肺部超声评分在急性呼吸窘迫综合征患者早期病情评估中应用
张磊 陶洋 姚丽娜 周成杰 安敏飞 俞万钧 陈国忠


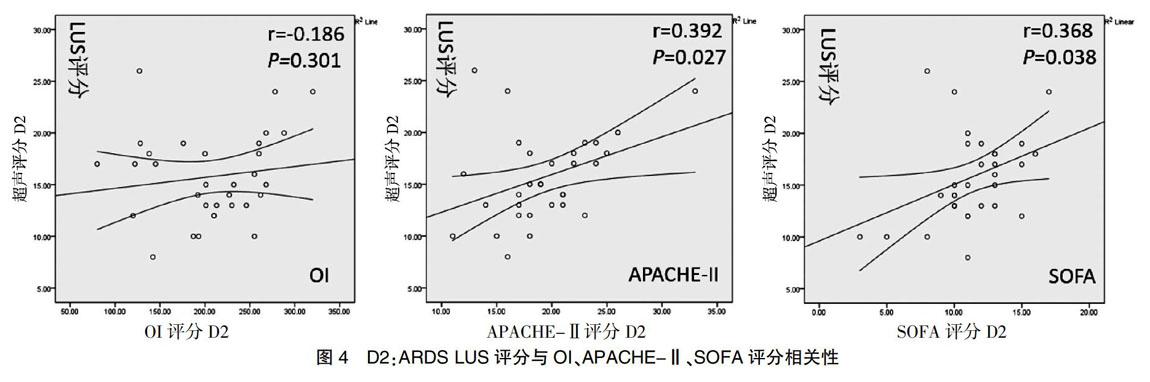
[摘要] 目的 探討肺部超声(lung utrasonography,LUS)评分在急性呼吸窘迫综合征(acute respiratory distress syndrome,ARDS)患者早期病情评估中的价值。 方法 选取2016年7月~2018年1月入住鄞州医院ICU和EICU且符合柏林标准诊断的ARDS患者,根据氧合指数(oxygenation index,OI)将ARDS患者分为轻中度组(100 mmHg [关键词] 肺部超声;急性呼吸窘迫综合征;氧合指数;血管外肺水 [中图分类号] R563.9 [文献标识码] A [文章编号] 1673-9701(2019)01-0028-05 Application of lung utrasonography score in early disease assessment of patients with acute respiratory distress syndrome ZHANG Lei1 TAO Yang2 YAO Li'na1 ZHOU Chengjie1 AN Minfei1 YU Wanjun3 CHEN Guozhong1 1.ICU, Yinzhou Hospital Affiliated to Ningbo University Medical College, Ningbo 315040, China; 2.Rome of Clinical Record, Yinzhou Hospital Affiliated to Ningbo University Medical College, Ningbo 315040, China; 3.Department of Respiratory, Yinzhou Hospital Affiliated to Ningbo University Medical College, Ningbo 315040, China [Abstract] Objective To investigate the value of lung utrasonography(LUS) score in the early assessment of patients with acute respiratory distress syndrome(ARDS). Methods Patients who were admitted to the Yinzhou Hospital ICU and EICU from July 2016 to January 2018 and who met the Berlin criteria for diagnosis of ARDS were selected. Patients with ARDS were divided into mild to moderate group(100 mmHg<OI≤300 mmHg) and severe group(OI≤100 mmHg) according to oxygenation index (OI). The patient's clinical data and the LUS score and OI, acute physiology and chronic health evaluation Ⅱ(APACHE-Ⅱ), and sequential organ failure assessment (SOFA) at the first day (D1), the second day (D2), and the third day (D3) were recorded, and the correlation between LUS score and OI, APACHE-Ⅱ, and SOFA scores was analyzed by Pearson correlation analysis. The LUS score was analyzed by ROC curve to determine the severity, sensitivity and specificity of patients with ARDS. Results 33 patients with ARDS were collected and 3 patients died in 72 hours. On D1, the LUS score was negatively correlated with OI (r=-0.419, P=0.015), positively correlated with APACHE-Ⅱ score (r=0.414, P=0.017), and positively correlated with SOFA score (r=0.477, P=0.005), and the correlation was close. On D2 and D3, the LUS score still had a good positive correlation with the APACHE-Ⅱ score and the SOFA score (r values on D2 were: 0.392, 0.368, P values were 0.027, 0.038, respectively; r values on D3 were: 0.466, 0.390, P values were 0.010, 0.033, respectively). The area under the ROC curve of the LUS score(AUC=0.933) was analyzed and the sensitivity of severe ARDS was 89% and the specificity was 79% with a threshold of 20.5. Conclusion The LUS score can well reflect the change of lung tissue with loss of air and the deficiency of lung ventilation area in patients with ARDS, and it has good reliability and stability, which can be used to assess the severity of ARDS. [Key words] Lung utrasonography; Acute respiratory distress syndrome; Oxygenation index; Extravascular lung edema ARDS指各种肺内、外因素导致的弥漫性肺泡损伤及肺部炎症进而发展为急性呼吸衰竭。