Aphasia rehabilitation based on mirror neuron theory:a randomized-block-design study of neuropsychology and functional magnetic resonance imaging
Wen-Li Chen , Qian Ye , Si-Cong Zhang, Yang Xia, Xi Yang, Ti-Fei Yuan, Chun-Lei Shan, , Jian-An Li
1 Department of Rehabilitation Medicine, The First Affiliated Hospital of Nanjing Medical University, Nanjing, Jiangsu Province, China
2 Department of Rehabilitation Medicine, Zhangjiagang Hospital Affiliated to Nanjing University of Chinese Medicine, Zhangjiagang, Jiangsu Province, China
3 School of Rehabilitation Sciences, Nanjing Normal University of Special Education, Nanjing, Jiangsu Province, China
4 Yueyang Hospital of Integrated Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, China
5 Department of Rehabilitation Medicine, Zhongda Hospital, Southeast University, Nanjing, Jiangsu Province, China
6 Shanghai Key Laboratory of Psychotic Disorders, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
7 School of Rehabilitation Science, Shanghai University of Traditional Chinese Medicine, Shanghai, China
8 Institute of Rehabilitation Medicine, Shanghai Academy of Traditional Chinese Medicine, Shanghai, China
Abstract When watching someone performs an action, mirror neurons are activated in a way that is very similar to the activation that occurs when actually performing that action. Previous single-sample case studies indicate that hand-action observation training may lead to activation and remodeling of mirror neuron systems, which include important language centers, and may improve language function in aphasia patients. In this randomized-block-design experiment, we recruited 24 aphasia patients from, Zhongda Hospital, Southeast University, China. The patients were divided into three groups where they underwent hand-action observation and repetition, dynamic-object observation and repetition, or conventional speech therapy. Training took place 5 days per week, 35 minutes per day, for 2 weeks. We assessed language function via picture naming tests for objects and actions and the Western Aphasia Battery. Among the participants, one patient, his wife and four healthy student volunteers underwent functional magnetic resonance imaging to analyze changes in brain activation during hand-action observation and dynamic-object observation. Results demonstrated that, compared with dynamic-object observation, hand-action observation led to greater performance with respect to the aphasia quotient and affiliated naming sub-tests and a greater Western Aphasia Battery test score. The overall effect was similar to that of conventional aphasia training, yet hand-action observation had advantages compared with conventional training in terms of vocabulary extraction and spontaneous speech. Thus, hand-action observation appears to more strongly activate the mirror neuron system compared with dynamic-object observation. The activated areas included Broca's area, Wernicke's area, and the supramarginal gyrus. These results suggest that hand-action observation combined with repetition might better improve language function in aphasia patients compared with dynamic-object observation combined with repetition. The therapeutic mechanism of this intervention may be associated with activation of additional mirror neuron systems, and may have implications for the possible repair and remodeling of damaged nerve networks. The study protocol was approved by the Ethical Committee of Nanjing Medical University, China (approval number: 2011-SRFA-086) on March 11, 2011. This trial has been registered in the ISRCTN Registry (ISRCTN84827527).
Key Words: nerve regeneration; mirror neuron; hand-action observation; aphasia; rehabilitation; stroke; functional magnetic resonance imaging;neuropsychology; neural regeneration
Introduction
Aphasia is an acquired neurogenic language disorder caused by injury or disease in the left hemisphere (Koyuncu et al., 2016). It is a language processing disorder of speech,morphology, lexical semantics, or syntax (Zumbansen andThiel, 2014) and can disrupt communication, decrease social activity, cause depression, hinder employment, and impair quality of life (Flamand-Roze et al., 2011; Qiu et al., 2017).
The discovery and characterization of the mirror neuron system have provided a new perspective for aphasia research.Mirror neurons are a specific group of visuomotor neurons that were originally discovered in the rostral part of the ventral premotor cortex (area F5) in the macaque monkey(Gallese et al., 1996). The group of neurons were found to discharge both when the monkey grasped or manipulated an object and when the monkey observed the experimenter making similar actions (Rizzolatti et al., 2006). These neurons were named for their observation-execution matching feature(Rizzolatti et al., 1996). Neuropsychological and brain imaging studies have confirmed that similar mirror neurons also exist in the human brain. These are located in the posterior part of the inferior frontal gyrus, the ventral premotor cortex,the inferior parietal lobule, and the superior temporal cortex(Buccino et al., 2004a). The core network of mirror neurons,i.e., the mirror neuron system, are activated during execution of a particular action as well as during observation of the same action executed by another person (Buccino et al., 2001;Skipper et al., 2007). A group of neurons in F5 have been found to command grasping actions involving the mouth and hands (Fischer et al., 2008). Gentilucci et al. (1988) proposed that these neurons are involved in coding the aim of the grasp action—that is, taking possession of an object with the mouth or hand. Thus, the discharge of these “grasp” neurons is selective for the type of grasp used.
