Neural-like cells from adipose-derived stem cells for cavernous nerve injury in rats
Cheng-Cheng Ying , Mei Yang , Yong Wang Yong-Lian Guo , Wan-Li Hu, Xin-Min Zheng
1 Department of Urology, the Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology, Wuhan,Hubei Province, China
2 Department of Endocrinology, Tongren Hospital of Wuhan University (Wuhan Third Hospital), Wuhan, Hubei Province, China
3 Department of Urology, Zhongnan Hospital of Wuhan University, Wuhan, Hubei Province, China
Abstract Although the remaining nerve tissue can regenerate and partly restore erectile function when the cavernous nerve is compressed/severed and function lost, the limited regenerative ability of these nerve tissues often fails to meet clinical needs. Adipose-derived stem cells are easy to obtain and culture, and can differentiate into neural cells. Their proliferation rate is easy to control and they may be used to help restore injured cavernous nerve function. Sprague-Dawley male rats (n = 45) were equally randomized into three groups: fifteen rats as a sham-operated group, fifteen rats as a bilateral nerve crush (BINC) group (with no further intervention), fifteen rats as a BINC with intracavernous injection of one million neural-like cells from adipose-derived stem cells (NAS) (BINC + NAS) group. After 4 weeks, erectile function was assessed by stimulating the cavernous body. The number of myelinated axons in the dorsal cavernous nerve was determined by toluidine blue staining. The area of neuronal nitric oxide synthase-positive fibers in the dorsal penile nerve was measured by immunohistochemical staining. Masson staining was used to analyze the ratio of smooth muscle to collagen in penile tissue. The results demonstrate that maximal intracavernous pressure, the ratio of maximal intracavernous pressure to mean arterial pressure, the numbers of myelinated axons and neuronal nitric oxide synthase-positive fibers in the dorsal penile nerve, and the ratio of smooth muscle to collagen could be increased after cell transplantation. These findings indicate that neural-like cells from adipose-derived stem cells can effectively alleviate cavernous nerve injury and improve erectile function. All animal experiments were approved by the Animal Ethics Committee of Huazhong University of Science and Technology, China (approval No. 2017-1925) on September 15, 2017.
Key Words: nerve regeneration; adipose-derived neural stem cells; corpus cavernosum; cavernous nerve; erectile dysfunction; radical prostatectomy;neurons; cell differentiation; neural regeneration
Introduction
Long-term oncologic results show that the gold standard treatment for prostate cancer is radical prostatectomy(Heidenreich et al., 2011). However, during this procedure, cavernous nerves, which run the posterolateral area of prostates, are easily injured. To reduce the incidence of erectile dysfunction after radical prostatectomy, Walsh et al. (1987) developed a nerve-sparing technique. However,despite the advantages of laparoscopic and robot-assisted surgery nerve-sparing techniques, erectile dysfunction still affects a remarkable proportion of radical prostatectomy patients (Dubbelman et al., 2006; Walz et al., 2010), as cavernous nerves may still be inadvertently damaged during nerve-sparing prostatectomy. When cavernous nerves have been crushed or cut, and nerve function is lost, distal injured cavernous nerves degenerate and die. However, proximal cavernous nerves may be able to regenerate and re-establish function, while the injured part dies and degenerates after such an injury. Although nerve regeneration from remaining neural tissues could restore erectile function (Carrier et al., 1995), the capacity of nervous system regeneration after injury is still a challenging area of investigation.
Adipose-derived stem cells (ADSCs) are easy to obtain and culture, and could promote neuronal regeneration by various growth factors after cavernous nerve injury (Fansa and Keilhoff, 2003; Sun et al., 2003). Studies have also shown that both in vivo and in vitro ADSCs can be induced to differentiate into neural cells (Jang et al., 2010; Zarei et al., 2016; Zheng et al., 2017; Fernandes et al., 2018; Makdissy et al., 2018;Zhong et al., 2018; Kato et al., 2019). Neuronal differentiation of implanted ADSCs that protect cells against intracerebral hemorrhage-induced apoptosis might improve neurological function (Chen et al., 2012). Many investigations have shown that intracavernous injection of ADSCs or autologous adipose-derived stem vascular fractions exert proerectile effects after cavernous nerve injury (Albersen et al., 2010; Lin et al.,2011; Zhang et al., 2011; Chen et al., 2017).
