Do medical students studying in the United Kingdom have an adequate factual knowledge of basic life support?
Robert D. Willmore, Damjan Veljanoski, Feray Ozdes, Bethan Stephens, James Mooney, Seamus G.Crumley, Arpan Doshi, Philippa Davies, Shreya Badhrinarayanan, Emily Day, Kristian Tattam0, April Wilson0, Nathan Crang, Lorna Green, Craig A. Mounsey, Howell Fu, Joseph Williams, Michelle S.D'souza, Dhanya Sebastian, Liam A. Mcgiveron, Matthew G. Percy, James Cohen, Imogen J. John,Alice Lethbridge, Imogen Watkins, Omar Amin, Mubasher A. Qamar0, John Gerrard Hanrahan, Emily Cramond-Wong
1 Barts Health NHS Trust, London, United Kingdom
2 Barts & the London Medical School, Queen Mary University of London, E1 2AT, United Kingdom
3 Norwich Medical School, University of East Anglia, NR4 7TJ, United Kingdom
4 Lancaster Medical School, Lancaster University, LA1 4YW, United Kingdom
5 School of Medicine, Dentistry and Biomedical Sciences, Queen's University Belfast, BT7 1NN, United Kingdom
6 Faculty of Medicine, University of St Andrews, KY16 9AJ, United Kingdom
7 Faculty of Medicine, Dentistry and Health, University of Shef field, S10 2TN, United Kingdom
8 Brighton and Sussex University Hospitals NHS Trust, BN2 5BE, United Kingdom
9 St George's University of London, SW17 0RE, United Kingdom
10 University of Liverpool School of Medicine, L3 5PS, United Kingdom
11 University of Exeter medical school, EX4 4QJ, United Kingdom
12 Faculty of Medicine, University of Southampton, SO17 1BJ, United Kingdom
13 Medical Sciences Division, University of Oxford, OX1 3PA, United Kingdom
14 University of Edinburgh Medical School, EH8 9YL, United Kingdom
15 Faculty of Medicine, University of Warwick, CV4 7AL, United Kingdom
16 University College London Medical School, WC1E 6BT, United Kingdom
17 Cardiff University School of Medicine, CF10 3XQ, United Kingdom
18College of Medical and Dental Sciences, University of Birmingham, B15 2TT, United Kingdom
19 College of Medical, Veterinary and Life Sciences, University of Glasgow, G12 8QQ, United Kingdom
20 Guys, Kings, and St Thomas School of Medicine, King’s College London, WC2R 2LS, United Kingdom
21 Faculty of Life Sciences & Medicine, King's College London, WC2R 2LS, United Kingdom
22 Faculty of Health Sciences at the University of Nottingham, NG7 2RD, United Kingdom
KEY WORDS: Emergency Medicine; Basic life support; Medical education; Resuscitation
INTRODUCTION
Survival following cardiac arrest has significantly improved over the past nine years, although ischaemic heart disease remains a leading cause of death worldwide.[1,2]Despite continued efforts to reduce cardiovascular risk factors in the general population,one of the strongest predictors of survival following cardiac arrest is immediate bystander cardiopulmonary resuscitation (CPR).[3]Bystander CPR doubles the odds of survival compared to no CPR.[4]All staff who work in a health care setting, both clinical and non-clinical,have a duty to maintain their BLS skills annually in the event of a cardiac arrest occurring in their workplace.[5]The UK Resuscitation Council and the General Medical Council (GMC) provide clear guidelines regarding the level of training required of medical graduates on graduation. In “Tomorrow’s Doctors”, the GMC states that clinicians should be able to provide basic first aid and CPR, and the UK Resuscitation Council agrees that this is an essential competency.[6-8]However, there is no requirement for medical students to attend annual BLS training, despite having regular contact with patients within hospitals and in the community.