As an observation-execution matching system, the mirror neuron system is involved in action execution, imitation,and learning of motor skills (Buccino et al., 2004b). The mirror neuron system appears to constitute a necessary bridge between “doing” and “communication”, and thus plays a key role in promoting action prediction and understanding goal-directed action. In addition, the brain perceives the speech of others via automatic imitation, which instigates some of the processing that occurs while we are talking.On the basis of this internalized and embodied process, the mirror neuron system is implicated in the development of language and speech, empathy, theory of mind, and social communication (Chen and Yuan, 2008). Furthermore, the discovery of the mirror neuron system has provided new neurobiological support for the idea that language and gestures share neural substrates (Gentilucci and Dalla Volta,2008). First, from an evolutionary perspective, humans were originally silent and communicated using gestures (Rizzolatti and Arbib, 1998). The mirror neuron system enabled humans to understand the meaning of actions by inducing covert imitations of the observed gestures. In support of the idea that the hand-mouth dual-command system relies on “grasp” neurons, communication signals related to the meaning of behavior may be linked to the activity of particular articulatory organs in the mouth that were later used for speech (Gentilucci and Corballis, 2006). Considering that this unique sharing mechanism combines manual and vocal communication, many researchers have stated their support for the theory that language evolved from manual gestures as opposed to animal calls (Arbib, 2005). Second,from the view of localization of brain function, mirror neuron system may also provide the necessary bridge between action and language. The mirror neuron system regions in the dominant cerebral hemisphere, for instance, the posterior inferior frontal gyrus (Broca's area), superior temporal sulcus (Wernicke's area), and inferior parietal lobule (angular and supramarginal gyrus) all are pivotal language neural networks (Chen et al., 2012). A common phenomenon in individuals with Broca's aphasia is ideomotor apraxia, a disorder characterized by impaired execution of purposeful actions (Fazio et al., 2009). Several neuropsychological studies have supported the idea that gestures play an important role in lexical retrieval (Krauss and Hadar, 1999).For instance, speakers frequently pronounce words as they execute symbolic gestures to express the same meaning. This may explain why production of fluent speech is hindered when individuals are forbidden to use facial expressions and gestures. Among patients with impaired word retrieval,approximately 70% of gestures are abnormal or produced with hesitation. Aphasia patients appear to frequently use a compensatory strategy in which gesture production is increased (Hadar et al., 1998). The observation and execution of transitive hand movements such as bringing an object to the mouth or grasping an object with the mouth have been found to affect the simultaneous pronunciation of syllables,and particularly the vocal spectra of vowels (Gentilucci et al., 2004; Bernardis and Gentilucci, 2006). The existence of the mirror neuron system represents strong support for the motor theory of speech perception, and has led to a new branch of psycholinguistics termed “Embodied Semantics”(Chersi et al., 2010). Using transcranial magnetic stimulation, Buccino et al. (2005) found that hearing sentences related to the hand regulated motor evoked potentials in hand muscles, while sentences related to the foot regulated motor evoked potentials in foot muscles. This indicates that motor cortical activity is implicated in the processing of motion-related language stimuli. Glenberg and Kaschak (2002) also reported on a new phenomenon termed the “action-sentence compatibility effect”, which is associated with language comprehension. This phenomenon suggests that sentence comprehension is affected by arm motor responses. In their study, when a sentence implied action in one direction (for example, closing a drawer implied an action that was “moving away from the body”), the participants had difficulty making a judgment requiring a response in the opposite direction (Glenberg and Kaschak, 2002).
Although mirror neuron system-targeted action-observation treatment has been applied in post-stroke patients with motor dysfunction and complex regional pain syndrome, few studies have examined the therapeutic effect of action-observation treatment on lexical retrieval and general language function in aphasia patients (Lee et al., 2010;Duncan et al., 2016). In this study, we hypothesized that action-observation treatment based on the mirror neuron system may trigger activation and plasticity of the mirror neuron system, which is also part of the critical language network, and promote the recovery of language function in patients with aphasia. We designed a neuropsychology study to evaluate the effect of hand-action-observation treatment on aphasia patients after stroke. Specifically, we used functional magnetic resonance imaging (fMRI) to compare differences in brain activation between hand-action and dynamic-object observation with the goal of uncovering the corresponding mechanisms related to the mirror neuron system.
Participants and Methods
Participants
This randomized-block-design study was conducted in the Speech Therapy Room of Zhongda Hospital, China from January 2014 to January 2015. A total of 24 stroke patients with aphasia were randomly divided into Groups A, B, and C. Before treatment, participants in the three groups showed no significant differences in terms of age, sex, education,course of disease, or severity of disease.
