Hydrocarbon pneumonitis following fuel siphonage: A case report and literature review
Yi-jung Chen, Chien-chin Hsu,2, Kuo-tai Chen,3
1 Emergency Department, Chi-Mei Medical Center, Tainan, Taiwan, China
2 Department of Biotechnology, Southern Tainan University of Technology, Tainan, Taiwan, China
3 Department of Emergency Medicine, School of Medicine, College of Medicine, Taipei Medical University, Taipei, Taiwan,China
KEY WORDS: Siphonage; Diesel; Fuel; Aspiration; Hydrocarbon pneumonitis
INTRODUCTION
Siphonage is the process of transferring fluid from a container to another container. People occasionally siphon fuel to fill their tanks. However, this process is potentially dangerous and could have severe consequences. Fuel oil is a mixture of long-chain saturated hydrocarbons obtained from petroleum.Gastrointestinal ingestion usually results in transient vomiting, diarrhea, and abdominal pain.[1]However,hydrocarbons disrupt surfactants, decrease pulmonary compliance, and cause a direct inflammatory response in the lungs.[1,2]Aspiration or inhalation of oil results in hydrocarbon pneumonitis. Symptoms can vary, ranging from diseases with a chronic indolent course to rapidly progressing fatal diseases.[1]Fuel siphonage involves forceful suction from a hose and a large amount of aspiration, which can commonly result in an accelerated clinical process. This route of poisoning is different from other cases commonly seen in cases of hydrocarbon pneumonitis, such as occupational exposure faced by fire eaters, accidental ingestion by children, and choking by aged or disabled patients.[1-4]We present the case of a patient with severe hydrocarbon pneumonitis after fuel siphonage, and we review the relevant literature for a better understanding of its clinical features and possible management strategies.
CASE
A 57-year-old man was taken to the emergency department after trying to siphon diesel from a tank via a hose, consequently accidentally aspirating a mouthful of diesel. Soon after the event, the patient began experiencing chest pain and shortness of breath,with his condition worsening over the course of a few hours. He reported no relevant premedical history, but reported nicotine (a pack of cigarettes) and alcohol(half a bottle of spirit) use daily for 20 years. At the time of arrival, his vitals were as follows: temperature 37.2 °C; pulse 85 beats/minute; respiratory rate 24 breaths/minute; and arterial pressure 122/71 mmHg. A physical examination revealed the man to be conscious but experiencing respiratory distress. The examination revealed coarse breath sounds and regular but rapid heartbeats during chest auscultation. Oxygen saturation was 88%, as measured by non-invasive pulse oximetry.A chest X-ray (CXR) displayed a moderate-sized heart and opacifications and in filtrations over the right middle,right lower, and left lower lung fields (Figure 1A).Laboratory tests revealed a decreased white blood cell count (700 cells/μL) and lactic acidosis (serum lactate 4.1 mmol/L). The patient subsequently underwent tracheal intubation with mechanical ventilation in the emergency department for deteriorated respiratory distress.
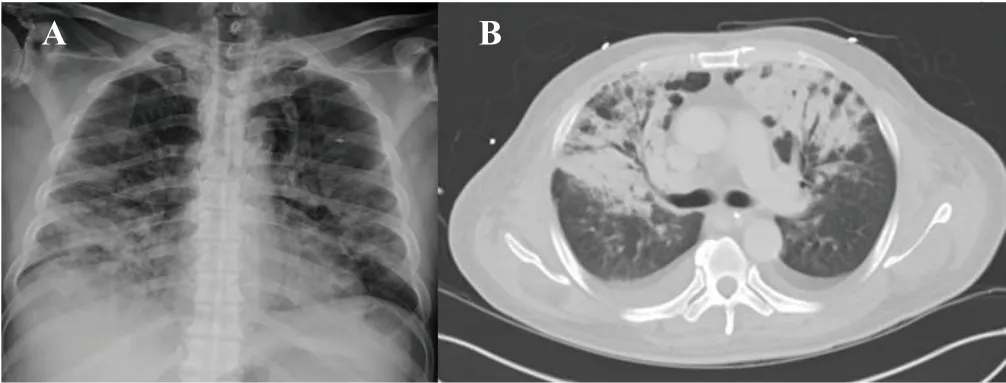
Figure 1. Patient’s CXR and CT results. A: patient’s CXR revealing a moderate-sized heart and opacifications and infiltrations over the right middle, right lower, and left lower lung fields; B: patient’s CT of the torso revealing pulmonary interlobular septal thickening and consolidation.
