Risk factors for cervical lymph node metastasis in papillary thyroid microcarcinoma: a study of 1,587 patients
Xiangqian Zheng, Chen Peng, Ming Gao, Jingtai Zhi, Xiukun Hou, Jingzhu Zhao, Xi Wei, Jiadong Chi,Dapeng Li, Biyun Qian
1Department of Head and Neck Tumor, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin, Tianjin's Clinical Research Center for Cancer,Tianjin 300060, China; 2Department of Head and Neck, Shanxi Cancer Hospital, Taiyuan 030013, China; 3Department of Ultrasound, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin, Tianjin's Clinical Research Center for Cancer, Tianjin 300060, China;4Department of Epidemiology, School of Public Health, Shanghai Jiao Tong University, Shanghai 200240, China
ABSTRACT Objective:The purposes of this study were to identify risk factors for cervical lymph node metastasis and to examine the association between BRAFV600E status and clinical features in papillary thyroid microcarcinoma (PTMC).Methods:A total of 1,587 patients with PTMC, treated in Tianjin Medical University Cancer Institute and Hospital from January 2011 to March 2013, underwent retrospective analysis. We reviewed and analyzed factors including clinical results, pathology records, ultrasound results, and BRAFV600E status.Results:Multivariate logistic regression analyses demonstrated that gender (male) [odds ratio (OR) = 1.845, P = 0.000], age (< 45 years)(OR = 1.606, P = 0.000), tumor size (> 6 mm) (OR = 2.137, P = 0.000), bilateralism (OR = 2.011, P = 0.000) and extrathyroidal extension (OR = 1.555, P = 0.001) served as independent predictors of central lymph node metastasis (CLNM).Moreover, CLNM (OR = 29.354, P = 0.000) served as an independent predictor of lateral lymph node metastasis (LLNM). Among patients with a solitary primary tumor, those with tumor location in the lower third of the thyroid lobe or the isthmus were more likely to experience CLNM (P < 0.05). Univariate analyses indicated that CLNM, LLNM, extrathyroidal extension, and multifocality were not significantly associated with BRAFV600E mutation.Conclusions:The present study suggested that prophylactic neck dissection of the central compartment should be considered in patients with PTMC, particularly in men with tumor size greater than 6 mm, age less than 45 years, extrathyroidal extension, and tumor bilaterality. Among patients with PTMC, BRAFV600E mutation is not significantly associated with prognostic factors. For a better understanding of surgical management of PTMC and the risk factors, we recommend multicenter research and long-term follow-up.
KEYWORDS PTMC; risk factors; CLNM; LLNM; BRAFV600E mutation
Introduction
Papillary thyroid microcarcinoma (PTMC) is defined by the World Health Organization (WHO) as a papillary thyroid carcinoma (PTC) ≤ 1 cm1. Clinically, fine needle aspiration biopsy (FNAB) and ultrasonography (US) are utilized to detect PTMC in patients without palpable thyroid nodes.Although PTMC has an indolent course, many cases have demonstrated highly aggressive clinical features, such as extrathyroidal extension and cervical lymph node metastasis.The incidences of central lymph node metastasis (CLNM)(24.1%-64.1%)2-5and lateral lymph node metastasis(LLNM) (3.7%-44.5%)2for PTMC are comparable with those of PTC.
BRAF mutation is a common genetic alternation in thyroid carcinoma. The most common and typical mutation in the BRAF gene is T1779A in exon 15, which results in a V600E amino acid substitution6. However, controversial results have been observed in studies of PTMC, as some research has shown that BRAFV600Emutation in PTMC led to more aggressive behavior7,8, whereas other studies found that the BRAFV600Emutation was not significantly related to high-risk clinicopathologic characteristics9.
As the clinical features of PTMC and the risk factors for CLNM have been previously investigated10-13, the aim of the present study was to examine the risk factors for lymph node metastasis, including both CLNM and LLNM, based on US results and postoperative pathological records in the setting of a large cohort of Chinese patients with PTMC.
Materials and methods
Patients
A total of 3,789 patients with PTC were initially treated at Tianjin Medical University Cancer Institute and Hospital from January 2011 to March 2013. Among these patients,1,587 were diagnosed with PTMC based on postoperative pathology.
