Can an 8th grade student learn point of care ultrasound?
Alexander S. Kwon, Shadi Lahham, John C. Fox
1 Sage Hill School, 20402 Newport Coast Drive, Newport Coast, California 92657, USA
2 Department of Emergency Medicine, UC Irvine Medical Center, UC Irvine School of Medicine, Irvine, Orange, California 92868, USA
KEY WORDS: Point of care ultrasound; FAST; Image acquisition; Training
INTRODUCTION
Point-of-care ultrasound (POCUS) has become a well-established diagnostic tool in the emergency and outpatient settings. Previous studies have documented its ease of use with minimal training. The teaching of POCUS to healthcare providers is well described and ultrasound training begins as early as the first year of medical school in the United States.[1]In recent years,POCUS has gained widespread use in developing countries due to decreased equipment costs and improved telemedicine capabilities of transmittable digital images.[2,3]Many of these resource-limited areas lack personnel with medical background or experience. Thus ultrasound training, and specifically image acquisition skills, is occurring with more frequency in non-medical personnel.[4]
Currently, few published studies exist exploring ultrasound use in non-medical personnel. NASA reported successful use of ultrasound by an astronaut aboard the International Space Station using verbal remote guidance from the ground.[5]Undergraduate college students in the United States participated in a POCUS course with good self-reported learning,[6]while another study showed good diagnostic accuracy at the bedside in college student users after a one-hour training session on musculoskeletal ultrasound.[7]
It is unclear how effectively ultrasound skills can be taught to laypersons of varying educational levels.According to the United Nations Educational, Scientific,and Cultural Organization Institute for Statistics (UIS),the average adult in the United States has 13 years of formal education. By comparison, UIS reports 40 countries where the typical adult averages less than 9 years of schooling, including Brazil and Mexico.[8]When considering starting a basic POCUS training program in non-medical personnel in one of these 40 countries, we realize that the average learner will not have a high school education. Given this dilemma, we sought to evaluate if American 8thgrade students can be trained to acquire ultrasound images that would be considered clinically useful by a physician ultrasound expert. A second objective was to determine if an 8thgrade student can teach peers these skills.
METHODS
This was a prospective, observational study of the entire 8th-grade class at a small private school in Orange County, California, USA in January 2016. The study was reviewed and approved by the site review board and school administrators. Prior to enrollment in the study,all subjects and their parents were required to complete assent and consent forms, respectively. Enrollment in the study was voluntary and participants were not reimbursed for their participation.
A certified medical sonographer presented a didactic 19-slide Powerpoint lecture introducing the Focused Assessment with Sonography for Trauma (FAST) to the entire class. This lecture highlighted basic anatomy and the four conventional image windows of the FAST exam (hepatorenal, splenorenal, subxiphoid cardiac, and retrovesical). Following the presentation, the class was divided into two groups for hands-on training to assess for image acquisition capabilities for each window of the FAST. Group A consisted of female students and used an adult female model, while Group B consisted of male students and used an adult male model. Group A received hands-on training by a certified medical sonographer, and Group B received hands-on training by a peer 8th-grade student trainer who had previously received two hours of individual hands-on training by the same medical sonographer. The total amount of didactic and hands-on training was 2 hours for each group.
Following this training period, all students were evaluated and tested individually. Students needed to independently demonstrate proficiency by obtaining adequate images of the four windows of the FAST scan. A total of four video clips of 15 seconds each were recorded and stored in the machine’s hard drive. All images were obtained using two SonoSite Edge ultrasound machines with phased array probes(FUJIFILM SonoSite Inc, Bothell, WA). Instruction or guidance was not provided during this testing period.A blinded ultrasound expert reviewer later evaluated each of these images and deemed each image adequate or inadequate for clinical use. The data was statistically analyzed using chi-square testing.
RESULTS
A total of 20 participants were enrolled in the study,with an average age of 14.1 years. Group A had 9 female students with the average age of 13.9 years, while group B had 11 male students with an average age of 14.3 years.
A total of 80 video images were obtained. The overall image adequacy rate was 74% (59/80 images). The splenorenal window had the highest rate at 95% (19/20),followed by retrovesical at 90% (18/20), hepatorenal at 75% (15/20), and subxiphoid cardiac at 35% (7/20)(Figure 1). If cardiac images are excluded, the image adequacy rate of the other three windows combined was 87% (52/60). The total image adequacy rate of group A (sonographer-trained) was 78% (28/36), while the total image adequacy rate of group B (peer studenttrained) was 70% (31/44) (Figure 2). The difference in image adequacy rate between Groups A and B was not statistically significant (P-value 0.459, chi-square).