After admission, the patient received intravenous antibiotics (Amoxicillin + Clavulanic acid 1200 mg q8h)and steroid therapies (hydrocortisone 100 mg q12h). Two days later, the patient’s white blood cell count increased to 4,400 cells/μL; nevertheless, the opacifications on his CXR did not improve. The first course of antibiotics and steroid was continued for 2 weeks. An echocardiogram revealed decreased cardiac contractility (left ventricular ejection fraction, 45%), which might be contributed to direct cardiac toxicity of hydrocarbon poisoning.[1]A computed tomographic scan (CT) of the torso revealed interlobular septal thickening and consolidation (Figure 1B). He later underwent bronchoalveolar lavage (BAL)to clean the tracheobronchial tree, tracheostomy to facilitate respiratory care, and tube thoracostomy for ventilator related pneumothorax. He was weaned from the ventilator on the 73rdday and discharged on the 97thday of his admission. Four months after undertaking fuel siphonage, the patient’s CXR continued to display increased infiltrations, and pulmonary fibrosis was suspected. However, his pulmonary symptoms had subsided, and his pulmonary function test was normal.
LITERATURE REVIEW
A literature search was performed with the following keywords: “diesel”, “gasoline”, “kerosene”, “fuel oil”,“siphonage”, “aspiration”, “lipoid pneumonia”, “lipid pneumonia”, and “hydrocarbon pneumonitis” from 1960 to 2017. The databases searched included PubMed and Google Scholar, and the articles were cross-referenced with the initial studies. No language restriction was applied. Two reviewers screened titles and abstracts to identify articles for full review and evaluate the full text of potentially eligible studies. Only articles concerning about fuel siphonage were included. Disagreements between reviewers were resolved by consensus, and if necessary, consultation with a third reviewer. In total, nine articles[6,8,10,12-14,16-18]were identified during the databases search and another 6 articles[5,7,9,11,15]were discovered from associated references. This resulted in a total of 3 original articles and 12 case reports for the presented review.
RESULTS
We added our presented case for data analysis. A total of 40 cases were included in this review. These cases were distributed across different countries including Russia, the United Kingdom, the United States,China, India, Turkey, and South Korea, which indicates that fuel siphonage remains a widespread procedure globally. The reviewed literature are list in Table 1. Most patients were men (39/40, 97.5%), indicating that men are most likely to carry out fuel siphonage. The age range of patients was 18-64 years (mean, 34.3 years).Pulmonary infiltration and opacification were found in most cases following fuel siphonage. The right middle lobe (80%) was the predominant lung field involved,followed by the right lower lobe (46.7%), the left lower lobe (40%), and the left upper lobe (3.3%). More than one-third of patients (36.7%) showed the involvement of two lobes and nearly one-sixth of patients (16.7%)involved more than two lobes (Figure 2). Leukocytosis was a common finding in most patients. In the reported case, the patient presented with leukopenia for the first 2 days, subsequently developing into leukocytosis during his hospital stay.
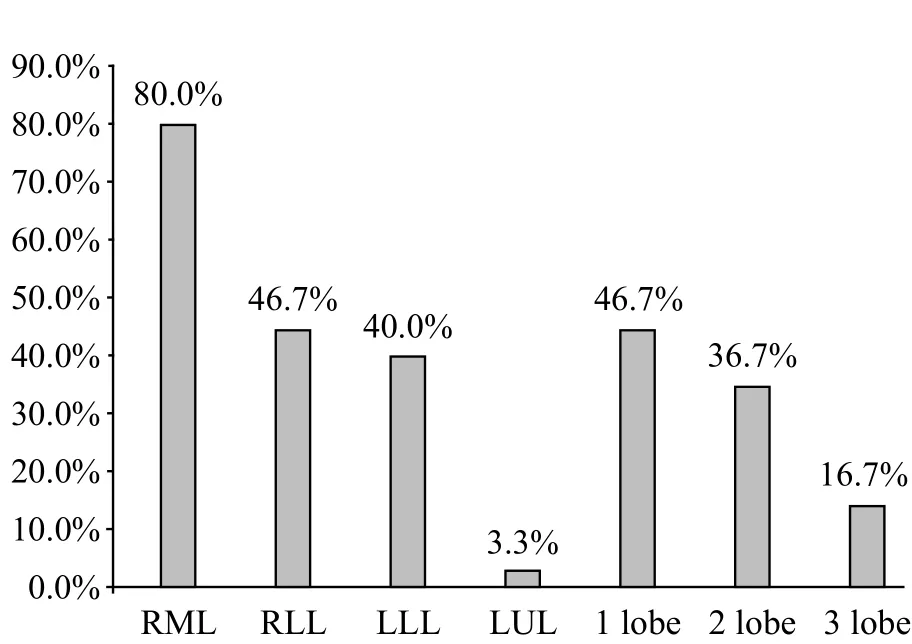
Figure 2. Involved pulmonary lobes. Right middle lobe (80%) was the predominant lung field involved, followed by right lower lobe (46.7%),left lower lobe (40%), and left upper lobe (3.3%). More than one-third of patients (36.7%) showed involvement of two lobes, and nearly onesixth of patients (16.7%) showed involvement of more than two lobes.RML: right middle lobe; RLL: right lower lobe; LLL: left lower lobe;LUL: left upper lobe.
