Secondary sex ratio of assisted reproductive technology babies
Nathira Abdul Majeed, Charley Zheng, Alex Polyakov, Megan Pucci, Mohamed Hatta Tarmizi, Mie Mie Cho Win
1Royal Women's Hospital, Melbourne, Victoria, Australia
2Royal Women's Hospital and Melbourne IVF, Melbourne, Victoria, Australia
3Oceania University of Medicinea, Australia
4Sabah Women's and Children's Hospital, Kota Kinabalu, Sabah, Malaysia
5Obstetrics & Gynaecology Department, International Medical School, Management & Science University, Selangor, Malaysia
Keywords:Artificial reproduction technology Intracytoplasmic sperm injection In-vitro fertilization Secondary sex ratio
ABSTRACT Objective: To assess the secondary sex ratio (SSR) of assisted reproduction technology babies within a fertility clinic in Melbourne, Australia.Methods: A retrospective cohort study was conducted on 3 369 babies who were born following single embryo transfer between 2011 and 2016. Variables examined included embryo creation date, maternal and paternal ages, maternal body mass index (BMI), type of infertility,sperm parameters, fertilization method, type of embryo and stage of transfer. Multivariate regression analysis was performed on the data set using STRATA V9.2.Results: More males were found to be born to embryos created in summer (adjusted odds ratio=1.46, 95% confidence interval: 1.08-1.95; P=0.01). Lower BMI of mother (≤30 kg/m2)and younger age of parents (≤35 years) were associated with an increase in SSR (50.1% vs.47.1%; 50.6% vs. 48.8%; 50.0% vs. 48.9%) respectively. Decreased SSR value was associated with primary subfertility, using in-vitro fertilization procedure and fresh embryo compared to those with secondary subfertility, using intracytoplasmic sperm injection procedure and thawed embryo (49.3% vs. 50.6%; 47.1% vs. 50.8%; 49.4% vs. 50.1%) respectively.Conclusions: The fertilization methods, type of embryo, stage of embryo transfer, parameters of the sperm and status of subfertility do not significantly affect the SSR. SSR is affected by the seasonality, maternal age, and BMI.
1. Introduction
Sex ratios in general populations have been noted to be related to a wide variety of reasons in many parts of the world. Social status,war, girl-child infanticide, or merely discrimination in the way of caring girls, are responsible for higher female mortality and increase in male survival. Since the 1980’s, approximately 80 million missing females have been resulted from sex-selective abortion in China and India. Countries with a surplus of males now reaching adulthood have found a number of problematic consequences. Many men living with low socioeconomic status have concerns about their inability to marry. The study of Wei et al[1] pointed out that the potential for marginalization in society could lead to antisocial behaviours and violence. As a consequence, societal stability and security might be threatened[2].
Secondary sex ratio (SSR), also known as sex ratio at birth,is the ratio of male live births to 100 female live births[2,3]. A comprehensive analysis was completed in 2014 by the University of California to explore the contributing factors that affect sex ratios in early human development. By accessing data from the embryos of Day 3 to Day 6, chorionic villus sampling, amniocentesis,termination of pregnancy, fetal deaths and live births, it is found that an initial sex ratio at conception is to be unbiased. However, beyond conception, male offspring increases in the first trimester and mortality of female fetus is higher than male during total pregnancy.The resultant birth ratio is therefore skewed in favor of males[4].
Studies have proved that numerous biological and environmental factors are associated with SSR. It is found that reduction of SSR in natural conception is related with elderly maternal age, emotional stress and some social factors[5-9]. Concerns about the impact of invitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI)on SSR have also emerged through various studies on SSR in IVF and ICSI babies[10-12].
Although conclusions have not been definitive, a trend is apparent whereby SSR in assisted reproduction technology (ART) babies resulted from IVF procedures is higher than those conceived with ICSI[6,10,12,13]. Additionally, many studies also demonstrate that higher SSR is seen in male babies after blastocyst-stage embryo transfer compared to those born following cleavage-stage embryo transfer in the same period of time[10-12,14,15]. However, further studies are still required for more understanding about the changes of SSR in ART related factors.
This study aims to assess the SSR of ART babies within a fertility clinic in Melbourne, Australia. The parameters of “IVF vs. ICSI” as well as “blastocyst embryo transfer vs. cleavage stage transfer” were fundamental inclusions. Further parameters, incorporating a greater number of variables, have also been addressed to potentially elude to the contributing factors in skewed sex ratios.