Inclusion criteria: (1) First occurrence of cerebral infarction or hemorrhage; (2) 35—70 years old with a disease course of 3—24 months; (3) right handed according to the Edinburgh Handiness Inventory (Li, 1983); (4) completion of primary school (greater than 5 years of education); (5) aphasia as determined by the Western Aphasia Battery (WAB) (aphasia quotient < 93.8) (Nilipour et al., 2014); (6) no obvious disturbances in attention, memory, or visuo-spatial function(Non-language cognitive function assessment scale (Wu et al.,2013) > 70); (7) sufficient auditory ability and endurance to complete a daily training task lasting more than 30 minutes.
Exclusion criteria: (1) Frenchay dysarthria score showing moderate to severe dysarthria; (2) serious speech apraxia or oral/maxillofacial apraxia; (3) anxiety as determined by the Hamilton Anxiety Scale (Hamilton, 1959) or depression as determined by Hamilton Depression Scale (Hamilton,1960); (4) obvious dyssomnia or emotion disturbances;(5) Visual Analog Scale (Koyuncu et al., 2016) score of > 8 points; (6) diseases likely to aggravate patient's functional status such as cancer or severe heart/lung disease.
Four healthy college students enrolled at Nanjing Medical University also participated in the fMRI test.
Inclusion criteria: (1) Right handedness according to the Edinburgh Handiness Inventory (Li, 1983); (2) 18—30 years old; (3) more than 12 years of education.
Exclusion criteria: (1) Poor physical condition for any reason.
All participants received verbal and written information about the purpose and procedure of our research (Additional file 1), and provided written informed consent to participate. The study was approved by the Ethical Committees of Nanjing Medical University, China (approval number: 2011-SRFA-086) on March 11, 2011 (Additional file 2). This study follows the 2010 guidelines of the Consolidated Standards of Reporting Trials (CONSORT) and was performed in strict accordance with the Declaration of Helsinki. A flow chart showing the experimental procedure is given in Figure 1.
To ensure stability of language function in patients who had experienced a stroke, we ensured that the stroke had occurred more than 3 months prior to the study. We extended the upper limit of the course of disease to 24 months to examine the effect of hand movement observation in patients who had experienced symptoms of aphasia for over 1 year.Although strokes include cerebral infarction and cerebral hemorrhage, these classifications are not the most important confounding factors affecting training efficacy. Therefore,we did not distinguish between the two types of stroke at the time of enrollment.
We adopted stratified randomization in this study. Specifically, because aphasia severity was the main confounding factor, we divided the participants into mild, moderate and severe aphasia sub-groups according to the aphasia quotient score on the WAB, and then randomly assigned them to treatment group A, B, or C. Using the minimum random method, we calculated the sample size to be 24.
Interventions

Figure 1 Experimental flow chart.
We asked the patients in Group A to watch a video showing goal-directed transitive hand movements (e.g., flapping a fan).When they heard the name of the objects being manipulated(e.g., fan), they were instructed to repeat them. Treatment materials comprised 175 videos showing different goal-directed dynamic hand movements and common objects in everyday life, such as waving a fan, writing with a pen, and peeling a boiled egg. Each video was shown for 12 seconds and included triplicate hand actions, meaning that each hand action lasted for 4 seconds and was repeated three times. For each video, the participants were instructed to observe the mute hand action carefully during the first 4 seconds, and then watch the same hand action in the second and third 4-second periods and repeat the object name. Thus, they repeated the object name heard in the video twice.
The patients in Group B watched videos showing a dynamic rotating meaningless object (e.g., a fan rotating on an automatic turnplate). They were asked to list the name of the object being manipulated (e.g., fan), and then repeat corresponding nouns. Treatment materials comprised 175 videos showing different daily-use objects rotating on an automatic turnplate, such as a rotating fan, a rotating pen, and a rotating egg. Each video was 12 seconds long and included three object-rotating fragments, such that each object-rotation lasted 4 seconds and repeated three times. For each video,participants were instructed to observe the mute rotating object carefully during the first 4 seconds, and then watch the same action in the second and third 4-second periods.As with Group A, they were asked to repeat the name of the object heard in the video twice.
The 175 hand-action videos displayed in Group A and 175 object-rotating videos displayed in Group B were identical in terms of the objects, number of repetitions, duration, and play order of the videos. The 175 videos were divided randomly into five groups to be played 5 days per week, such that the participants watched 35 different videos on a computer screen every day, each of which was repeated 5 times.Each participant underwent training five days per week for 35 minutes per day for two weeks. The second week of training was exactly the same as the first week.
The patients in Group C underwent routine speech therapy conducted by speech therapists (or speech-language pathologists) with graduate-level training and more than 2 years of professional experience. The traditional aphasia training content included Schuell's stimulation approach,constraint-induced aphasia therapy, the PACE (Promoting Aphasic's Communication Effectiveness) program, functional communication therapy, and melodic intonation therapy. Each patient in Group C underwent training 5 days per week for 35 minutes per day for two weeks.