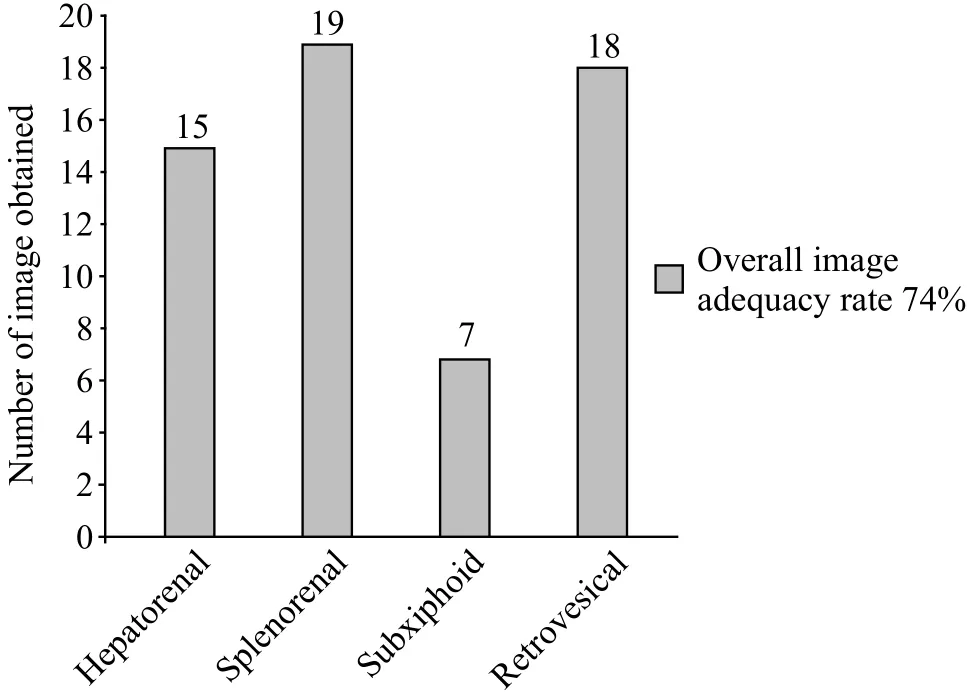
Figure 1. Clinically adequate FAST image.
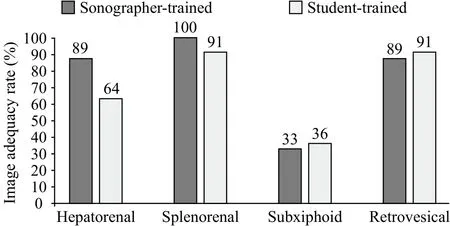
Figure 2. FAST image adequacy rate (%).
DISCUSSION
Our data suggests that an 8thgrade student has the mental and technical abilities to obtain clinically adequate FAST images in all but the subxiphoid view after a minimal amount of training. These students exhibited adequacy to obtain abdominal windows of the FAST exam. The FAST examination is one of the most common applications of POCUS, with one survey in developing countries reporting it as the second most common ultrasound application behind obstetrical use.[9]Accuracy and ease of training of FAST among physicians worldwide have been well documented,[10-12]with one Peruvian study reporting increased confidence in FAST scanning abilities in physicians after just 2.5 hours of ultrasound training.[13]While our overall image adequacy rate of 74% after two hours of training appears impressive, it is dif ficult to compare as other studies on POCUS applications among non-physicians are lacking.A non-physician astronaut aboard the International Space Station successfully completed a FAST exam in 5.5 minutes with only brief training and voice assistance by a ground-based ultrasound expert.[5]A study from Spain by Garcia-Casasola et al[14]reported that 4thyear medical students with over 15 hours of hands-on training correctly imaged and identified the liver, spleen, and kidneys over 95% of the time, while the heart via the subxiphoid view had the lowest rate at 55%. In another study, after a three-day college POCUS course in the United States, premedical college students self-rated performing bladder ultrasound as their strongest area(4.86 on Likert scale), while obtaining the subxiphoid view their weakest area (4.40).[6]These findings are consistent with our study, in which we found the bladder window to be the second easiest image to capture, while the cardiac window was the most dif ficult.
The higher POCUS image acquisition success rates in the Spanish study discussed above is expected given the advanced education of medical students compared to the 8thgraders in our study. Additionally, that study also had more hands-on training of over 15 hours, compared to just 2 hours in our study. Unfortunately, our hands-on training time was limited due to the nature of a typical 8thgrade school day and time limitations placed by school administrators. While we can assume that increasing hands-on training will increase image acquisition success in these young users, we are unsure as to how much a lack of physical maturation or higher education would act as a barrier to that success. Further studies involving non-medically trained adults of varying educational levels may help impact the design of ultrasound training for these groups going forward. Special attention in future studies should be given to better teaching in acquiring the subxiphoid view in FAST.