2. Materials and methods
This retrospective analysis was prepared from a single large fertility unit based in Melbourne, Australia. Data were obtained through a centralized database. The study population included 3 369 babies who were born following single embryo transfer during the period of 2011 to 2016. Donor cycles, preimplantation genetic diagnosis or preimplantation genetic screening and twin pregnancies were excluded from the analysis. Approval of ethics for the study was received on 4th February 2019 through the Department of Health and Human Services Human Research Ethics Committee (HREC number - 67/19, MIVF), Melbourne, Victoria 3000, Australia.
Variables examined included embryo creation date (summer or other seasons), maternal and paternal ages, maternal body mass index (BMI), type of infertility, sperm parameters, fertilization method (IVF or ICSI), type of embryo (fresh or frozen) and stage of transfer (cleavage or blastocyst). For each variable used, the ratio of male to female babies and the SSR were calculated. Moreover,multivariate regression analysis was performed on the data set using STRATA V9.2 (Copyright STRATA Corp, Texas USA) to find out the statistical significance of the factors effecting SSR in ART babies. Finally, the trend of SSR values against the methods of fertilization (IVF vs. ICSI), type of embryo (fresh vs. thawed) and the stage of transferred embryo (cleavage vs. blastocyst) was studied.
3. Results
In total, 3 369 women were included into this study, and 1 674(49.7%) male babies and 1 695 (50.3%) female babies were born.The mean age of women and their partners were (34.0±4.9) years and (36.7±5.5) years, respectively.
The SSR was stratified by main demographic characteristics of the patients, type of infertility, sperm parameter status and different ART procedures (Table 1). A significant sex ratio imbalance towards males of 54.2% (male: female = 118 : 100) was found when the dateof embryo creation was performed in summer, compared to 48.7%(male: female = 95:100) if the procedure was not undertaken in summer. Furthermore, we also recognized higher SSR in younger maternal and paternal age group (≤35 years) and lower BMI group (≤≤30 kg/m2) (50.3% vs. 48.4%; 50.6% vs. 