nerve supplying the IR muscle, its myoneural junction, or the IR muscle itself. Choietal[8]and Leeetal[9]proposed that the IR fascicle and other oculomotor fascicles are somatotopically arranged from medial to lateral in the ventral midbrain, as shown in Figure 9. Some causes of isolated IR palsy have been reported, including multiple sclerosis[10], benign and metastatic tumors[11], cerebral infarction in the brainstem[9], hypoplasia[12-13], restriction after sub-Tenon’s anesthesia[14]and rupture after blunt orbital trauma[15]. Similarly, cases of congenital diseases also exist.
Von Noordenetal[1]reported 21 patients with isolated IR paralysis. Among them, six cases were explicit congenital patients, and five cases were idiopathic. He believed that most of these five idiopathic patients might also have congenital isolated IR paralysis. At the time of birth, no
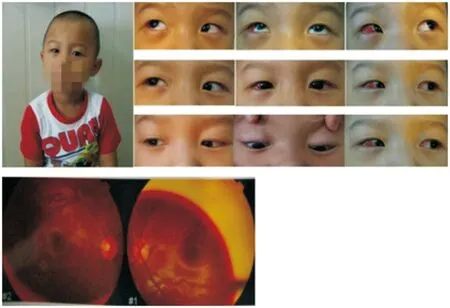
Figure8Postoperation(Case11)
The vertical deviation in primary position was eliminated, but an apparent vertical deviation remained RHL12 PD in the right and down-right gazes. The facial rotation along the vertical axis (Y-axis) to the right remained clear. Meanwhile, the image of the fundus was found to be unbelievably an apparent intorsion during the postoperation (-6.4°).
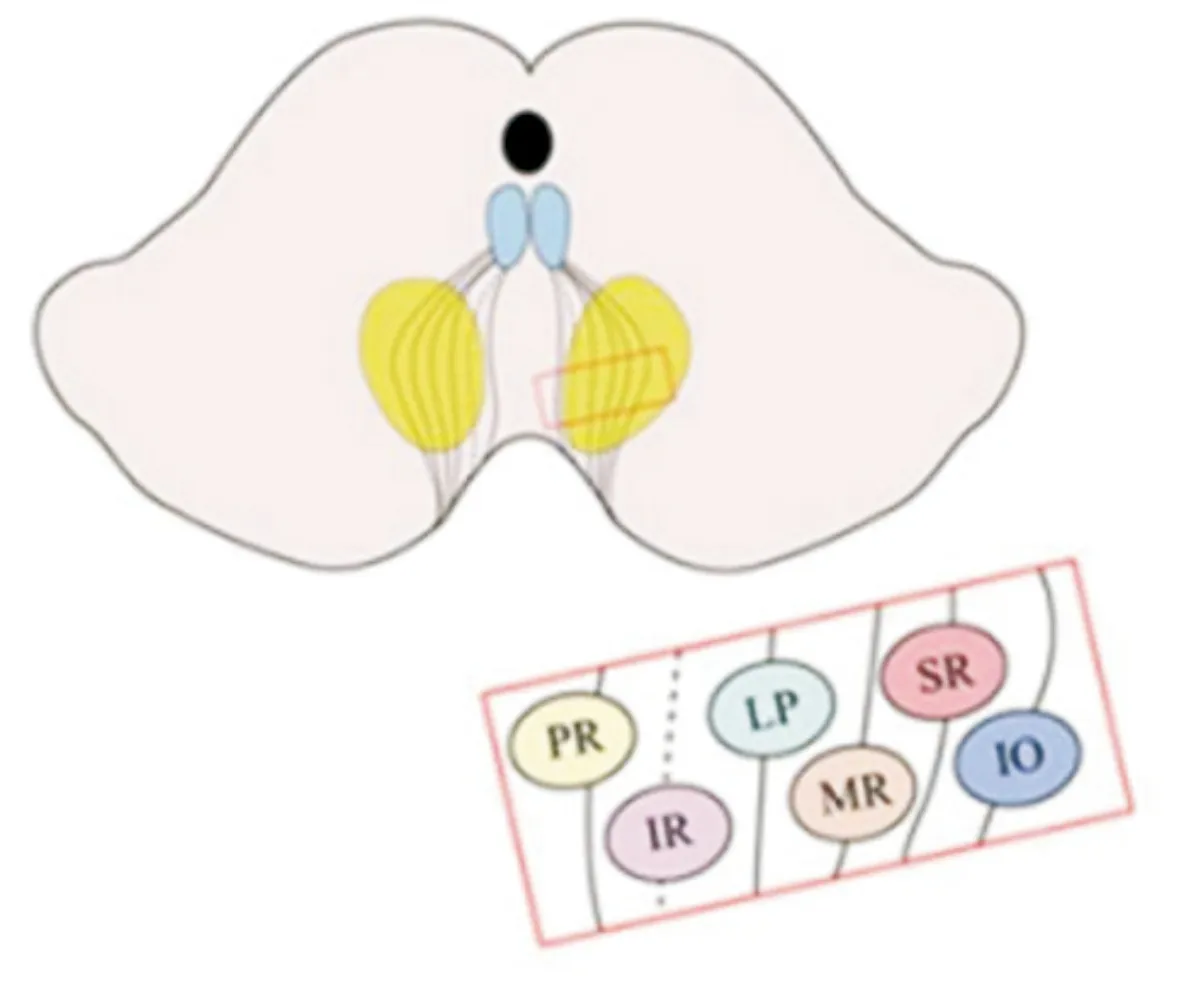
Figure9Topographicorganizationofoculomotorfascicles
PR: Pupillar fiber; LP: Levator palpebrae; SR: Superior rectus; IR: Inferior rectus; MR: Medial rectus; IO: Inferior oblique.