Outcome measures
WAB
We chose the WAB because it is a good indication of general speech function and is an effective measure of spontaneous speech ability, auditory comprehension, repetition, and naming. The WAB score can serve as a general measure of oral language according to the aphasia quotient. We conducted four sub-tests of oral language (i.e., spontaneous speech, auditory verbal comprehension, repetition, and naming) and measured the aphasia quotient of the WAB before and after the 2-week training period.
Picture naming test for objects
Naming materials were 180 object pictures selected from standardized picture naming norms for Mandarin Chinese(Liu et al., 2011). The 180 object pictures were divided into three groups that were equal in terms of concept familiarity,concept agreement, image agreement, and word frequency and used as the naming materials at 0 weeks (before treatment) and after 1 and 2 weeks of treatment.
Picture naming test for actions
Naming materials were 120 action pictures selected from the Russian language and neuropsychological research online database (http://neuroling.ru/en/analog.htm). The 120 action pictures were divided into three groups, as with the object naming materials, and used at 0 weeks (before treatment) and after 1 and 2 weeks of treatment.
The naming test comprised 60 objects and 40 action pictures. We used E-Prime 2.0 software (http://pstnet.com/products/e-prime/) to implement the naming test. The pictures were presented one at a time in random order for 20 seconds, and were separated by a five-second interval.The participants were instructed to observe the pictures and verbally report the corresponding noun or verb as soon as possible. The response time and correct/incorrect reactions were recorded using E-Prime 2.0.
fMRI measure
We conducted an fMRI experiment to investigate the influence of hand-action observation on language function and the corresponding neurophysiological mechanisms underlying mirror neuron system. An aphasia patient (Liao,Broca's aphasia, Case 2 in the behavioral experiment) and his age-matched wife (Zhao), both right-handed, underwent the fMRI experiment along with other four healthy college student participants.
In comparing brain activation during hand-action observation and dynamic-object observation, we adopted a block-designed fMRI procedure to avoid bias. During fMRI scanning, the participants were presented two sets of stimuli including two hand-action blocks (Protocol A), two dynamic object blocks (Protocol B), and five rest blocks. Run 1 had structure R-A-R-B-R-B-R-A-R, and Run 2 had structure R-B-R-A-R-A-R-B-R (Figure 2A).
Each hand-action block (Protocol A) lasted 60 seconds and included 20 trials (20 hand-action video fragments, each shown for 3 seconds). Each dynamic object block (Protocol B) lasted 60 seconds and included 20 trials (20 dynamic object-rotating video fragments, each shown for 3 seconds).In addition, we included a rest block (see crosshair “+”) that lasted 20 seconds (the first block was 28 seconds and the 8 second-images were discarded to confirm the stability of the MRI signal). Therefore, the total time of each run was 348 seconds (Figure 2B).
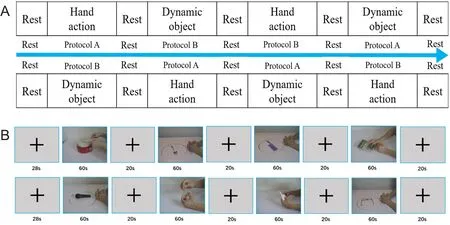
Figure 2 Procedure of fMRI experiment.
To verify that the participants watched the videos continuously without distraction, they were asked to press a button on a reaction box as soon as they saw a video of a tube of toothpaste being squeezed (20% in Protocol A) or rotating on the table (20% in Protocol B).
The area of the mirror neuron system most strongly activated by viewing three-dimensional images was labeled as the region of interest. The eight regions of interest included the bilateral posterior part of the inferior frontal gyrus(BA44/45 area), the ventral premotor cortex (BA6 area), the inferior parietal lobule (ventral BA40 area), and the superior temporal cortex (BA22 area).
Statistical analysis
The data are presented as the mean ± SE. Data were analyzed using the SPSS 22.0 software package (IBM, Chicago,IL, USA). We compared the three groups in terms of naming performance, scores, and the aphasia quotient from the WAB using a one-way analysis of variance and the least significant difference test. The level of statistical significance was set at P < 0.05.
Results
Behavioral consequences of different rehabilitation treatments in aphasia patients
The three groups showed no significant differences in terms of age, years of education, or stroke course (F = 0.067, P= 0.936; F = 0.120, P = 0.888; F = 1.089, P = 0.355). Before treatment, the WAB evaluation indicated that there were no significant differences in language function among the three groups (F = 0.008, P = 0.992; Table 1).