48.8%; 50.1%vs. 47.1%), respectively. The study also found lower SSR value in primary subfertility, IVF procedures and fresh embryo transfers than those with secondary subfertility, ICSI procedures and thawed embryo transfers (49.3% vs. 50.6%; 47.1% vs. 50.8%; 49.4% vs.50.1%) respectively. The study did not identify sperm parameter status and stage of embryo at the time of transfer as the significant contribution to the change in SSR.
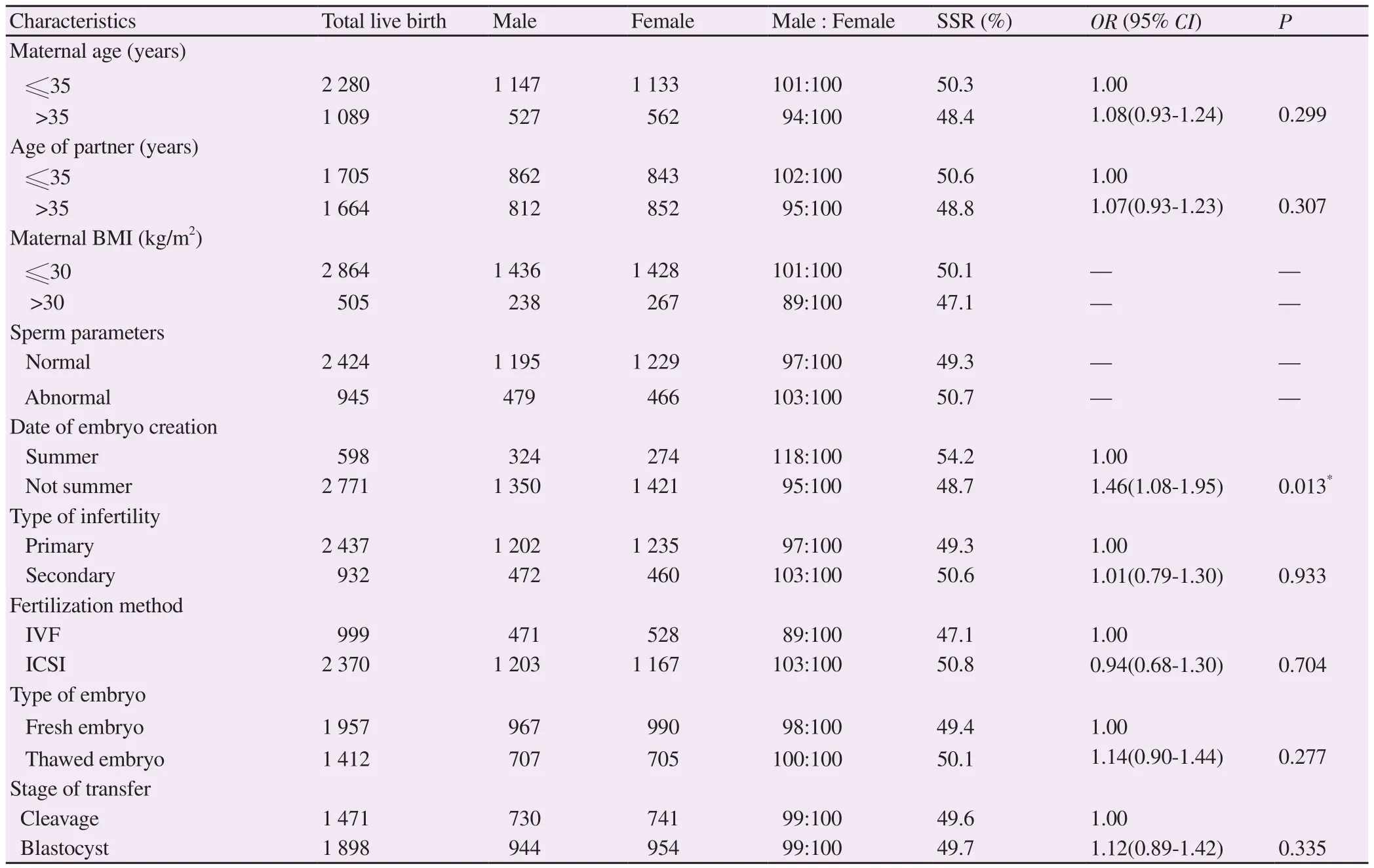
Table 1. Secondary sex ratio stratified by different demographic characteristics, types of infertility, sperm parameter and ART procedures.
Multivariable logistic regression was done, and the results were showed in Table 1. After adjusting for confounding factors, the creation of embryo during summer was the only factor which was significantly associated with SSR in both IVF and ICSI babies[adjusted odds ratio (OR)=1.46, 95% confidence interval (CI): 1.08-1.95; P=0.013]. Regarding the method of fertilization, the use of IVF was associated with a decrease in SSR value (adjusted OR=0.94,95% CI: 0.68-1.30; P=0.704), whereas thawed embryo transfers was associated with an increase in SSR (adjusted OR=1.14, 95% CI:0.90-1.44; P=0.277). However, no changes in SSR were identified in term of cleavage/blastocyst stage embryo transfers.
In order to see the different effects of ART procedures on SSR, all of the data from each subgroup was analyzed (Table 2-4). As we found in Table 2, for the pregnancies resulted from blastocyst stage embryo transfer, the SSR was significantly higher in ICSI group when compared with IVF group (51.4% vs. 46.6% in fresh embryo;52.0% vs. 44.1% in thawed embryo). However, the SSR was similar in IVF/ICSI babies for patients undergoing cleavage transfer.
The comparison of SSR in terms of embryo stage against other variables was explained by Table 3. It was clearly seen that cleavage stage embryo transfer was associated with increased SSR in IVF group (49.0% vs. 46.6% in fresh IVF; 51.9% vs. 44.1% in thawed IVF). However, there was no significant effect on SSR between using fresh and thawed embryo in IVF/ICSI (Table 4).
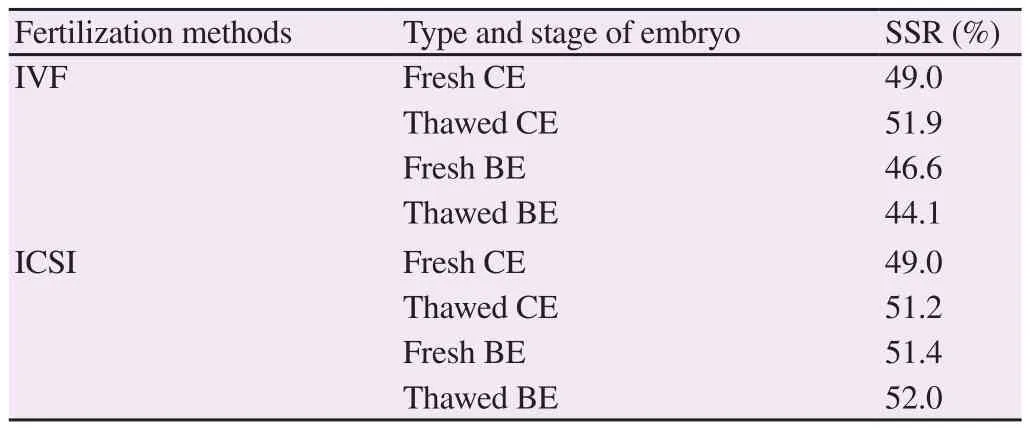
Table 2. SSR in different fertilization methods (IVF/ICSI).