Symptoms
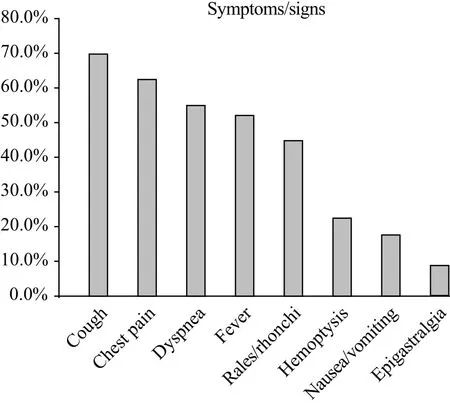
Figure 3. Reported symptoms. Cough (70%), chest pain (62.5%),dyspnoea (55%), and fever (52.5%) presented in more than half of all patients. Other clinical manifestations included rales or rhonchi (45%),hemoptysis (22.5%), nausea or vomiting (17.5%), and epigastralgia(7.5%).

Table 1. The reviewed literature
Fuel siphonage has been practised worldwide for decades; hence, case series and case reports have consistently been published worldwide.[4-18]Although hydrocarbon aspiration results in multiorgan toxicity,acute toxidrome primarily presents with pulmonary symptoms.[1-19]Most patients (80%) became symptomatic within 1 day of fuel siphonage. Cough (70%), chest pain (62.5%), dyspnoea (55%), and fever (52.5%)presented in more than half of all patients. Other clinical manifestations included rales or rhonchi (45%),haemoptysis (22.5%), nausea or vomiting (17.5%), and epigastralgia (7.5%) (Figure 3). Unlike fire eaters or patients with chronic diseases, who usually had sustained repeated episodes of aspiration and presented with an indolent disease progression, patients who experienced complications after fuel siphonage presented with an expeditious disease course; 80% of all cases showed obvious symptoms within 24 hours of siphonage. This finding is consistent with those in the literature.[1-3,20,21]
Diagnosis
Diagnosis of patients who may have undertaken fuel siphonage depends on three criteria: presence of pulmonary symptoms following an episode of fuel siphonage, typical manifestations on radiologic investigations (CXR or chest CT) with suspected history,and lipid-laden macrophages on BAL or pathologic findings.[3]If bystanders or the patients themselves mention having engaged in fuel contact, then the diagnosis is established.[22]We suggested physicians order CXR and monitor the patients’ oxygenation and respiratory symptoms to determine the severity level.However, if no witnesses are available and the patient is in an altered mental state, unable to recount what happened, the symptoms and features revealed by CXR of hydrocarbon pneumonitis are similar to those of pneumonia.[12]
In patients with hydrocarbon pneumonitis, the pulmonary infiltrations and opacifications are usually revealed early by CXR. Most patients present with lower pulmonary field involvement, and the right middle lobe is the most commonly involved lobe.[2,3,6]The resolutions of pulmonary lesions on CXR can last long after improvements in patients’ clinical symptoms. In the reviewed studies, we found that pulmonary lesions remained obvious 2 months after discharge.[8,12,15]
Mrachiori et al[3]discovered four common parenchymal abnormalities of hydrocarbon pneumonitis in images of chest CT, including consolidations with an air bronchogram, ground-glass opacifications, air-space nodules, and crazy-paving pattern. Nevertheless, none of these findings are unique to hydrocarbon pneumonitis.Areas of fat attenuation within the consolidation were reported as a characteristic manifestation of hydrocarbon pneumonitis.[2]However, fat attenuation may later be obscured by superimposed in flammation.[2]
In patients with pneumonia who are unresponsive to conventional treatment, further tests are required to reveal the underlying causes of pulmonary lesions. If the pathologic findings derived from bronchoscopic or percutaneous biopsy demonstrate a lipid-laden macrophage, hydrocarbon pneumonitis should be suspected and a further review of the patient’s history for possible fuel aspiration should be undertaken.