The WAB results showed that before the behavioral study,there were no significant differences in noun retrieval or verb retrieval among Groups A, B, and C (F = 0.004, P =0.960; F = 0.996, P = 0.942). After 1 week of training, Group A showed a significant improvement in object and action naming (t = 3.819, P = 0.007; t = 6.788, P = 0.000), while Group B did not appear to make any significant progress (t= 0.188, P = 0.857; t = 1.000, P = 0.351) compared with thatbefore training. Group C made significant progress in terms of object but not verb naming in the first week of training(t = 4.784, P = 0.002). The extent of improvement in object naming was similar between Groups A and C (P = 0.300).After the second week of training, both Groups A and C showed significant improvement in object and action naming compared with before treatment (Group A: t = 6.257, P= 0.000; t = 7.435, P = 0.000; Group C: t = 4.537, P = 0.003; t= 2.693, P = 0.031). Importantly, Group A made further significant progress in object and action naming after the first week of training (t = 3.114, P = 0.017; t = 4.498, P = 0.003),while this was not the case for Group B even after 2 weeks of training (t = 0.789, P = 0.456; t = 2.263, P = 0.058; Table 2).
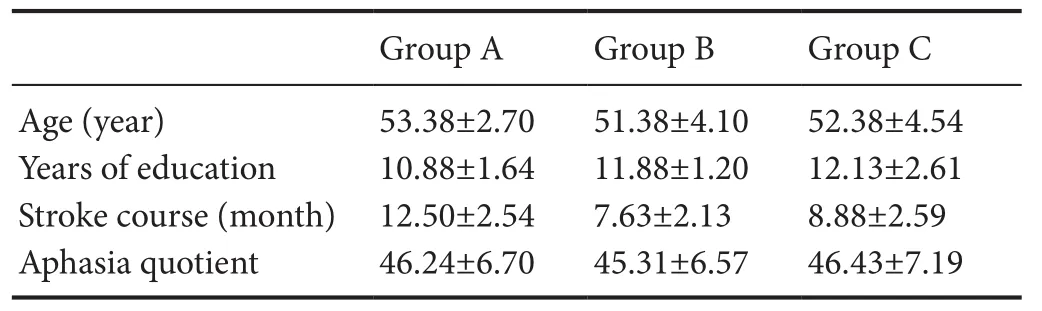
Table 1 Demographic information for aphasia patients in different groups
In regards to the WAB test, while all three groups exhibited significant improvement after 2 weeks (t = 7.719, P =0.000; t = 9.170, P = 0.000; t = 8.312, P = 0.000), the degree to which the aphasia quotient increased was not the same among the three groups (F = 8.529, P = 0.002). The degree of progress in the aphasia quotient was equal between Groups A and C, and superior to that in Group B (P = 0.001, P =0.005; Figure 3).
The scores for the four WAB sub-tests i.e., spontaneous speech (including content and fluency), auditory verbal comprehension, repetition, and naming, are shown above.Before the study, we found no significant differences in scores on the four sub-tests (F = 0.044, P = 0.95; F = 0.211,P = 0.812; F = 0.02, P = 0.998; F = 0.357, P = 0.953, respec-tively) among Groups A, B, and C, or in terms of content or fluency scores for spontaneous speech (F = 0.334, P = 0.72;F = 0.197, P = 0.823, respectively). After 2 weeks of therapy,both Groups A and C exhibited significant improvements in not only the aphasia quotient but also in all four WAB subtests, i.e., spontaneous speech, auditory verbal comprehension, repetition, and naming (Group A: t = 56.355, P = 0.000;t = 3.702, P = 0.008; t = 3.283, P = 0.013; t = 5.557, P = 0.001,respectively; Group C: t = 3.224, P = 0.001; t = 5.007, P =0.002; t = 3.945, P = 0.006; t = 4.618, P = 0.002, respectively).Furthermore, the extent of progress in the above four WAB sub-tests was equal among Groups A and C (P = 0.404; P =0.746; P = 0.147; P = 0.509, respectively). However, GroupB did not make any significant improvements in the above sub-tests (t = 2.049, P = 0.080; t = 1.379, P = 0.210; t = 2.078,P = 0.076, respectively) except for repetition (t = 3.157, P =0.016). Groups A and C made progress in terms of content and fluency scores for spontaneous speech (Group A: t =3.667, P = 0.008; t = 2.646, P = 0.033, respectively; Group C: t = 2.826, P = 0.026; t = 4.965, P = 0.002, respectively). In terms of content score, the degree of progress in Groups A and C was equal, but Group C made more progress in terms of fluency score compared with Group A (P = 0.034). Group B showed no significant improvements in terms of the content and fluency dimensions of spontaneous speech (t =1.000, P = 0.351; t = 1.528, P = 0.170, respectively; Figure 4).