POCUS continues to gain widespread use in developing countries and resource-limited settings.Financial constraints can frequently be overcome by industry or corporate donations.[2,15]The most common barrier cited for POCUS use in these areas is lack of expert training and continuing education at the local level.[2,9]Due to this lack of local ultrasound physician expertise, some have utilized non-medical personnel with little or no ultrasound training. A review in low and middle income countries showed that the vast majority of persons performing ultrasound do not meet the World Health Organization ultrasound training criteria, and that many ultrasound users are non-medical personnel with little to no formal training.[4]Previous studies suggest that task-shifting and training non-physicians may be the only way to sustain ultrasound use in these areas.[4,16]Peer teaching and “training the trainer” education programs may be another way to expand and maintain ultrasound skills.
Peer-assisted learning is a proven and cost-effective method to train adult students across many industries and learning environments. An evidence-based review suggests that peer teaching in medical school programs is comparable to conventional faculty-based teaching when utilized in selected contexts.[17]Specific to ultrasound training, medical student-teachers have proven that they can be just as effective as faculty teachers when training peers in abdominal and musculoskeletal ultrasound as well as sonographic anatomy.[14,18,19]Our study showed no difference in scanning ability between the group trained by the professional sonographer and the group trained by the student trainer. Although there was only one student trainer in this study, our results suggest that peer-assisted learning for POCUS can be employed effectively in students without any prior medical education or experience. The medical adage “see one, do one, teach one” may apply to ultrasound image acquisition in novice users, and peer teaching may lead to program sustainability in these underdeveloped areas.
It is important to note that in our study, although one group received hands-on training by a peer 8thgrade student trainer, both groups received didactic instruction from a professional medical sonographer only. In a resource-poor setting where the goal is to have peerto-peer teaching, didactic training by a professional expert may not be practical or possible. However, in areas that may be employing non-medical personnel to acquire images to send digitally, it can be assumed that computers with Internet access will be a minimal standard. Online video lectures by remote experts could substitute for minimally interactive lecture material provided by live credentialed teachers, while peerassisted interactive hands-on training will take place onsite. Thus, we don’t feel that having the sonographer give both groups a didactic lecture was a study design flaw, as it can be reproduced in a real world setting.
Lastly, ultrasound and telemedicine merit discussion.With increased capabilities to transmit digital images worldwide for remote interpretation, there is increasing interest in developing ultrasound programs in low and middle income countries. The NASA study cited earlier is an extreme example of effective telesonography from outer space. First responders in the prehospital setting have also shown an impressive diagnostic accuracy of 88% with FAST studies using real-time remote review by an emergency physician.[20]These studies illustrate the power of telemedicine and importance of training proper image acquisitions skills at the local level. With smaller and more affordable hand-held ultrasound devices being brought to market, the popularity of POCUS and demand for ultrasound training will continue to rise in underdeveloped areas.
Limitations
Th ere are several limitations to this study. The main limitation is the single school and geographic site, thus it is unclear if our findings will be generalizable to other regions and ages. The demographics of 8thgrade students vary widely in other parts of the country and world. The two groups of learners were also divided based on gender,which may have produced a selection bias. Future studies will need to be obtained to determine if gender plays a role in the ability to acquire ultrasound images. Lastly,the study sample size was small and thus not powered to detect small but potentially relevant differences in outcomes between the two trainee groups. Future, largescale studies are needed to determine if there are any differences in image acquisition and confirm whether peer-to-peer teaching is possible at this stage.
CONCLUSIONS
Our data indicates that an 8thgrade student can obtain clinically adequate FAST images in all but the subxiphoid view after minimal training. Additionally,there was no difference found between the studenttrained group and the instructor-trained group. This data is promising, however, larger studies must be performed to determine the optimal amount of training for pro ficiency in novice or non-traditional ultrasound users.
Funding:None.
Ethical approval:The study was reviewed and approved by the site review board and school administrators.
Conflicts of interest:All authors have no financial or other conflicts of interest related to the submitted article.
Contributors:ASK led the design of the study and data collection, and drafted the manuscript. All authors contributed to the interpretation of the results and the critical revision of the manuscript.
 World journal of emergency medicine2019年2期
World journal of emergency medicine2019年2期
- World journal of emergency medicine的其它文章
- Keeping nephrotic syndrome on the emergency department edema differential: A case report
- Instructions for Authors
- A patient presenting painful chest wall swelling:Tietze syndrome
- Central nervous system manifestations due to iatrogenic adrenal insufficiency in a Ewing sarcoma patient
- Perceived effectiveness of infection control practices in Laundry of a tertiary healthcare centre
- The “PAWPER-on-a-page”: Increasing global access to a low-cost weight estimation system