All patients underwent indirect laryngoscopy before and after surgery. Preoperative US, performed in all cases,provided information regarding disease and possible cervical LNM. When preoperative findings were suspicious for LNM,computed tomography (CT) was performed. Preoperative FNAB was not performed routinely in patients with PTMC.Primary thyroid tumor location was divided into four regions: upper third, middle third, lower third, or isthmus,according to US imaging results.
Different therapeutic strategies were used for different types of PTMC, such as lobectomy with isthmectomy plus ipsilateral central lymph node dissection (CLND) for unilateral PTMC, isthmectomy plus prophylactic bilateral CLND for isthmus PTMC, and near-total thyroidectomy plus bilateral CLND for multiple tumors limited to a single thyroid lobe. Moreover, patients with multiple bilateral tumors were treated with total thyroidectomy with bilateral CLND, and patients with US and CT findings suspicious for LLNM were treated with ipsilateral lateral lymph node dissection, including levels II-V. Surgical treatments for the 1,587 patients are shown in Table 1.
Extrathyroidal extension, tumor size, tumor number, and presence of LLNM and CLNM were confirmed by two pathologists independently in a blinded fashion. Cases in which findings were inconsistent were discussed with a third pathologist. Extrathyroidal extension was defined according to gross infiltration evident at the time of surgery or by microscopic evidence on pathologic examination.Multifocality was defined as the presence of more than one tumor lesion in the thyroid. The maximum diameter of the primary tumor was defined as tumor size in multifocal cases.
Postoperative complications were also evaluated.Temporary hypoparathyroidism was defined as serumcalcium < 8 mg/dL within 6 months after surgery. Permanent hypoparathyroidism was defined as low calcium levels in a patient with low/absent parathyroid hormone levels 6 months after surgery. Vocal cord paralysis was defined as temporary recurrent laryngeal nerve injury within 6 months after the operation; vocal cord paralysis continuing longer than 6 months was defined as permanent laryngeal nerve injury.

Table 1 Surgical treatment in 1,587 patients
Follow-up data were available for all 1,587 patients, and the follow-up period ranged from 40 to 72 months. All patients underwent US every 3-6 months in our hospital during follow-up. This retrospective study was approved by the Institutional Review Board of Tianjin Medical University Cancer Institute and Hospital.
DNA extraction and analysis of BRAFV600E mutation
DNA was extracted from paraffin-embedded tissues using a kit (Tiangen, Beijing, China) according to the manufacturer's instructions. Specifically, we selected unstained tumor tissue areas on 2 mm thick sections for comparison to hematoxylin and eosin-stained sections. For small tumors, we adopted laser-capture microdissection to collect tissues. Tumor samples were incubated in TE9 for 2 days at 37°C, with fresh proteinase K added daily. Samples were then centrifuged, and the supernatants were digested for an additional 2 days at 55°C. Chelex 100 resin (Bio-Rad Laboratories, Inc., Hercules,CA, USA) was added to each sample and incubated for 1 h,after which the supernatant was removed. DNA was extracted using phenol-chloroform, concentrated using ethanol precipitation, and resuspended in Tris-EDTA (1 mM EDTA and 10 mM Tris hydrochloride; pH 8.0).
The DNA samples extracted from tissues were then subjected to PCR analysis to explore the BRAFV600Emutation.The appropriate primers have been described in previous research33. PCR cycles were performed using the BigDye Terminator sequencing kit (Applied Biosystems, Foster City,CA, USA) and the sequencing products were analyzed with an ABI PRISM 310 Genetic Analyzer (Applied Biosystems).
Statistical analysis
SPSS 22.0 software (IBM Corp., Version 22.0, Armonk, NY,USA) was used to analyze the data. Data were presented as mean ± standard deviation. The χ2test or Fisher's exact test was used to compare cervical LNM and BRAFV600Emutation status with clinicopathologic features. We performed multivariate logistic regression analysis to assess independent risk factors for cervical LNM, using the factors screened by univariate analysis, with P < 0.05. We employed receiver operating characteristic curve (ROC) analysis to determine the optimal cutoff point of primary tumor size for determining the risk of CLNM. Values of P < 0.05 were considered statistically significant.