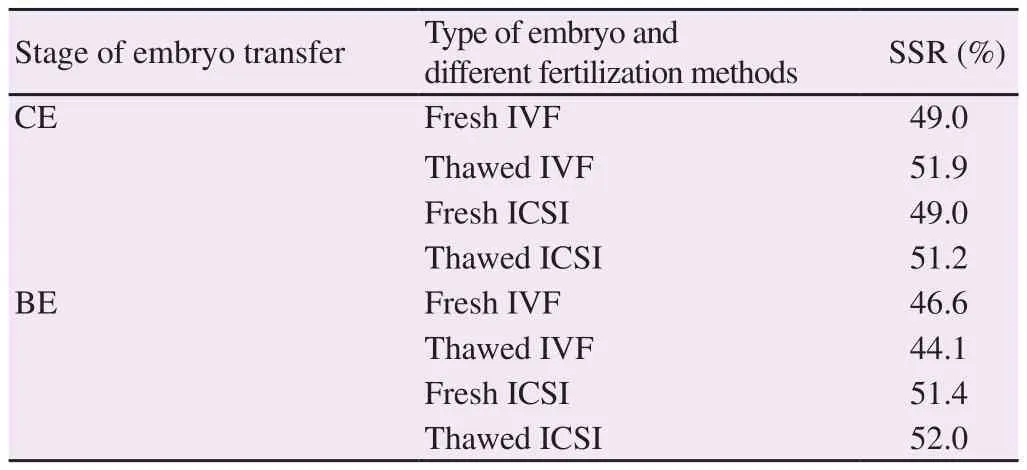
Table 3. SSR in different stages of embryo transfer (CE/BE).

Table 4. SSR in use of fresh and thawed embryo.
4. Discussion
Our study revealed that sex ratio was closely related to the seasons,where the SSR was found to be significantly higher when embryo creation occurred during summer when compared to any other time of the year. Even after adjusting for confounding factors, the creation of an embryo during summer (adjusted OR = 1.46, 95% CI: 1.08-1.95; P=0.013) was the only factor that was significantly associated with SSR in both IVF and ICSI.
Certain animal species, such as the crocodile, undergo dependent sex determination. That is the temperature at which eggs are incubated determines the sex of the offspring. Whilst such a mechanism has not been elucidated, there may possibly be such a mechanism even in the mammalian world. Temperature, heat and indeed radiation may all be such causative factors[16]. In our study,we found there was, for unknown reasons, a statistically significant higher number of males born when embryo creation was in summer.Studies have showed that natural environmental factors have significant impact on SSR mainly in terms of synchronizing built-in rhythms. Among these, temperatures and seasons are the important environmental factors that influence fecundity in mammals. A link between human fertility, temperature and seasonal birth patterns has also been reported[17,18]. Another study carried by Rojansky et al[19] described that the highest fertilization and quality of embryo were observed during the spring, and in the autumn, the lowest fertilization and quality of embryo were observed[20].
While these papers were not directly linked to sex ratio, several other explanations existed for seasonal variation and the rate of fertility. The hormone called melatonin may be responsible because of its local effect. Natural cycle of melatonin levels is typically changing in response to light and dark. Mammals of all kinds have physical responses to this cycle and the most obvious can be seen in the natural sleep/wake patterns. Vahidi et al[21] found in IVF treatment cycles, successful conception was more common in early spring from March to June while the minimum conception was seen in autumn (22% vs.14%), respectively. It indicates in-vitro fertilization has been effected by the seasons but they concluded that more data are needed to conclude the exact time for best results[22].Our study also revealed that lower BMI (≤30) and younger age of parents (≤35) were associated with an increased SSR. Mechanisms defining the regulation of sex ratio in animals and humans have been long questioned. Several factors appear to be involved,particularly parental condition. In humans, a sex ratio biased towards females was seen in smoking parents[23,24], in older mothers[25,26],in older fathers[26,27] and in women with metabolic alterations,like diabetes[28,29]. Some researches indicate specific paternal age involvement of >40 years[26,27], maternal age of >40 years[30], and multiparty as being another factor[26,30].