文献报道提示ARDS总体病死率在36%~50%[1,2],其预后与早期原发病治疗和疾病严重程度明显相关。Joyner等[3]首次应用LUS获取病理状态下肺组织图像。研究者[4,5]发现LUS在胸腔积液、肺实变/肺不张、肺水肿、气胸诊断敏感性和特异性比传统X线胸片具有明显优势,与胸部CT相似,可作为CT的替代检查方法用于ARDS的诊断。ARDS病情变化快,复杂棘手,死亡率高,患者存活的关键在于早期积极治疗干预。本研究采用连续动态方式探讨LUS评分在ARDS患者早期病情评估中的应用价值从而反馈临床医师,对ARDS疾病进行早期干预、改善患者预后具有积极的临床意义。 1 资料与方法 1.1 一般资料 收集2016年7月~2018年1月期间入住我院ICU、EICU符合柏林定义ARDS成年患者33例,平均年龄(71.27±14.70)岁,男22例,占67%,3 d内死亡3例。轻中度组(100 mmHg<OI≤300 mmHg)24例、重度组(OI≤100 mmHg)9例,其中72 h内轻中度组存活22例,重度组存活6例。排除标准主要包括严重心力衰竭、急性冠脉综合征、严重的心脏瓣膜病、肺间质性病变患者及不适宜或拒绝超声检查患者。 本项研究根据氧合指数将患者分为轻中度组(100 mmHg<OI≤300 mmHg)和重度组(OI≤100 mmHg),进一步比较两組患者基本临床特征的差异,见表1。患者年龄、性别、左室射血分数的组间差异无统计学意义。病因构成上,重症肺炎和感染性休克是导致ARDS的主要原发病,分别占45.5%、33.3%。此外,随着患者ARDS病情进展,入住ICU时间及死亡率逐渐增高,组间差异均有统计学意义(P<0.05)。 1.2 研究内容 所有患者给予6 mL/kg小潮气量通气,根据氧合状态调整机械通气参数,行GEM Premier 300动脉血气分析等相关检查。检查前给予100%氧浓度吸入30 min,CT检查前30 min内进行肺部超声检查,并在心尖四腔心切面获得左心室射血分数(left ventricular ejection fraction,LVEF),并完成APACHE-Ⅱ、SOFA评分及OI。此后大致相同条件相同时间段进行D2、D3 LUS评分及APACHE-Ⅱ评分、SOFA评分及OI。 1.3 APACHE-Ⅱ、SOFA评分、LUS评分 APACHE-II评分为急性生理学与慢性健康状况评分系统,评估内容包括体温、血压、血肌酐水平等17项急性生理学评分、年龄评分、慢性健康状况评分,三项评分总分值即为APACHE-Ⅱ评分值,最高分值为71分,分值越高,表示病情越严重,预后越差,病死率越高[6,7];SOFA评分为序贯器官衰竭评分,由呼吸功能、凝血功能、肝功能、心血管功能、神经功能及肾脏功能构成,每项评分0~4分,总分为24分,分值越高,预后越差[8-10];LUS评分为肺部超声评分,最早在Soummer等[11]研究中提出,其研究表明分值越大,患者呼吸窘迫发生率越高,拔管失败的风险越高。目前LUS已经有多种评分方法,本项研究采用Monastesse[12]评分方法,将患者胸部分为12个分区,每个分区分值总和即为肺部超声评分值,最高分值为36分,分值越高,表示病情越严重,预后越差。 1.4 检查方法 采用SonoSite S Series S-ICUTM型号医用彩色超声仪,搭载探头SonoSite P21 1~5 MHz和SonoSite HFL 38 6~13 MHz,P21探头主要用于肺部超声检查及心脏检查,HFL38探头主要用于观察胸膜线情况。采用图1所示方法,整个胸部分为12个分区。扫查每个分区以肺部LUS评分标准最高值作为记录值,记录每个肺部分区分值,12个分区分值总和即为肺部超声评分值,分值在0~36分之间,最小值0分代表正常肺组织通气;最高分值36分,代表肺组织严重实变。患者检查时间控制在5 min以内,肺部超声检查医师均为同一个医师,且对患者临床资料不知情。 肺部超声评分标准[11,12]:单个肺部超声切面出现水平A线或两侧胸壁B线≤2条,代表正常肺组织通气区(图2A),计0分;单个肺部超声切面出现多发典型B7线,代表中度肺组织通气减少区(图2B),计1分;单个肺部超声切面出现多发融合B3线,代表重度肺组织通气减少区(图2C),计2分;单个肺部超声切面出现肺叶实变,代表肺组织严重的失气化(图2D),计3分(图2)。 1.5 统计学方法 采用SPSS18.0统计软件对数据进行统计学分析,计量资料以均数±标准差(x±s)表示,计数资料用χ2检验。组间比较使用t检验。Pearson相关系数分析D1、D2、D3 LUS评分与OI、APACHE-Ⅱ评分、SOFA评分之间的相关性;绘制ROC曲线计算出LUS评分在轻中度组和重度组之间的界值,预测重度组敏感性和特异性。P<0.05表示差异具有统计学意义。 2 结果 2.1 LUS评分与OI、APACHE-Ⅱ评分、SOFA评分相关性 采用spearson相关分析D1、D2、D3 LUS评分与之对应D1、D2、D3 OI、APACHE-Ⅱ评分、SOFA评分之间的相关性,结果发现LUS评分与D1时OI负相关(r=-0.419,P=0.015),与APACHE-Ⅱ评分、SOFA评分正相关(r值分别为:0.414、0.477,P值分别为0.017、0.005);D2、D3时,LUS评分与APACHE-Ⅱ评分、SOFA评分依然具有较好的正相关性(D2 r值分别为0.392、0.368,P值分别为0.027、0.038;D3 r值分别为0.466、0.390,P值分别为:0.010、0.033)。