Results
Patient characteristics
There were 1,587 patients with PTMC, consisting of 1,251(78.8%) women and 336 (21.2%) men. The mean age was 45.7 (11 to 73) years, and 333 (21.0%) patients were diagnosed with Hashimoto's thyroiditis.
The mean size of primary tumors in the largest diameter was 5.9 ± 2.5 mm, with 586 (36.9%) tumors larger than 6 mm and 1,001 (63.1%) tumors smaller than or equal to 6 mm in diameter. Among all patients, 1,039 (65.5%) and 573(36.1%) demonstrated extrathyroidal extension and multifocal lesions, respectively. Considering solitary lesions,312 (30.8%) were in the upper third of the lobe, 268 (26.4%)were in the middle third, 407 (40.1%) were in the lower third, and 27 (2.7%) were in the isthmus.
CLNM occurred in 491 (30.9%) of the 1,587 patients,while LLNM was found in 73 (4.6%). Skip metastases,meaning LLNM without CLNM, were observed in 19 patients (1.2%). Table 2 shows the clinical and pathologic characteristics of these patients.
Risk factors for CLNM
ROC curve analysis showed that primary tumor size of 6 mm was the optimal cutoff point to distinguish between patients with and without CLNM (area = 0.649, standard error =0.015, asymptotic significance = 0.000, 95% confidence interval = 0.620-0.678).
Risk factors for CLNM were evaluated by univariate and multivariate analyses according to final pathological results.In univariate analysis, male gender, age < 45 years, primary tumor size greater than 6 mm, multifocality, bilateralism, and extrathyroidal extension (P < 0.01) were significantly related to CLNM. Moreover, univariate analysis performed for the solitary primary tumor group showed that CLNM was significantly associated with tumor location (P < 0.05);tumors located in the lower third and isthmus conferred a higher risk of CLNM than did those in the upper third. On multivariate analysis, male gender [odds ratio (OR) = 1.845,P = 0.000], age < 45 (OR = 1.606, P = 0.000), tumor size greater than 6 mm (OR = 2.137, P = 0.000), bilateralism(OR = 2.011, P = 0.000), and extrathyroidal extension (OR =1.555, P = 0.001) were independent risk factors for CLNM,and number of primary tumors was not significantly correlated with CLNM (P > 0.05) (Table 3).
Risk factors for LLNM
According to univariate analysis, tumor size greater than 6 mm, CLNM, extrathyroidal extension, multifocality,bilateralism, and tumor location (P < 0.05) were characterized as risk factors for LLNM, whereas sex, age, and Hashimoto's thyroiditis status were not significantly associated with LLNM (P > 0.05). Tumor location in the middle third of the thyroid gland conferred a high risk for LLNM. However, multivariate analysis identified only CLNM and recurrence as independent predictors for LLNM in patients who underwent follow-up for 40 to 72 months(Table 4).
Correlation of clinicopathologic characteristics and BRAFV600E mutation
Among the 1,587 patients, BRAFV600Emutation was detected in 299 patients with a frequency of 83.3% (249/299).Univariate analysis showed that CLNM, LLNM,multifocality, and extrathyroidal extension were not significantly associated with BRAFV600Emutation. Among patients who underwent follow-up for 40 to 72 months,recurrence was not significantly associated with BRAFV600E(Table 5).
Complications, follow-up, and recurrence
Recurrent laryngeal nerve injury occurred in 14 patients(0.9%); among these, owing to direct tumor invasion, 8 patients underwent shaving procedures or intentional resection of the recurrent laryngeal nerve resulting in permanent vocal fold paralysis, while the injury in the other 6 patients was temporary. Of the 1,587 patients, 386 (24.3%)suffered postoperative hypocalcemia requiring calcium supplementation, and 4 (0.3%) experienced permanent hypocalcemia. Four patients developed a postoperative chylous fistula, and 1 patient required reoperation on the same day owing to postoperative bleeding.