In this study, we aimed to isolate ADSCs from Sprague-Dawley rats and induce them to differentiate into neural cells. We then assessed whether intracavernous injection of neural-like cells from ADSCs (NAS) could improve erectile function and promote nerve regeneration in rat models of cavernous nerve injury.
Materials and Methods
Animals
Forty- five specific-pathogen-free male Sprague-Dawley rats aged 3 months were purchased from the Center for Experimental Animal of Medical College of Wuhan University in China (animal license No. SCXK (E) 2008-0004). All animal experiments were approved by the Animal Ethics Committee of Huazhong University of Science and Technology,China (approval No. 2017-1925) on September 15, 2017.
Establishment and treatment of rat models of cavernous nerve injury
The rats were randomized into three groups: sham-operated group, bilateral cavernous nerve-crush injury (BINC) group,and BINC + NAS group (n = 15 each). The sham-operated group received a sham operation comprising a midline incision and identification of the cavernous nerves bilaterally without further surgical manipulation. The cavernous nerve crush model was established as detailed elsewhere (Zhao et al., 2016). After the rats were anesthetized, body temperature was maintained isothermically with a heating pad at 37°C. A midline abdominal incision was made to expose the bladder and prostate. The bilateral major pelvic ganglion was dissected from the lateral areas of the prostate with the aid of a surgical microscope (SXP-1C, Medical Optical Instruments Factory of Shanghai Medical Instruments Co.,Ltd., Shanghai, China). From the bilateral major pelvic ganglion, cavernous nerves were identified towards the corpus cavernosum. The BINC and BINC + NAS groups underwent BINC using a hemostat clamp (Cheng-He Microsurgical Instruments Factory, Ningbo, Zhejiang Province, China)for 2 minutes. The BINC + NAS group received immediate intracavernous injections of 100 μL NAS (approximately 1 million neural-like cells from adipose-derived stem cells in 100 μL phosphate buffered saline), while the BINC group received an immediate intracavernous injection of 100 μL phosphate buffered saline.
Preparation of NAS cells
Adipose tissue was harvested and neural differentiation conducted as described previously (Ying et al., 2012). Briefly,inguinal fat pads were collected from specific-pathogen-free Sprague-Dawley rats aged 1 month (purchased from the Center for Experimental Animal of Medical College of Wuhan University in China) under anesthesia with intraperitoneal injection of 2% sodium pentobarbital 40 mg/kg. The tissues washed using phosphate buffered saline were cut into pieces and digested with type I collagenase. Enzyme activity was neutralized with Dulbecco's modified Eagle's medium containing 10% fetal bovine serum and centrifuged at 300× g (1200 r/min) for 600 seconds to obtain a high density of cellular particles. The stem cellular particles were then digested for 2 hours in Dulbecco's modified Eagle's medium containing 10% fetal bovine serum with 5% humidified CO2at 37°C. ADSCs were examined for surface markers by flow cytometry as described previously (Ying et al., 2012). The cells were trypsinized and subcultured when they reached 90% confluence at a density of 1 × 106cells/cm2(third passage). Neurogenic differentiation was induced in ADSCs in preinduction medium (Dulbecco's modified Eagle's medium with 10% fetal bovine serum (Gibco, Carlsbad, CA, USA)10 ng/mL epithelium growth factor (PeproTech, Rocky Hill,UK), 20 ng/mL basic fibroblast growth factor (PeproTech)and 10 ng/mL brain derived neurotrophic factor (Pepro-Tech)) for 3 days. Subsequently, cells were induced in neurogenic medium (Dulbecco's modified Eagle's medium with 10% fetal bovine serum, 120 μM indomethacin, 3 μg/mL insulin, 300 μM isobutyl-methyl-xanthine (all from Sigma-Aldrich, St. Louis, MS, USA)) for 48 hours after preinduction.The cells were analyzed by immuno fluorescence staining for the expression of Beta III-tubulin (Tuj-1) and glial fibrillary acidic protein (GFAP) as previously reported (Ying et al.,2012). Solutions of 100 μL NAS (approximately 1 million neural-like cells in 0.1 mL phosphate buffered saline) were prepared.