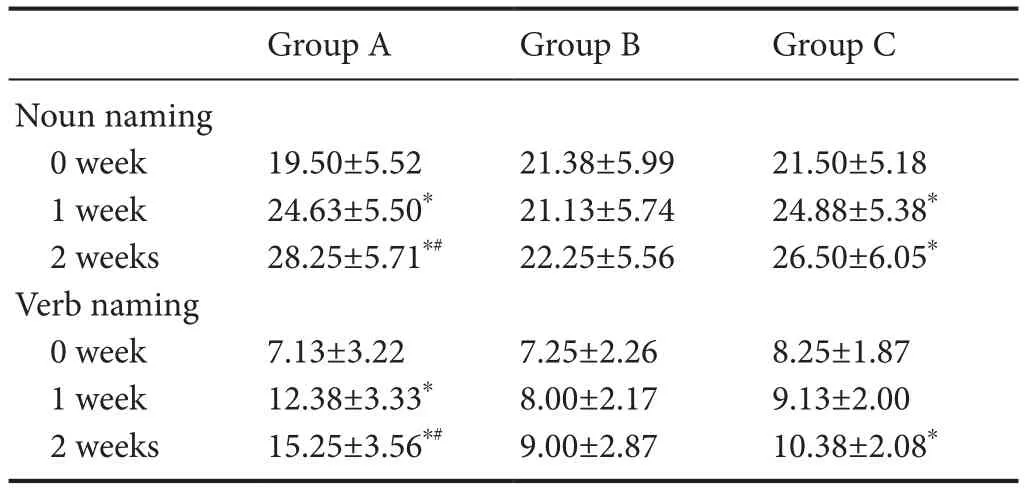
Table 2 Noun naming and verb naming performance before and after training in aphasia patients in different rehabilitation treatment groups
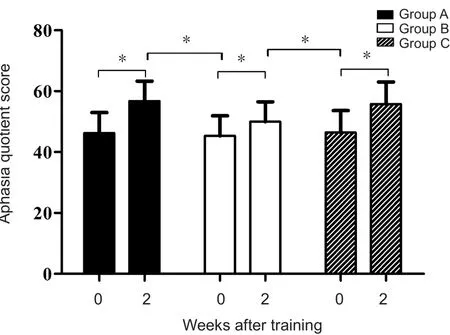
Figure 3 Aphasia quotient of the Western Aphasia Battery before and after training in three groups of aphasia patients.

Figure 4 Speech content, fluency, spontaneous speech, auditory verbal comprehension, repetition, and naming scores in the Western Aphasia Battery for aphasia patients in different rehabilitation treatment groups.
After observing rotating objects and engaging in repetition training for two weeks, the aphasia quotient score in group B significantly improved. However, subtest scores showed that individuals in group B only improved in terms of repetition items, and that there was no significant improvement in spontaneous speech, auditory verbal comprehension, or naming test scores. This suggests that the training received by Group B had a smaller impact on speech and naming compared with action-observation training.
fMRI examination of aphasia patients following different rehabilitation treatments
In the fMRI experiment, we examined brain activation in six participants during the hand-action observation task (Protocol A) and object-rotating observation task (Protocol B)(Figure 5). Figure 5A shows the brain activation of an aphasia patient (Liao, Broca's aphasia) during an fMRI task and Figure 5B-F shows the brain activation of his age-matched wife (Zhao), along with that of four healthy college student participants. In the three-dimensional activation images of each participant, we found that activation in the left and right hemispheres during the object-rotating observation task had four regions of interest, namely in areas BA44/45, BA6, BA40,and BA22. The clear difference in activated areas between Protocol A and Protocol B indicated that hand-action observation elicited more activation in bilateral mirror neuron system areas compared with rotated-object observation.
Discussion
Mirror neuron-theory-based mirror therapy, including mirror treatment, motion imagery therapy, and action-observe therapy has been applied widely for post-stroke rehabilitation of hemiplegia/hemiparesis and complex regional pain syndrome (Stevens and Stoykov, 2003, 2004; Yavuzer et al.,2008). However, to the best of our knowledge, few studies have examined the efficacy of hand-action on aphasia rehabilitation. Duncan and colleagues asked aphasia participants to observe a mouth-action (the shape of the mouth) and repeat the corresponding pronunciation. The researchers found no differences between observation of mouth-actions and static faces in terms of lexical retrieval or global language function (aphasia quotient in the WAB) (Duncan et al., 2016). Their study was conducted in response to a preliminary study that reported that hand-action observation may be efficacious for aphasia rehabilitation (Chen et al., 2015). We carried out the present neuropsychology and fMRI study to investigate the effect of hand-action observation training on language function and to examine the corresponding mechanisms underlying mirror neuron system in aphasia patients.