见图3~5。 2.2 LUS评分评估ARDS严重程度价值 通过LUS评分ROC曲线下面积(AUC)分析得到,当LUS评分值≥20.5时提示患者病情严重,需警惕死亡发生,预测重度组敏感度为89%,特异度为79%。见图6。 3 讨论 目前ARDS诊断主要依靠临床表现及胸部影像学改变,胸部CT被认为是“金标准”[13],但存在转运风险,重复性差,辐射损伤,床边胸片检查可避免转运风险,但影像分辨率差,病情反映滞后。LUS在ARDS应用中具有明显优势[14,15],表现间质综合征[16],可以通过B线进行半定量评估[17];其次LUS属无创检查技术,重复性强,特别是当前ARDS没有特异性高的生物学标记物来监测病情的情况下,LUS或许是合适的方式。 ARDS时血管外肺水含量(extravascular lung water,EVLW)增加,可通过脉搏指示连续心输出量监测技术(pulse-indicated continuous cardiac output,PICCO)客观地监测EVLW评估患者病情。PICCO监测技术属于有创检查,费用昂贵,不能常规开展。研究发现LUS评分与PICCO-EVLW呈明显的正相关性,可以用来评估ARDS患者病情严重程[17-19],这与Bataille等[17]研究结果相符,与PICCO相比具有明显优势;Ma等[20]研究发现ARDS患者LUS评分与胸部CT图像表现存在很强的相关性,因此LUS评分评估ARDS患者病情提供了可行性。 探讨D1、D2、D3 LUS评分与传统信度较好的临床评分[19,21]如APACHE-Ⅱ评分、SOFA评分及OI进行相关性分析发现,D1时LUS评分与它们都具有較高的相关性,与OI呈负相关,与APACHE-Ⅱ评分、SOFA评分呈正相关,这与之前的研究者[19,22,23]研究结论相一致;D2、D3时APACHE-Ⅱ评分、SOFA评分依旧呈较好的正相关,说明LUS评分可以早期评估ARDS病情。目前LUS评分尚不统一,Bataille等[17]把胸部分为4个肺区,最高值为20分,超过11分为重度ARDS,随着评分值的增加病情越严重,研究提示LUS评分可以反映ARDS患者病情严重程度。Santos等[22]把胸部分为6个肺区,最高分为24分;Volipicelli等[14]把胸部分为8区,而此项研究采用Monastesse等[12]把胸部分为12个分区,总分值为36分,根据ARDS肺内病变特征,选择这种评分方式比上述评分方法更全面更合理,更充分的反映患者肺部病情。本研究显示LUS评分提示重度ARDS阈值为20.5,预测重度的敏感性为89%,特异度为75%,当LUS评分>20.5时,患者死亡风险明显增高,这与Zhao等[19]研究结果相符。 肺部超声具有可重复、易操作无创快捷、无辐射损伤、经济廉价及患者家属接受度高等诸多优点,且肺部超声评分可以很好地反映ARDS患者肺组织失气化改变及肺通气面积的缺失;LUS评分与氧合指数呈较明显的负相关,与APACHE-Ⅱ评分、SOFA评分、LIS评分、MODS评分呈较好的正相关,特别在早期相关性更强,且具有一定的信度和稳定性。肺部超声评分可在临床中用来评估ARDS患者病情严重程度,预测重度敏感性为89%,特异度为79%,特别是在疾病早期优势明显。当LUS评分超过20.5时,提示重度ARDS,死亡风险极高。 [参考文献] [1] Afshari A,Brok J,Moller AM,et al. Inhaled nitric oxide for acute respiratory distress syndrome and acute lung injury in adults and children:A systematic review with meta-analysis and trial sequential analysis[J]. Anesth Analg,2011,112(6):1411-1421. [2] Bellani G,Laffey JG,Pham T,et al.Epidemiology,patterns of care,and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries[J]. JAMA,2016,315(8):788-800. [3] Joyner CR Jr.,Herman RJ,Reid JM.Reflected ultrasound in the detection and localization of pleural effusion[J].JAMA,1967,200(5):399-402. [4] Ashton-Cleary DT. Is thoracic ultrasound a viable alternative to conventional imaging in the critical care setting?[J].Br J Anaesth,2013,111(2):152-160. [5] Copetti R,Soldati G,Copetti P.Chest sonography:A useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome[J]. Cardiovasc Ultrasound,2008,6:16. [6] 黎耀俊,李国明,林惠文.慢性阻塞性肺疾病急性发展期的临床特征与APACHEⅡ评分的关系[J].