A patient presenting painful chest wall swelling:Tietze syndrome
Kohei Sawada, Hiromi Ihoriya, Taihei Yamada, Tetsuya Yumoto, Kohei Tsukahara, Takaaki Osako, Hiromichi Naito, Atsunori Nakao
Department of Emergency, Critical Care and Disaster Medicine, Okayama University Graduate School of Medicine,Dentistry and Pharmaceutical Sciences, 2-5-1 Shikata-cho, Kita-ku, Okayama-shi, Okayama, 700-8558, Japan
Dear editor,
Patients frequently visit the emergency room with acute chest pain. While some potentially life-threatening disorders may cause the pain, in approximately 80% of cases, the chest pain source is benign, and musculoskeletal chest pain accounts for nearly 20%-50% of those cases.[1-6]Thus, pain caused by benign and pathological conditions of the chest wall encountered in the emergency department is sometimes incorrectly attributed to angina pectoris or pleuritic and other serious cardiopulmonary diseases.
Tietze syndrome is an inflammatory ailment characterized by chest pain and costochondral junction swelling with unknown cause. Tietze first described the syndrome in 1921 as a non-suppurative, benign, painful superior chondrosternal joint swelling. We report a case of Tietze syndrome in a 41-year-old male experiencing acute chest pain. Pain caused by this disease is frequently referred to the emergency department and occasionally misdiagnosed as pleurisy, angina pectoris,or other severe cardiopulmonary disorders. Our report may help raise awareness of the clinical presentation and the management of this disease among emergency physicians. Emergency physicians must be aware that musculoskeletal chest pain causes are frequent but often overlooked.
CASE
A 41-year-old man without traumatic episode presented to our emergency room complaining of acuteonset anterior chest pain. His past medical history was unremarkable without diabetes mellitus, but the patient reported smoking and alcohol consumption on a regular basis. The patient stated that the severe pain felt like a stabbing knife and was unlike any pain experienced before.
On physical examination, his temperature was 36.4°C, blood pressure 134/73 mmHg, pulse rate 78 beats/minute, and oxygen saturation 99% on room air. He was oriented and coherent in conversation. The patient had swelling of the third chondrosternal joints and tenderness on palpation. Initial electrocardiogram was normal without ST-segment elevation or depression. No arrhythmia or abnormal T-wave change was detected.His laboratory data was unremarkable and his white blood cell count and serum troponin level were normal.Radiographs were examined to rule out pulmonary and cardiovascular causes and were found to be normal.Chest computed tomography (CT) showed minimal focal enlargement of the left second chondrosternal joint without fracture (Figure 1). Based on clinical and radiological findings, Tietze syndrome was diagnosed.A non-steroidal anti-inflammatory drug (NSAID) was administered. After a few days, the NSAID relieved the pain. Twelve months after the first visit, the patient no longer experienced chest pain during exertion or rest,and restriction of joint movement and swelling over the chondrosternal joints were gone.
DISCUSSION
Tietze syndrome usually presents in both male and female adults under the age of 40. The source of this condition is not known. No causal link has been found between Tietze syndrome and occupation, geography,or ethnicity; however, there have been clustered cases.Results of the few pathological studies conducted vary from no unusual findings to degradation and swelling of the costal cartilage with associated minimal in flammation of the perichondrium.[7]
One differential diagnosis for Tietze syndrome is costochondritis, a more common condition characterized by tenderness and pain of the chondrosternal joints without swelling.[8]The term costochondritis is used interchangeably with costosternal syndrome and chest wall syndrome, and definitions are not consistent.[9]These syndromes are all characterized by pain and local tenderness at the costochondral or chondrosternal articulations, or even at the xiphoid process, but without the in flammation and swelling seen in Tietze syndrome.Many patients are left untreated and undiagnosed,possibly leading to further unnecessary examinations or cost.