Treatment
Apart from supportive care, treatments with intravenous antibiotics (92%), steroids (57.5%), and BAL (32.5%) are common therapies. Although antibiotics are ineffective in the treatment of hydrocarbon pneumonitis, most patients with h ydrocarbon pneumonitis undergo treatment with antibiotics because radiologically differentiating between hydrocarbon pneumonitis and superimposed pulmonary infection is impossible. Additionally, leukocytosis is commonly observed in patients with hydrocarbon pneumonitis, which is also a typical laboratory finding in cases of pneumonia. Regarding the therapeutic effects of steroid treatment, Sen et al[23]reported in their retrospective study that patients with hydrocarbon pneumonitis responded well to steroid therapy. However, an animal study carried out to examine the effects of corticosteroids and antibiotics in the treatment of hydrocarbon aspiration found no supporting evidence for their use.[24]A few case reports have reported dramatic improvements after BAL in patients with hydrocarbon pneumonitis.[25,26]
However, none of these treatments have adequate scientific evidence to prove their therapeutic effect on patients with hydrocarbon pneumonitis.
Therefore, supportive care remains the mainstay of treatment for this condition.
Evaluation, complications, and prognosis
The majority of patients showed clinical manifestations on the first day after aspiration, and CXR also quickly revealed noticeable signs of pulmonary involvement.The progress and severity of subsequent pulmonary symptoms determine the requirements for further care and length of hospital stay. Similar to patients with pneumonia, symptomatic improvement might precedes the resolution of lesions on CXR. Thus, decisions on treatment should depend on the patients’ pulmonary symptoms. Nearly 20% of patients demonstrated an oxygenation saturation level of less than 90% on arrival at hospital, and one case eventually required continuous positive airway pressure mask ventilation; another case underwent tracheal intubation with ventilator support.Of those patients whose hospital course was fully documented, 40.9% had to be admitted for more than 1 week; moreover, three cases required intensive care and one case was fatal. We found three complications,all pulmonary sequelae, including one empyema,one pulmonary abscess, and one pneumothorax. The complication and mortality rates in this review were 7.5% and 2.5%, respectively. A retrospective study concerning hydrocarbon-poisoned children in the Negeve Desert found favourable outcomes for the study cohort.[20]These results indicate that, after proper supportive care,hydrocarbon pneumonitis rarely causes severe morbidity,or mortality, in patients.
CONCLUSION
Regarding the frequency of fuel siphonage in the population, this procedure may result in more cases of occult or unreported hydrocarbon pneumonitis, which are clearly harmful to patients’ health and productivity.Clinically, estimating the amount of aspirated fuel and evaluating the severity of patients’ condition following fuel siphonage are difficult processes.Severe pulmonary symptoms, hypoxia on arrival, and pulmonary involvements on CXR were determined to be key factors indicating the possibility of severe disease.In cases with ambiguous history, chest CT and BAL provide evidence to prove the presence of hydrocarbon pneumonitis. Supportive care remains the mainstay of treatment; whereas antibiotics, steroids, and BAL are reasonable therapeutic choices. Patients’ clinical improvement precedes the resolution of lesions on CXR.Most complications arise from these pulmonary lesions.The prognosis of patients suffering from hydrocarbon pneumonitis following fuel siphonage might be improved by accurate diagnosis and appropriate care.
Funding:This research received no specific grant from any funding agency, commercial or not-for-pro fit sectors.
Ethical approval:The Institutional Review Board approved the study.
Conflicts of interest:Authors have no financial or other conflicts of interest related to this submission.
Contributors:YC proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
 World journal of emergency medicine2019年2期
World journal of emergency medicine2019年2期
- World journal of emergency medicine的其它文章
- Keeping nephrotic syndrome on the emergency department edema differential: A case report
- Instructions for Authors
- A patient presenting painful chest wall swelling:Tietze syndrome
- Central nervous system manifestations due to iatrogenic adrenal insufficiency in a Ewing sarcoma patient
- Perceived effectiveness of infection control practices in Laundry of a tertiary healthcare centre
- Can an 8th grade student learn point of care ultrasound?