中国现代医生, 2009,47(21):87-88. [7] Knaus WA,Draper EA,Wagner DP,et al.APACHEⅡ:A severity of disease classification system[J]. Crit Care Med,1985,13(10):818-829. [8] Fullerton JN,Thompson K,Shetty A,et al. New sepsis definition changes incidence of sepsis in the intensive care unit[J].Crit Care Resusc,2017,19(1):9-13. [9] Siddiqui S,Chua M,Kumaresh V,et al.A comparison of pre ICU admission SIRS,EWS and q SOFA scores for predicting mortality and length of stay in ICU[J].J Crit Care,2017,41:191-193. [10] Vincent JL,Moreno R,Takala J,et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure.On behalf of the working group on sepsis-related problems of the european society of intensive care medicine[J].Intensive Care Med,1996,22(7):707-710. [11] Soummer A,Perbet S,Brisson H,et al. Ultrasound assessment of lung aeration loss during a successful weaning trial predicts postextubation distress[J].Crit Care Med,2012,40(7):2064-2072. [12] Monastesse A,Girard F,Massicotte N,et al. Lung ultrasonography for the assessment of perioperative atelectasis:A pilot feasibility study[J].Anesth Analg,2017,124(2):494-504. [13] Mazzei MA,Guerrini S,Cioffi Squitieri N,et al.Role of computed tomography in the diagnosis of acute lung injury/acute respiratory distress syndrome[J].Recenti Prog Med,2012,103(11):459-464. [14] Volpicelli G,Elbarbary M,Blaivas M,et al. International evidence-based recommendations for point-of-care lung ultrasound[J].Intensive Care Med,2012,38(4):577-591. [15] Volpicelli G.Point of care lung ultrasound[J]. Praxis,2014, 103(12):711-716. [16] 張磊,俞万钧,马坚.超声在肺部疾病中的临床应用[J].中国医学影像技术,2017,33(4):611. [17] Bataille B,Rao G,Cocquet P,et al. Accuracy of ultrasound B-lines score and E/Ea ratio to estimate extravascular lung water and its variations in patients with acute respiratory distress syndrome[J]. J Clin Monit Comput,2015, 29(1):169-176. [18] 王敏佳,龚仕金,严静,等.肺部超声B线数目与血管外肺水的相关性分析[J].浙江医学,2016,38(2):109-111. [19] Zhao Z,Jiang L,Xi X,et al. Prognostic value of extravascular lung water assessed with lung ultrasound score by chest sonography in patients with acute respiratory distress syndrome[J].BMC Pulm Med, 2015,15:98. [20] Ma H,Huang D,Guo L,et al. Strong correlation between lung ultrasound and chest computerized tomography imaging for the detection of acute lung injury/acute respiratory distress syndrome in rats[J]. J Thorac Dis,2016, 8(7):1443-1448. [21] Macdonald SP,Arendts G,Fatovich DM,et al. Comparison of PIRO, SOFA, and MEDS scores for predicting mortality in emergency department patients with severe sepsis and septic shock[J]. Acad Emerg Med,2014,21(11):1257-1263. [22] Santos TM,Franci D,Coutinho CM,et al. A simplified ultrasound-based edema score to assess lung injury and clinical severity in septic patients[J]. Am J Emerg Med,2013,31(12):1656-1660. [23] Li L,Yang Q,Li L,et al. The value of lung ultrasound score on evaluating clinical severity and prognosis in patients with acute respiratory distress syndrome[J]. Zhong-hua Wei Zhong Bing Ji Jiu Yi Xue,2015,27(7):579-584.