Assessment of erectile function
Erectile function was assessed in accordance with our previous methods (Ying et al., 2013). At 4 weeks after model establishment, erectile function was assessed in all groups.In brief, after anesthesia, cavernous nerves and the major pelvic ganglion were exposed bilaterally via midline laparotomy with a 23-G needle, using 250 U/mL heparin connected to the pressure transducers. The proximal parts of cavernous nerves activated by platinum electrodes were connected to a stimulator. The stimulus parameters are 20 Hz, duration of 50 seconds, 0.2 ms pulse width and 1.5 mA. After carotid artery cannulation, mean arterial pressure (MAP) and intracavernous pressure (ICP) were recorded by a data acquisition system (Chengdu TME Technology Co., Ltd., Chengdu, China). Finally, the maximal ICP/MAP ratio was calculated. The penis and cavernous nerves were then harvested for histology.
Toluidine blue staining
Toluidine blue staining was conducted according to our previous methods (Ying et al., 2013). Briefly, 2—3 mm of cavernous nerve was obtained from the proximal part of injured cavernous nerves. The cavernous nerves were fixed in cold glutaraldehyde (3% w/v), in filtrated with the graded araldite propylene oxide mixtures, and embedded in epon812(Shell Chemical, CA, USA) after dehydrating with ethanol and 1% osmium tetroxide. Nerve segments were post fixed.The results were examined by light microscopy (Olympus BX60, Tokyo, Japan) after the embedded nerves were stained with 1% toluidine blue. A DP12 camera (Olympus) at 100×oil immersion objective was used to capture images. Images were processed with Images Pro-Plus 3.0 (MediaCybernetics,Bethesda, MD, USA). The number of myelinated axons in cavernous nerves was analyzed.
Immunohistochemical staining
Nitric oxide is the most important neurotransmitter involved in the relaxation of the smooth muscle layer in the corpus cavernosum and it is the main mediator of penile erection. In the urogenital system, neuronal nitric oxide synthase (nNOS) production of nitric oxide in cavernous nerve fibers supplying the penis is well-established as the primary stimulus for neuronally induced penile erection (Burnett and Musicki, 2005). Thus, we studied nNOS in the cavernosa of the penis of rats. Penile tissues were fixed in cold fixative solution supplemented with 0.1 M phosphate buffered saline (pH 8.0), 2% formaldehyde and 0.002% trinitrophenol for 4 hours. Tissues were transferred into 30% sucrose in 0.1 M phosphate buffered saline (pH 7.3) solution overnight.After embedding with optimal cutting temperature compound, paraffin-embedded tissues were processed for 5 μm sectioning for nNOS staining. The paraffin-embedded tissue sections were washed twice with phosphate buffered saline for 5 minutes and then incubated with horse serum (3%)/phosphate buffered saline/Triton X-100 (0.3%) for 30 minutes. The sections were incubated with mouse anti-rat nNOS(1:500) overnight at 4°C after draining excess fluid. The sections were incubated with FITC-conjugated goat anti-mouse secondary antibody (1:100) after rinsing with phosphate buff-ered saline. To analyze the content of nNOS, the total areas of the dorsal nerves and the areas of nNOS-positive fibers in the dorsal nerves were evaluated at 200× magnification.
Masson's trichrome staining
Our previous methods were used for this staining (Ying et al., 2013). Brie fly, the middle part of penile tissue was fixed in 10% formalin overnight, stored and washed at 4°C with 70%alcohol. After that, the penile tissues were cut into 5 μm paraffin-embedded sections for Masson's trichrome staining. After staining the muscle tissues were identified according to color distribution using Photoshop CS 8.0 (Adobe, San Jose, CA,USA). The muscle tissue expressed as the color red was selected after the color distributions of all images were calculated.
Statistical analysis
All data are expressed as the mean ± SD. Statistical analyses were performed using SPSS 13.0 for Windows (SPSS Inc., Chicago, IL, USA). One-way analysis of variance was used for the first analysis of our results. A Student-Newman-Keuls test was carried out if the difference was signi ficant (P < 0.05).
Results
Neural differentiation capacity of adipose-derived stem cells
After 24 hours, the primary adipose-derived stem cells adhered to the bottom of culture bottle and exhibited a heterogeneous population of spindle-shaped cell morphologically. Adipose-derived stem cells displayed changes in cellular morphology after neurogenic differentiation, which included formation of axons, dendrite-like cytoplasmic projections and shrinkage of cytoplasm, and expressed neuronal markers Tuj-1 and GFAP during neuronal differentiation in vitro (Figure 1).