Currently, most speech-language pathologists implement traditional aphasia treatments, which center on the principle of “re-education” and emphasize intensive and sustained treatments targeting specific language deficits. Impairments are expected to exist permanently, and so patients are encouraged to make limited gains in function by training unspecified brain circuits, such as those that increase communication efficacy (Aten et al., 1982). However, unlike traditional “re-education” strategies that target specific language deficits at the behavioral level, the “brain repair” strategy emphasizes neurophysiological rehabilitation and aims to reactivate or repair damaged neural circuits (Small et al.,2013). In the present study, our goal was to explore ways in which it might be possible to activate and “repair” a specific neural circuit in the mirror neuron system by assessing its mechanisms of action and language function recovery via hand motion observation training (Buccino et al., 2006;Johnston, 2009). We agree with Small et al. that stroke treatment should be fundamentally neurological, and that the mechanisms of neural repair involve plasticity of cells and circuits (Buccino et al., 2006). Developmentally, neural networks are shaped by intensive experience over years of practice, and brain remodeling after injury requires similar levels of experience (Johansson, 2000; Hunt and Castillo, 2012).The mirror neuron system-targeted action-observation treatment is just one approach used in new models for neurological brain repair, which propose that brain plasticity is a synaptic phenomenon that is largely stimulus-dependent,and that brain repair requires both physical and behavioral interventions to rewire specific brain circuits (Johnston,2009; Spitzer, 2012).
Our neuropsychological data indicate that, compared with dynamic object observation, hand-action observation can improve lexical retrieval, spontaneous speech auditory comprehension, repetition, naming, and aphasia quotient.The therapeutic effect of hand-action observation was nearly equal that of the traditional method, and it even had advantages in terms of facilitating word retrieval and speech content as measured by the WAB. Our fMRI experiment showed that, compared with dynamic-object observation,hand-action observation elicited more activation in mirror neuron system-related areas, including important language centers. Hand-action observation training may have generated these effects because it elicited greater activation of the mirror neuron system, including critical language centers,compared with dynamic-object observation. This may have led to enhanced restoration and plasticity in impaired language networks.
In this study, 1—2 weeks of hand-action observation treatment led to significant improvement in the WAB test,specifically picture naming of objects and actions. This was the case even in some individuals with chronic aphasia who had previously undergone traditional training. Hand-action observation induced activation in mirror neuron system-associated areas including important language centers. The mirror neuron system closely links brain with behavior, and plasticity in this region enhances brain network connectivity. If the treatment method tested in the present study enhances the plasticity of brain network interactions, this could have important implications for aphasia patients with respect to clinical and community rehabilitation.
The present study included behavioral data from 24 patients and fMRI data from 6 adults (1 patient and 5 healthy participants). Further studies with larger sample popula-tions are necessary, as well as studies that include patients with different types of aphasia. Brain functional imaging or transcranial magnetic stimulation techniques may be helpful in testing whether improvements in language function in aphasia patients are associated with mirror neuron system activation. Simultaneously, further aphasia training methods based on the mirror neuron system should be explored.