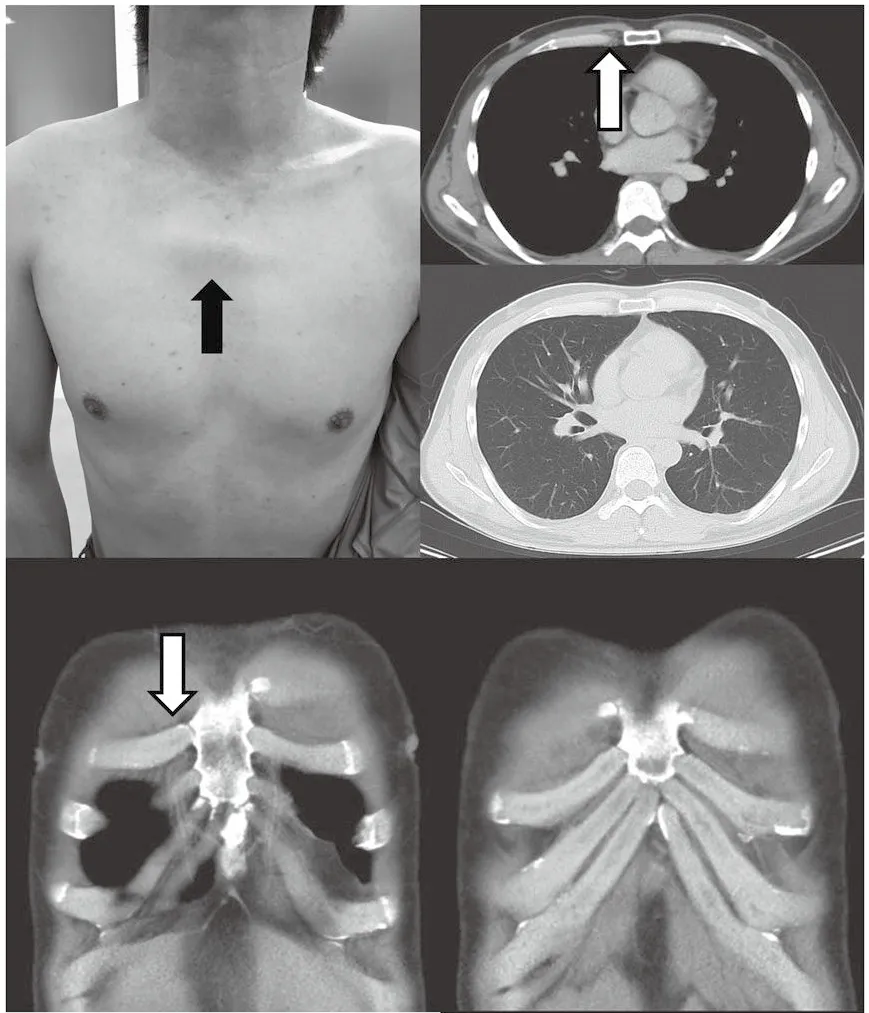
Figure 1. The patient had swelling of the second chondrosternal joints and tenderness on palpation (black arrow, left upper panel). Chest computed tomography (CT) showed minimal focal enlargement of the right second chondrosternal joint without fracture (white arrow).
Diagnosis is a clinical one, as there are no characteristic laboratory or radiographic findings. Full characterization of the chest pain is needed regarding site, onset,radiation, and exacerbating and relieving factors.Reproducible chest wall tenderness helps to rule out acute coronary syndrome in patients with acute chest pain in an early stage of the evaluation process.[10]Manual palpation of pain and motion of muscles and joints of the chest wall and cervicothoracic spine are important; however, pain localization does not help with differential diagnosis, since pain localization of acute coronary disease does not differ from that experienced by patients with chest wall syndrome, gastroesophageal reflux disease, or psychogenic chest pain. Interestingly,one study showed that the final diagnosis in patients presenting acute chest pain in the emergency room were chest wall syndrome in 46.6%, acute coronary disease in 14.8%, and psychogenic disorders in 9.5%.Gastroesophageal reflux disease and hypertension were seen in 3.5% and 4.0% of the patients with chest pain,respectively.[11]
Thus, this diagnosis of Tietze syndrome is based on ruling out other possibly life-threatening health issues affecting the chondrosternal joints, such as tumors and pyogenic and rheumatoid arthritis, after careful case history,physical exam, and test results analysis.[12]Obviously, acute injuries or trauma including rib contusion or fracture and muscular strains should be excluded. Physicians can confirm a musculoskeletal diagnosis using clinical examination alone, an important part of which is reproducing the pain by movement or palpation over the pain-originating structure. Differential diagnosis between Tietze syndrome and chest wall tumors is often difficult, especially in a patient with a history of malignant disease that frequently metastasizes to the bone. CT or bone scintigraphy is not specific enough to confirm malignant or other benign costochondral junction disorders. A report of a patient with Tietze's syndrome and squamous cell carcinoma of the mediastinum with unknown primary site invading the anterior chest wall and sternum has been published.[13]Clinicians should more closely follow patients with Tietze syndrome and should consider early diagnostic biopsy in cases of increasing swelling size.[1]Treatment strategies comprise manual therapy and administration of anti-inflammatory agents and analgesics either orally, topically, or by injection. Focal local anesthetic injection alone may also be a useful therapeutic and diagnostic tool. As mentioned above, careful follow-up is critical.
CONCLUSION
Chest wall syndrome constitutes the most common etiology of chest pain seen in primary care. Emergency physicians must be aware of the management and clinical presentation of Tietze syndrome to avoid further unnecessary anxiety, time, and expense.
Funding:None.
Ethical approval:Not needed.
Conflicts of interest:The authors declare that there are no conflicts of interest regarding the publication of this paper.
Contributors:KS proposed the study, analyzed the data and wrote the first drafts. All authors contributed to the design and interpretation of the study and to further drafts.
 World journal of emergency medicine2019年2期
World journal of emergency medicine2019年2期
- World journal of emergency medicine的其它文章
- Keeping nephrotic syndrome on the emergency department edema differential: A case report
- Instructions for Authors
- Central nervous system manifestations due to iatrogenic adrenal insufficiency in a Ewing sarcoma patient
- Perceived effectiveness of infection control practices in Laundry of a tertiary healthcare centre
- Can an 8th grade student learn point of care ultrasound?
- The “PAWPER-on-a-page”: Increasing global access to a low-cost weight estimation system