Effects of NAS on nerve conduction capacity
The ICP and the ICP/MAP ratio of rats in the BINC group were decreased compared with the sham-operated group (P< 0.05). The ICP of rats in the BINC + NAS group was much higher than that in the BINC group (P < 0.05). The ICP/MAP ratio in the BINC + NAS group was higher than in the BINC group (P < 0.05), but still lower than in the sham-operated group (P < 0.05; Figure 2).
NAS increases the number of myelinated axons in the dorsal nerves of a rat model of cavernous nerve injury
The number of myelinated axons was significantly lower in the BINC group than in the sham-operated group (P < 0.05). The number of myelinated axons in the BINC + NAS group was significantly higher than in the BINC group (P < 0.05), but still less than in the sham-operated group (P < 0.05; Figure 3).
NAS increases the number of nNOS-positive nerve fibers in the penile tissue of a rat model of cavernous nerve injury
nNOS-positive nerve fibers were diffusely distributed throughout the penis, and were usually observed on the periphery of dorsal nerves of the penis. In the dorsal nerves,the number of nNOS-positive nerve fibers was decreased in the BINC group compared with the sham-operated group(P < 0.05). The number of nNOS-positive nerve fibers in the BINC + NAS group was significantly higher than in the BINC group (P < 0.05), but still less than in the sham-operated group (P < 0.05; Figure 4).
NAS increases smooth muscle in the penile tissue of a rat model of cavernous nerve injury

Figure 1 Neural differentiation capacity of ADSCs.

Figure 2 Effects of NAS on ICP and MAP in a rat model of cavernous nerve crush injury at 4 weeks after modeling.

Figure 3 Effect of NAS on the number of myelinated axons in dorsal nerves of a rat model of cavernous nerve injury.
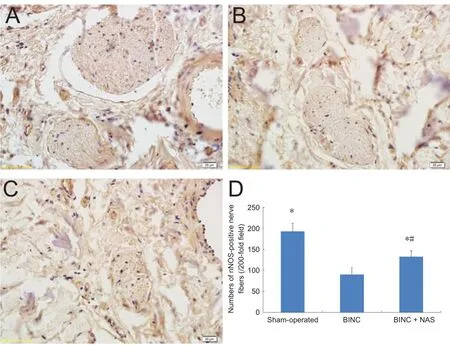
Figure 4 Effect of NAS on the number of nNOS-positive nerve fibers in the penile tissue of a rat model of cavernous nerve injury.
Computerized histomorphometric analysis showed that the ratio of smooth muscle/collagen was decreased in the BINC group compared with the sham-operated group (P < 0.05).However, the ratio of smooth muscle/collagen in the BINC+ NAS group was almost fully preserved compared with the sham-operated group (P > 0.05), and was much higher than in the BINC group (P < 0.05; Figure 5).
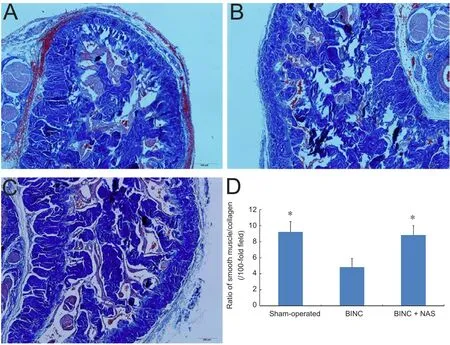
Figure 5 Effect of NAS on smooth muscle/collagen ratio in penile tissue of a rat model of cavernous nerve injury.
Discussion
This study is the first to use neural-like cells from adipose-derived stem cells to recover erectile function after cavernous nerve injury. Our present study demonstrates that NAS can remarkably enhance functional repair after cavernous nerve injury. Our ICP/MAP results and the mean maximal ICP changes showed that erectile response was much better in the BINC + NAS group than in the BINC group 4 weeks after surgery. Histologically, the number of myelinated cavernous nerve axons was greater in the BINC + NAS group than in the BINC group, directly indicating the recovery of cavernous nerves. The ratio of smooth muscle/collagen in the BINC + NAS group was almost fully preserved and much higher compared with the BINC group. nNOS-positive nerve fiber staining showed that in dorsal nerves, the number of nNOS-positive nerve fibers was increased in the BINC + NAS group compared with the BINC group.