Little is known about the preparedness of undergraduate medical students with respect to their ability to serve as rescuers in both in-hospital and out-of-hospital cardiac emergencies. Research at individual institutions across the world have identified that the factual knowledge of BLS amongst healthcare students and healthcare professionals is poor.[9-12]No medical students achieved 100% in a survey on BLS by Almesned et al,[9]whilst Kila and Yockopua[10]found that only 44% of doctors in one institution knew the correct compression:ventilation ratio for CPR and only 33% could identify the correct rate of compressions. Authors could identify no studies in the literature assessing medical student factual knowledge of BLS on a national level within the UK.This study therefore aims to investigate medical students’factual knowledge and previous training in BLS, and to understand their perceived expectations of managing a cardiac arrest. This information may better inform medical education policy makers and regulatory bodies on the training needs of medical students.
METHODS
Ethical approval was granted by the Faculty of Health Sciences Research Ethics Committee (FREC)at the University of Bristol Faculty of Health Sciences for a cross-sectional observational closed response questionnaire of the first- and fourth-year students studying at UK medical schools. Further ethical approval was required and granted by the Faculty of Medicine and Health Research Office, School of Medicine Research Ethics Committee (SoMREC) at Leeds University for application MREC15-026. All participating institutions gave permission via year group coordinators and or ethics committee application for the study to take place.Eight medical schools refused permission or did not respond to contact from researchers and four medical schools failed to submit data within the given deadline.
Participants were recruited and data collected over a five-month period from October 2015 to February 2016 at UK medical schools. A non-random purposive sampling method was used. The first- and fourth-year students completing a medical undergraduate degree were included in this study. Students in their fourth-year of study who had undertaken an intercalated degree,research year, or a study break were not included. The year groups selected for sampling were to chosen to allow comparison of student groups at the beginning of their training and towards the end of their training.Fixed groups also allowed comparison of students at the beginning of their studies versus those who had had greater clinical experience. Furthermore the fourthyear students were chosen over those in their fifth-year to allow a greater number of institutions to take part -some medical schools offer only 4-year courses for postgraduate students and additionally the fifth-year medical students often fly abroad for medical electives during their final year of studies. Participants were recruited during university lectures or tutorial teaching sessions.The estimated population of UK medical students studying in the first- and fourth-year was 12,000. A 95%confidence level with a 2% margin of error required a minimum sample size of 2,001 respondents. With an estimated 50% response rate the minimum number of respondents invited to take part in the survey would be 4,002.
A structured closed-response paper survey was utilised with a total of ten questions. Questions regarding adult BLS knowledge were taken from the Adult Basic Life Support Manual produced by the Resuscitation Council (UK) 2015. The questionnaire complied with agreed survey based research recommendations (Good practice in the conduct and reporting of survey research[8])and avoided “double-barrelled” questions, questions containing double negatives, and leading or ambiguous questions.
The questionnaire collected information regarding the student’s year of study; BLS training received during time at medical school, and five MCQs on Adult BLS.
MCQ’s assessed students’ knowledge of the BLS algorithm including its sequence, number of compressions and ventilations delivered alongside the depth and rate of compressions in Adult BLS. Answers from two of MCQ’s were combined during analysis to ascertain if students demonstrated knowledge of the correct ratio of compression to ventilations provided during BLS. The questionnaire also evaluated student beliefs on expectations of their ability to manage a cardiac arrest using BLS and if they desired more training in BLS as part of their undergraduate curriculum.
Questionnaires were trialled on a convenience sample of the third-year students at Bristol University.The trial demonstrated that the method of sampling and that the content of the questionnaires was both suitable and feasible with a high response rate.
Participants were recruited by announcing details of the study prior to a year group lecture or year group tutorials when the data collection would take place.Paper surveys were placed on the desk where students were seated for their teaching. Consent to take part in the study was implied by the participant choosing to fill in a questionnaire. All data collected was anonymous and forms were placed into a blank collection box.
Participants who marked any year group outside of the study specifications (first or fourth year) met criteria for exclusion. Submissions that failed to mark an answer for a single question were excluded due to their questionnaires being deemed as incomplete. Students who selected two different answers were automatically marked as incorrect. A single survey was provided for each student present. Students were encouraged to take part to avoid non-response bias.
Once collected MCQ’s were marked according to a master answer sheet referenced from the Adult Basic Life Support Manual produced by the Resuscitation Council(UK) 2015. As MCQ’s were closed response there was no ambiguity in answers requiring a second opinion.