Table 2 Characteristics of patients
Postsurgical clinical examinations were performed every 6 months; these included cervical US and serum thyroidstimulating hormone and thyroglobulin levels. The mean follow-up duration was 56 months (range, 40-72 months),and 121 patients were lost to follow-up. During the follow-up period, 16 patients experienced recurrence in the central cervical compartment. Among 88 patients who had undergone lateral neck dissection, 3 patients (0.19%) suffered from LLNM: 2 and 1 experienced ipsilateral and contralateral neck recurrence, respectively. Among patients without LLNM at the time of initial treatment, 7 patients (0.44%)suffered regional recurrence: ipsilateral neck recurrence wasfound in 4 patients, contralateral neck recurrence in 1, and bilateral neck recurrence in 2. Regional recurrence was frequent at levels III, IV, and II. Among 1,209 patients who did not undergo total thyroidectomy, 12 (0.99%)experienced malignant recurrence in the contralateral lobe.At the data cutoff point, no patient demonstrated distant metastasis. During the follow-up period, 2 patients died from adrenal insufficiency and pneumonia, and another died of heart failure. None of the patients died of PTMC.

Table 3 Univariate and multivariate logistic regression for CLNM
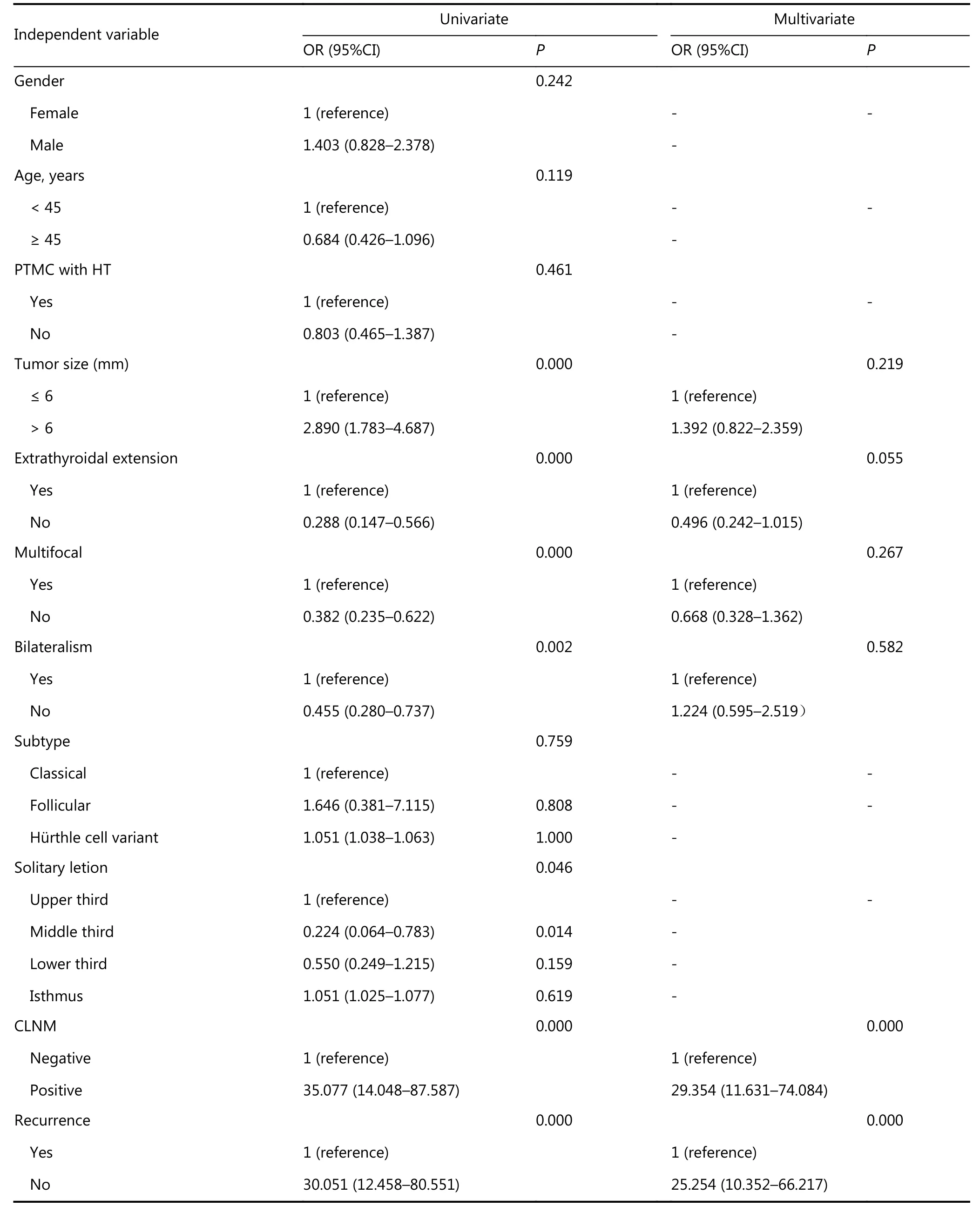
Table 4 Univariate and multivariate logistic regression for LLNM

Table 5 Correlation between clinicopathological characteristics and BRAFV600E mutation in PTMC
Discussion
In this retrospective study, we evaluated the risk factors for CLNM and LLNM in 1,587 patients with PTMC. In previous reports, the prevalence of CLNM ranged from 24.1% to 64.1%2-5, and that for LLNM ranged from 3.7% to 44.5%2. In the present study, the prevalence of CLNM and LLNM was 30.9% (491 of 1,587) and 4.6% (73 of 1,587), respectively.There were 19 patients (19 of 73) with skip metastases,meaning LLNM without CLNM.
In the present study, we used univariate and multivariate logistic regression analyses to evaluate risk factors for cervical LNM. Consistent with the results of previous reports, we found that male gender, age less than 45 years, extrathyroidal extension, and bilateralism were independent risk factors for CLNM14-18. Multifocality was not an independent predictor of CLNM, although significance was demonstrated on univariate analysis.