typical performance was observed in idiopathic cases because the conditions of the patients were not serious after birth, or the patients had good compensation, fusion function, and decompensation or deterioration in the course of time that led to typical clinical features. Akbarietal[3]described the clinical features and surgical outcomes of 22 patients with isolated IR muscle paralysis, and nine (40.9%) patients with history of hypertropia since birth of all 22 subjects were considered congenital. Awadein[2]also reported one congenital IR muscle paralysis of 28 patients with isolated IR muscle paresis or underaction. Understanding of the structure of the oculomotor nerve nucleus was credited to Warwick[4]. He observed retrograde degeneration in the oculomotor nucleus after the extirpation of individual extraocular muscle in monkeys. He arrived at a conclusion that the IR subnucleus acted as a unique position[16], which was at the most rostral level of the oculomotor nucleus complex. The characteristics of this anatomical structure allowed the IR to be affected independently from other extraocular muscles innervated by the oculomotor nerve. Unilateral congenital IR palsy is not common, and we should pay enough attention to this disease.
The congenital IR muscle underaction was seldom reported maybe because it was diagnosed as other diseases, such as congenital SOP Knapp class V, A pattern strabismus, skew deviation, Brown’s syndrome, and so on. Differential diagnosis between these rare diseases is often difficult. In SOP Knapp Class V[17], the greatest hypertropia is across the lower fields of gaze, and the underaction of the ipsilateral superior oblique (SO) and IR muscle can be presented in both SOP and IR palsy. However, the paralyzed eyes of patients with SOP Knapp V showed excyclotropia, or in some cases, excyclotropia of the contralateral eye[18]. The paralyzed eyes of patients with IR paralysis showed incyclotropia. We also found that contralateral incyclotropia was performed in a few cases. The underaction of IR and the overaction of SO are common characteristics of A pattern strabismus, skew deviation, Brown’s syndrome, and IR palsy[19-21]. Siatkowskietal[20]reported that the vertical misalignment of the visual axes following damage to the supranuclear control areas for ocular movement is termed skew deviation, which results from the unilateral or asymmetric disruption of the central graviceptive input in the roll plane as it ascends from the utricles to the interstitial nucleus of Cajal in the mesencephalon. Posterior cranial fossa and cerebellar lesions, and conjugate fundus rotation are often seen in skew deviation. A pattern strabismus as a special kind of horizontal strabismus with the difference of the horizontal deviation of upward between downward greater than 10 PD is distinguished from the IR palsy with vertical strabismus caused by vertical muscle paralysis. Excluding the Brown’s syndrome can be performed by a technique of forced ductions[21].
In this paper, the compensatory head positions of twelve patients of all 15 subjects were presented with facial rotation along the vertical axis. Two patients were presented mainly with facial rotation along vertical axis accompanied with tortile head along longitudinal axis. A patient lost the compensatory head posture due to the disappearance of fusion with the deterioration of the condition. The correlation analysis showed that no significant correlation occurred between the vertical deviation and the degree of facial rotation. We analyzed that the IR palsy caused vertical strabismus in different degrees, and then patients mainly adopted fusion and abnormal compensatory head positions to reduce the deviation of strabismus, obtain binocular vision, and relatively perfect stereopsis as the normal. Furthermore, compensatory head position is mainly for vertical strabismus but not for the obvious cyclodeviation[22]. The fusion function can control the orthophoric only during small vertical deviation. Vertical strabismus is revealed only when the fusion function is broken by alternate covering. When the vertical deviation of strabismus increased with the use of fusion function, different types of abnormal head posture, including facial rotation along vertical axis, head tilt along longitudinal axis, chin up and down along horizontal axis, or their mixed form, can be used to obtain relatively perfect binocular single vision function. The facial rotation along vertical axis is the main head posture of compensation in patients with congenital IR muscle paralysis. Through the facial rotation to the ipsilateral and combined with the use of fusion function, the body can get a good binocular single visual at the contralateral field of view where the vertical deviation is smallest. On the basis of the above, the vertical deviation of some patients is still too apparent to maintain a relatively normal binocular single vision and stereopsis. Tilting head to the contralateral as an additional supplement can be made to achieve binocular single vision function. In this paper, no patient with chin up and down was found. Kimlinetal[23]and Urquhart (the author and the subject of that paper) reported a similar case of congenital inferior rectus paralysis. Sensory tests revealed adaptation patterns that varied with gaze direction and showed a cyclotorsional element.