Other research has indicated that higher semen concentration and total motile sperm count significantly increase the odds of getting Y-chromosome spermatozoa, which may lead to sex imbalance at birth in infertile males[31].
The use of ICSI is typically employed when male infertility factor is found. Its use in the USA has substantially increased in recent decades, from 11.0% of ART cycles in 1995 up to 57.5% of cycles in 2004[13]. Data from a number of countries have shown that by comparison to IVF, ICSI significantly reduces SSR, thereby showing a bias towards female offspring[10,32-35].
In our study, SSR was not altered in patients who underwent ICSI.Our study also elucidated that IVF had a lower SSR, however this was not statistically significant. These findings are contrary to the current consensus that IVF procedure significantly produces more male live births than ICSI procedure[3,14].
There is no enough conclusion regarding the use of ICSI and reduced SSR. The study of Ménézo[25] concluded that reduced number of Y-bearing sperm in male partner may be responsible as ICSI is used in patients with male infertility factor, frequently with poor spermatogenic function[36]. However, it should be noted that studies have found the decreased SSR in offspring following ICSI in patients with normal spermatogenic function (unexplained infertility). It is suspected that an increase in Y-chromosome abnormalities may directly affect embryogenesis[13].
Since SSR could be affected by other factors in IVF and ICSI, we explored the association between SSR and fertilization methods in subgroups. Our results showed that in ICSI procedures, the SSR was lower in cleavage embryo transfers compared to blastocyst transfers.However, SSR was higher in ICSI than IVF. Recent evidence from meta analyses and large population-based studies have suggested that blastocyst embryo transfer is associated with a sex ratio imbalance towards males[21,1]. A number of reasons have been offered. The most prominent rationale is that of morphological selection criteria.It is proposed that clinicians may select more male blastocysts for transfer due to their capacity to cleave at a faster rate than female embryos. This occurs from day two until blastocyst stage is reached.Male embryos also have a faster preimplantation development rate than female embryos[10,37]. Tarín et al[36] provided an excellent paper detailing the molecular mechanisms observed and X-chromosome inactivation likely involved in gender selection, and loss of females throughout pregnancy[38].
However, two recent retrospective studies[39,40] assessed the mean number of cells and embryo grades of male and female babies. No difference in growth and delivery rates between male and female embryos was found. The authors concluded that blastocyst transfer and selection of higher grade embryos were not associated with an increased SSR. In our study, the SSR in the blastocyst transfer subgroup was higher than those of cleavage stage embryo transfer,however this was seen in the ICSI method only.
In our present study, we also explored the effect of SSR on fresh vs. frozen embryo transfers. To date, very few studies have reported a difference, and results are mixed[10,13,32,34]. Our study showed that SSR was not significantly related to the type of embryo (fresh or frozen) according to multivariate logistic regression analysis and after controlling related factors. Subgroup analysis also showed that SSR was consistently not affected by frozen embryo transfer.
In conclusion, the data collated in this study assessed the relation of SSR in ART. A greater number of variables contributing to the causation of SSR were assessed in comparison to those provided by previous studies. Interestingly, our data did not produce the same skewed results as shown by previous researchers when assessing IVF vs. ICSI or blastocyst-stage vs. cleavage-stage. The differences seen in these subgroups did not reach statistical significance in our study. Of curious note, there was a statistically significant difference found in SSR when assessing seasonality where greater number of male were born when embryos were created in summer compared to other seasons of the year. This was established in both IVF and ICSI procedures. Correspondingly, patients with a lower BMI and of younger parental age showed an increased SSR, however, it was not statistically significance. Further research is called for in order to investigate rationale involved in seasonality and SSR.
Conflict of interest statement
All authors declare that there is no conflict of interest.
 Asian Pacific Journal of Reproduction2019年2期
Asian Pacific Journal of Reproduction2019年2期
- Asian Pacific Journal of Reproduction的其它文章
- Comparison of p38 MAPK, soluble endoglin and endothelin-1 level in severe preeclampsia and HELLP syndrome patients
- Oestrous cycle of Wistar rats altered by sterol and triterpenes rich fraction of Adansonia digitata (Linn) root bark - A scientific rationale for contraceptive use
- Improvement of Phaseolus vulgaris on breastfeeding in female rats
- Effect of Vitex agnus-castus plant extract on polycystic ovary syndrome complications in experimental rat model
- Effect of combination of Gynura procumbens aqueous extract and Trigona spp. honey on fertility and libido of streptozotocin-induced hyperglycaemic male rats
- Review on canine pyometra, oxidative stress and current trends in diagnostics