Tumor size is considered to be an essential prognostic factor in patients with PTMC19. Although the majority of previous studies used a tumor size of 5 mm as the size threshold20-23, we assessed thresholds greater than 4 mm,5 mm, 6 mm, 7 mm, and 8 mm by ROC curve analysis, and found that primary tumor size (> 6 mm) was significantly correlated with CLNM. Extrathyroidal extension was an evaluated risk factor for CLNM22,24. However, the diagnosis of extrathyroidal extension is subjective and controversial as there is not a well-defined true capsule in the thyroid gland.The thyroid capsule is usually made up of inconspicuous thin fibrous tissues and contains a variable amount of skeletal muscle, blood vessels, and adipose tissue. In the present study, most cases of PTMC with extrathyroidal extension exhibited extension to the perithyroid soft tissue, such as adipose tissue, rather than to the sternothyroid muscle. In this study, 1,039 (65.5%) patients showed extrathyroidal extension, as we selected intrathyroidal areas with low-risk thyroid carcinoma for observation rather than surgery.
Furthermore, the present study showed that tumor size greater than 6 mm, extrathyroidal extension, multifocality,bilateralism, and CLNM were statistically significant factors for LLNM, and CLNM was an independent risk factor.Although CLNM is not significantly associated with diseasefree survival in PTMC25-27, this outcome can be strongly associated with LLNM.
The connection between tumor location and LNM in patients with PTMC remains controversial. Wada et al.28first reported that the location of PTMC may be related to CLNM and LLNM, although the differences were not statistically significant. Xiang et al.29found a correlation between PTMC located in the middle third of the thyroid gland with both CLNM and LLNM. In contrast, Zhang et al.14showed that location of PTMC in the upper third of the thyroid conferred a lower risk for CLNM and a higher risk for LLNM. In the present study, we found that tumor location in the lower third of the thyroid gland and the isthmus was strongly associated with CLNM, whereas tumor location in the middle third was correlated with LLNM.