After surgery, all patients, except for Cases 11 and 12, showed that the vertical strabismus disappeared, the eye movements became coordinated, and the abnormal head position disappeared. The resection of IR is effective and perfect. Similar cases and treatments were also reported by Akbarietal[3]. Mild overcorrection and undercorrection do not influence curative effect. In case 11, without fundus photography examination before the operation, only in preliminary judgment that both maculae were located near the horizontal line across the lower boundary of optic disc through indirect ophthalmoscopy after general anesthesia, incyclotropia was excluded, and then he was diagnosed as congenital SOP Knapp V[17]in no rigorous way. The myectomy of right inferior oblique muscle was performed in the case of overcorrection caused by resection of rectus muscle in patients with little verticle deviation (6 PD RHL) in the primary position. Postoperatively, the image of the fundus was found to be unbelievably an apparent intorsion regardless of the effect of the internal rotation of the eyeball by the myectomy of inferior oblique. Thus, incyclotropia was presumed to occur preoperatively. Therefore, this patient should be diagnosed with congenital IR palsy. The incoordination of eyeball movement existed after the operation and destroyed the fusion function of patients. Thus, the abnormal compensatory head position did not improve significantly. Case 12 also had a similar condition.
Statistical analyses from Cases 1-9 and Cases 13-15 were performed by only IR muscle resection and showed that the different levels of incyclotropia in most of the patients were significantly improved postoperatively. The changes of FDA between preoperation and postoperation were statistically significant, and we have concluded that each shortening of 1 mm of the IR muscle corrected 1.54°±0.93° incyclotropia. However, no apparent incyclotropia occurred in paralytic or contralateral sound eyes in Case 8. Vertical strabismus in the primary position was found to be 35 PD by prism and alternate cover test, which was the largest. However, the fusion and stereopsis were perfect; Titmus stereopsis inspection was 40". To our surprise, the patients maintained orthophoric during hirshberg inspection and had only facial rotation 15° to ipsilateral based on the perfect fusion function. We speculated that the perfect fusions of the ability that controls the vertical strabismus and incyclotropia were allright. In Case 10, incyclotropia was not presented in the paralytic eye but obvious incyclotropia in the contralateral sound eye. With a gradually deteriorated and decompensated condition, the loss of binocular single vision and stereopsis made the former typical facial rotation described by the patient’s mother also disappeared. Pre-operative examination showed that the paralytic eye was the dominant eye at times. We believe the phenomenon (paradoxical cyclotropia) that no incyclotropia occurred in the paralysis eye but existed in the contralateral eye, which might be caused by the paralytic eye as the dominant eye[1,24]. Kimlinetal[23]described that intorsion of both eyes was apparent, provided the patient was fixating with the paralytic eye, which he can do voluntarily. Meanwhile it disappeared if fixating with the sound eye. Retinal correspondence status and suppression were dependent not only on gaze direction but also on which eye was fixating.
A number of limitations were encountered in this study. The number of subjects was small. Fundus photography and orbital imaging were not available for all patients. Fundus torsion was recorded by assessing the location of the fovea in respect to the optic disc, which is a subjective method and its accuracy may be limited by the determination of the location of the fovea. Both A pattern strabismus and IR palsy have similar characteristics in eye movement: SO overaction and IR muscle dysfunction. On the surface, binocular attack is possibly presented in most of A pattern strabismus and unilateral underaction in most of congenital IR palsy conditions. The links and differences between A pattern strabismus and congenital IR palsy are not clearly explained in this document. The exact cause of congenital IR palsy remains unclear as most strabismus diseases. Clark[25]found that some of the patients who had been diagnosed with marked SO overaction had a superior mislocation of at least one lateral rectus pulley by 1.8 mm to 4.9 mm. Thus, they put forward the idea that pulley heterotopy should be one of the causes of incomitant strabismus. Guyton[26]given his point of view that ocular torsion due to the loss of fusion was the key to understanding the mechanisms involved in cyclovertical strabismus. Kushner[27]proposed that patients manifesting SO palsy and inferior oblique hyperfunction had a normal cross-sectional area of the extraocular muscle. He also presented a potential mechanism of the altered contractility of the normal cross-sectional area of the extraocular muscle by a shift in fiber type and distribution within a normal-sized muscle due to the vergence adaptation or any change in neural stimulus to the anatomically normal muscle. The diverse causes of IR palsy are worthy of our further study in clinical work in the future.