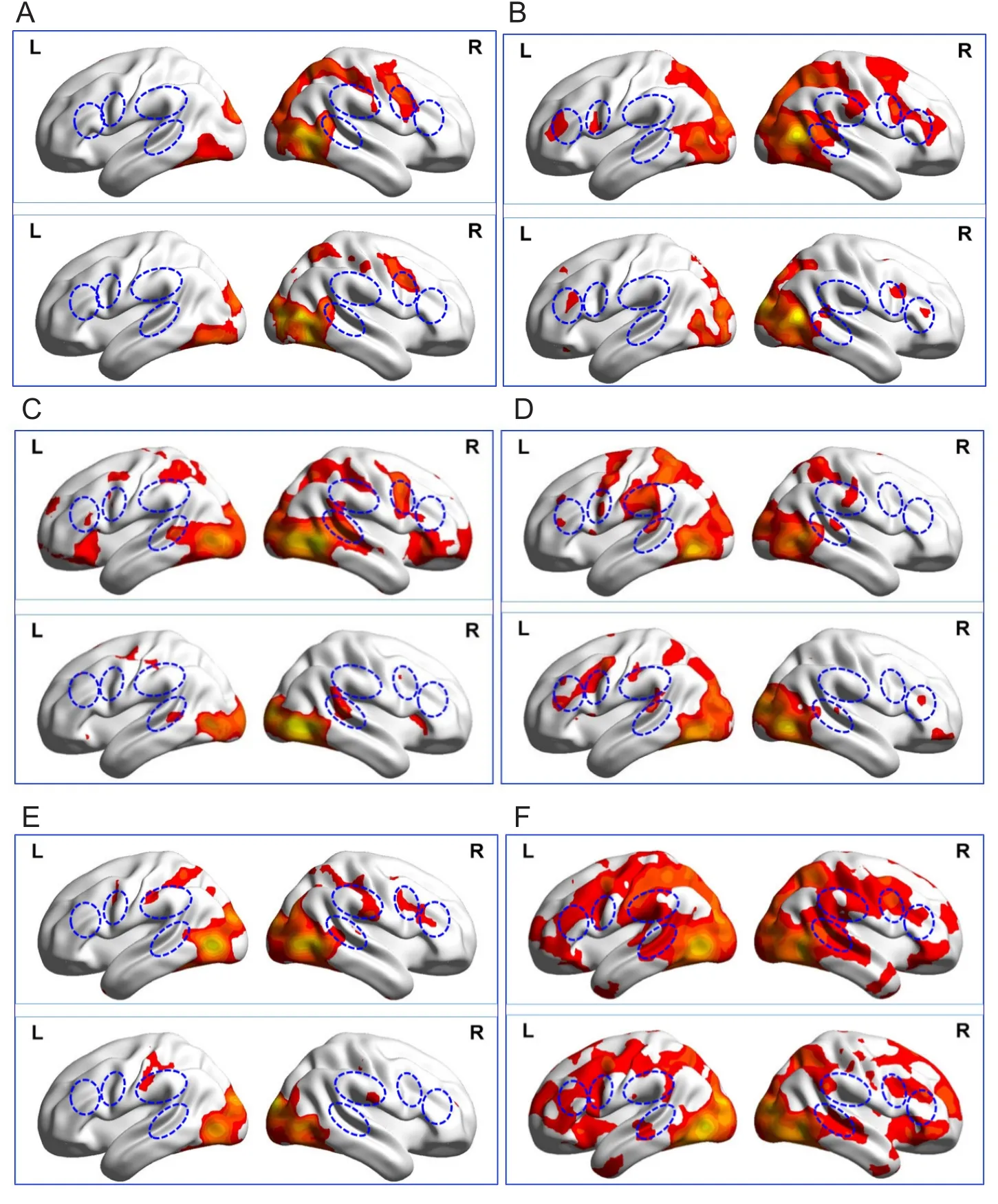
Figure 5 Three-dimensional activation images during Task A and Task B for an aphasia patient,his wife, and healthy volunteers.
Acknowledgments:We thank all the participants in this study.
Author contributions:Study design: CLS, WLC, and QY; experimental implementation, data analysis and paper writing: WLC, QY; experimental implementation: SCZ, YX, XY, TFY; study supervising and paper reviewing: JAL, CLS. All authors approved the final version of the paper.
Conflicts of interest:The authors confirm that this article content has no conflict of interest.
Financial support:This work was supported by the National Natural Science Foundation of China, No. 81472163, 81874035 (to CLS); the General Project of University Philosophy and Social Science Research of China, No. 2016SJB740015 (to QY); the Science and Technology Plan Project of Zhangjiagang city of China in 2016, No. ZKS1615 (to WLC);the Youth Science and Technology Project of Suzhou Health Development through Scientific Research and Education in 2018, No. KJXW2018059 (to WLC). Funders had no involvement in the study design; data collection,management, analysis, and interpretation; paper writing; or decision to submit the paper for publication.
Institutional review board statement:The protocol was approved by the Ethical Committees of Nanjing Medical University, China (approval number: 2011-SRFA-086) on March 11, 2011. This study was performed in strict accordance with the Declaration of Helsinki. All participants provided written informed consent. This trial had been registered in the ISRCTN Registry (ISRCTN84827527).
Declaration of patient consent:The authors certify that they obtained all appropriate patient and their legal guardian consent forms. In the forms the patients and their legal guardian have given their consent for patients' images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Reporting statement:This study followed the CONsolidated Standards Of Reporting Trials (CONSORT) 2010 guidelines.
Biostatistics statement:The statistical methods of this study were reviewed by the biostatistician of the Nanjing Medical University, China.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement:Individual participant data that underlie the results reported in this article after deidentification (text, tables, figures,and appendices) will be shared. Study protocol, informed consent form and clinical study report will be promulgated within 6 months after the completion of the trial. Results will be disseminated through presentations at scientific meetings and/or by publication in a peer-reviewed journal.Anonymized trial data will be available indefinitely at www. figshare.com.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Non-Commercial-ShareAlike 4.0 License, which allows others to remix, tweak,and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:Min Cheol Chang, University of Ulsan College of Medicine, Republic of Korea.
Additional files:
Additional file 1:Informed Consent Form (in Chinese).
Additional file 2:Ethical Approval Documentation (in Chinese).
Additional file 3:Open peer review report 1.
- 中国神经再生研究(英文版)的其它文章
- Busting the myth: more good than harm in transgenic cells
- Comparative study of microarray and experimental data on Schwann cells in peripheral nerve degeneration and regeneration: big data analysis
- Lessons from glaucoma: rethinking the fluid-brain barriers in common neurodegenerative disorders
- Characteristics and advantages of adenoassociated virus vector-mediated gene therapy for neurodegenerative diseases
- Gene expression changes in dorsal root ganglia following peripheral nerve injury: roles in in flammation, cell death and nociception
- Nicotinamide adenine dinucleotide phosphate oxidase activation and neuronal death after ischemic stroke