It is reported that adipose tissue is an alternative source of multipotent mesenchymal stromal cells (Patrick, 2000).ADSCs isolated from adipose tissue can self-renew and differentiate into several cell lineages, such as cardiac myocytes,chondrocytes, myocytes, adipocytes, osteo-blasts, and endotheliocytes (Lin et al., 2009; Madonna et al., 2009; An et al.,2010; Nagasaki et al., 2011). This study demonstrated that ADSCs can be induced to differentiate neural cells in vitro,which is consistent with the reports of previous researchers(Jang et al., 2010; Chen et al., 2012). However, whether ADSCs can actually be induced to differentiate into neural cells in vivo remains challenge (Santiago et al., 2009; Zhang et al., 2009;Qian et al., 2010). Moreover, although these cells have important functions, they remain poorly understood. Bochinski et al. (2004) showed that embryonic stem cells can be induced to differentiate into neural cell lines that can improve erectile function in rat models of cavernous nerve injury when used intracavernously. Chen et al. (2012) showed that rat ADSCs,could be induced to neuronal differentiation both in vivo and in vitro. Neuronal differentiation of implanted ADSCs could protect cells against intracerebral hemorrhage-induced apoptosis, possibly improving neurological function.
Although stem cells may promote nerve regeneration by supporting axonal extension, the mechanisms of NAS cell action remain unclear. A possible mechanism may be that stem cells are capable of constitutively producing growth factors that induce neuronal growth (Lu et al., 2003). Fandel et al.(2012) demonstrated that stem cells provided an incentive for ADSC recruitment towards the major pelvic ganglion, promoting the recovery of erectile function after cavernous nerve injury. Due to the loss of axonal connectivity, the functional deficit after cavernous nerve injury may mean this mechanism is less important than the other proposed mechanisms.In the cavernous nerve fibers, nNOS production of nitric oxide, which can be supplied to the penis, is well established as a major stimulus for neuronal-induced penile erection in the genitourinary system (Burnett and Musicki, 2005). Our Masson's trichrome staining results revealed that NAS cell therapy decreased in muscle content and increased in collagen content in the BINC group compared with the sham-operated group. Histologically, the numbers of nNOS-positive nerve fibers and myelinated axons of cavernous nerves in the BINC + NAS group were greater than in the BINC group but less than in the sham-operated group. After NAS cell treatment, we could see changes in the morphological characteristics of nerve fibers in the corpora cavernosa. nNOS staining in the BINC group showed nerve fiber atrophy, beading, and attenuation compared with the sham-operated group, whereas the nNOS-positive nerve fibers of the BINC + NAS group resembled those of the sham-operated group. The protection of nerve morphology may have contributed to the improved erectile function in the BINC + NAS group.
In conclusion, intracavernous injection of NAS cells to the site of cavernous nerve injury has neuromodulatory effects on the recovery of erectile function and the regeneration of cavernous nerves. Our results suggest an effective treatment for erectile dysfunction following radical prostatectomy, and further clinical research is warranted. However, the mechanism of action of NAS cells is still unknown and this will be an area of future research.
Author contributions:Study design, preparing animal ethics and funding applications, experiment implementation, manuscript preparation and revision: CCY; animal ethics, manuscript preparation and revision, and study design: MY; peptide synthesis, study design and funding application: YW;statistical analysis: YLG; manuscript design and revision: WLH; study design,experimental implementation and manuscript revisions: XMZ. All authors reviewed and accepted the final manuscript.
Conflicts of interest:None declared.
Financial support:This study was supported by the Fundamental Research Funds for the Central Hospital of Wuhan, China, No. YB16A01 (to CCY);and the Natural Science Foundation of Hubei Province of China, No.2017CFB176 (to CCY). The funders did not participate in data collection and analysis, article writing or submission.
Institutional review board statement:The studies reported in the current manuscript were approved by the Animal Ethics Committee of Huazhong University of Science and Technology, China (approval No. 2017-1925) on September 15, 2017.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement:Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:Wenjiao Tai, University of Texas Southwestern Medical Center at Dallas, USA.
Additional file:Open peer review report 1.
- 中国神经再生研究(英文版)的其它文章
- Busting the myth: more good than harm in transgenic cells
- Comparative study of microarray and experimental data on Schwann cells in peripheral nerve degeneration and regeneration: big data analysis
- Lessons from glaucoma: rethinking the fluid-brain barriers in common neurodegenerative disorders
- Characteristics and advantages of adenoassociated virus vector-mediated gene therapy for neurodegenerative diseases
- Gene expression changes in dorsal root ganglia following peripheral nerve injury: roles in in flammation, cell death and nociception
- Nicotinamide adenine dinucleotide phosphate oxidase activation and neuronal death after ischemic stroke