The BRAFV600Emutation, which occurs in about 29%-60%of PTC, has been identified as the most common genetic change in PTC30,31. These mutations activate the RAS/RAF/mitogen-activated protein kinase pathway and cause the malignant proliferation of cells32. Previous observations have indicated that the BRAFV600Emutation is correlated with highly aggressive factors, such as advanced stage of disease, extrathyroidal extension, and nodal metastasis in PTC33-35. The BRAFV600Emutational status of highly aggressive PTMC was analyzed by Lee et al.32who discovered that the rate of BRAFV600Emutation in patients with penetration of the capsule was higher than the rate in those without. The authors also found that mutations occurred in 50% of T3 or T4 stage tumors, meaning that the presence of BRAFV600Emutation can predict the existence of extrathyroidal metastasis. Moreover, the BRAFV600Emutation was discovered more commonly in highly aggressive subtypes, such as tall cell PTMC, indicating that BRAFV600Emutational status is significantly associated with poor tumor behavior. BRAFV600Eis also observed in PTMC, and the mutation may thus be an early event in tumor development,perhaps facilitating the acquisition of secondary genetic events through induction of genomic instability. However,unlike the findings of previous studies, Sun et al.8observed that BRAFV600Emutation displayed a weakly negative association with PTMC neck and distant metastasis in a group of 101 patients. In the present study, we were unable to identify a significant correlation between BRAFV600Emutation and clinicopathologic characteristics such as multifocality, neck metastasis, and extrathyroidal extension.Accordingly, it seems that BRAFV600Emutation is not a prognostic factor for PTMC. In fact, most patients with PTMC have an extremely good prognosis following surgery.Large numbers of patients undergo very long-term followup, and it will be necessary to identify the clinical relevance of the BRAFV600Emutation in PTMC. Despite the restrictions of the current study, our data also suggest that larger studies are warranted to determine the relationships between the BRAFV600Emutation and clinical characteristics in patients with PTMC.
Although we analyzed a cohort of 1,587 patients with PTMC, there are nonetheless still several limitations in the present study. First, the incidence of LLNM was relatively low in our research sample, and patients who did not undergo LLND were regarded as negative. However, prophylactic LLND could only be performed in cases of LLNM proven by FNAB or with clinical suspicion on US. In fact, prophylactic LLDN is not recommended in the American Thyroid Association guidelines. Nevertheless, data based on prophylactic LLND are more accurate and meaningful. In PTMC, however, the complications of LLND cannot be weighed against its questionable effect on recurrence and survival. Second, long-term follow-up was not performed in the current study. Third, the BRAFV600Emutation analyses were performed in a relatively small number of patients(299); therefore, the rate of BRAFV600Emutation may be underestimated, leading to the absence of a significant correlation between BRAFV600Emutation and aggressive factors.
Conclusions
In conclusion, the present study showed that male sex, age less than 45 years, tumor size larger than 6 mm, presence of bilateralism, and extrathyroidal extension were all independent risk factors for CLNM. Moreover, larger primary tumor, extrathyroidal extension, multifocality,bilateralism, and CLNM were factors that conferred an increased risk of LLNM. Notably, the location of the tumor had an important association with cervical lymph node metastasis status in patients with a solitary primary tumor.Specifically, PTMC location in the lower third of the thyroid gland and the isthmus was associated with a higher risk of CLNM, and PTMC location in the middle third correlated with LLNM. In our studies including 299 patients, BRAFV600Emutation was not significantly associated with prognostic factors in patients with PTMC.
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (Grant No. 81402392,81472580, 81502322) and Tianjin Municipal Science and technology project (Grant No. 15JCQNJC12800 and 17YFZCSY00690).
Conflict of interest statement
No potential conflicts of interest are disclosed.
 Cancer Biology & Medicine2019年1期
Cancer Biology & Medicine2019年1期
- Cancer Biology & Medicine的其它文章
- Application of next-generation sequencing technology to precision medicine in cancer: joint consensus of the Tumor Biomarker Committee of the Chinese Society of Clinical Oncology
- Methods of computed tomography screening and management of lung cancer in Tianjin: design of a population-based cohort study
- Reactive capillary hemangiomas: a novel dermatologic toxicity following anti-PD-1 treatment with SHR-1210
- Perioperative rh-endostatin with chemotherapy improves the survival of conventional osteosarcoma patients: a prospective non-randomized controlled study
- 68Gallium-labelled PSMA-PET/CT as a diagnostic and clinical decision-making tool in Asian prostate cancer patients following prostatectomy
- Identification of portal vein tumor thrombus with an independent clonal origin in hepatocellular carcinoma via multi-omics data analysis