Statistical analysis was performed using Chisquared and Spearman’s rank-order correlation.Statistical and graphical analysis was performed on IBM SPSS Statistics 25® software and Microsoft Excel 2013®. Descriptive statistics for data analysis included frequencies, percentage, 95% confidence intervals, range and mean scores. Results were significantly significant if P<0.05.
RESULTS
Twenty-one of 33 UK medical schools successfully submitted data. Figure 1 shows the breakdown of responses. A total of 4,333 surveys were returned. Of the responses provided 3,732 met inclusion criteria -a 43% response rate. A greater number of responses were received from the first-year students compared to the fourth-year students (Table 1). Furthermore, there was little difference between the two groups in terms of those that had completed training outside of the medical curriculum and the duration of this training.
As shown in Table 2 the fourth-year students scored significantly more correct answers compared to the firstyear students in all MCQs except the identification of the depth of compressions during CPR (χ2[1, n=3,732]= 2.782, P=0.095). There was a small but significant difference between the number of the first-year students who correctly answered all five MCQs compared with the fourth-year students (χ2[1, n=3,732] = 9.503,P=0.002). Overall only 10.3% (n=384, 95% CI 9.9% to 10.7%) of all students could achieve a perfect score and identify the correct answer to all 5 MCQ’s.
The mean score achieved by students from different institutions was varied with a range from 4.34 to 1.65(Figure 2). The proportion of students achieving a perfect score varied widely with 54% of students at one medical school achieving a score of 5 out of 5 compared with only 2% at another.
2.1 身体动作的呈现形式丰富成套动作层次感 动作轨迹,即指在做动作时,身体或身体某部分所移动的路线。包括:轨迹形状(直线、曲线、弧线等)、轨迹方向(前后、左右、上下等6个基本方向及各种旋转与环绕等)和轨迹幅度(长度、角度)[2]。运动员的运动轨迹与方向的多变将直接在视觉上留给裁判和观众第一印象,其必须以变化多样且完整的方式利用整个地面区域,并创造出不同的模式[3]。
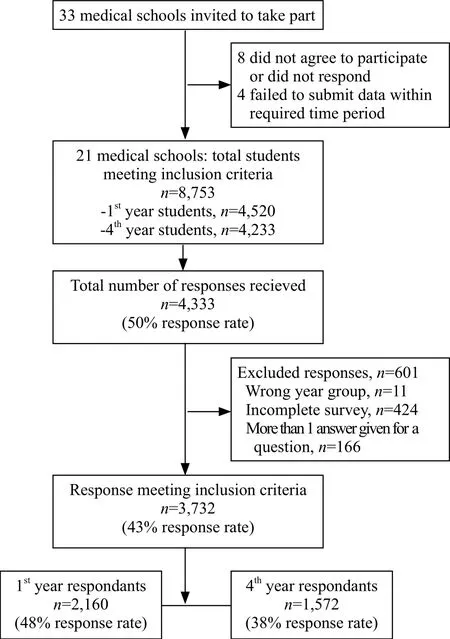
Figure 1. Overview of responses.
Only 9% (n=146) of the fourth-year students had attended a course on an annual basis compared with 49%(n=765) who had only attended a single course. Thirty percent of those that had attended 4 courses answered all questions correctly compared with 13% (n=96) of those who had attended a single course.
There was a weak, positive correlation between number of courses attended and score achieved, which was statistically significant (rs [1,572]= 0.171, P<0.001).
This study also found that 81% of students (n=3,031)wanted more BLS training in the medical school curriculum and 96% (n=3,575) believed there was an expectation for medical students to be able to manage an out-of-hospital cardiac arrest.
DISCUSSION
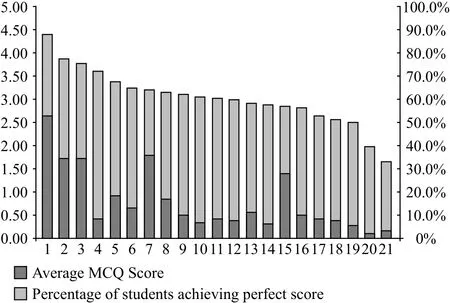
Figure 2. Differences between institutions.
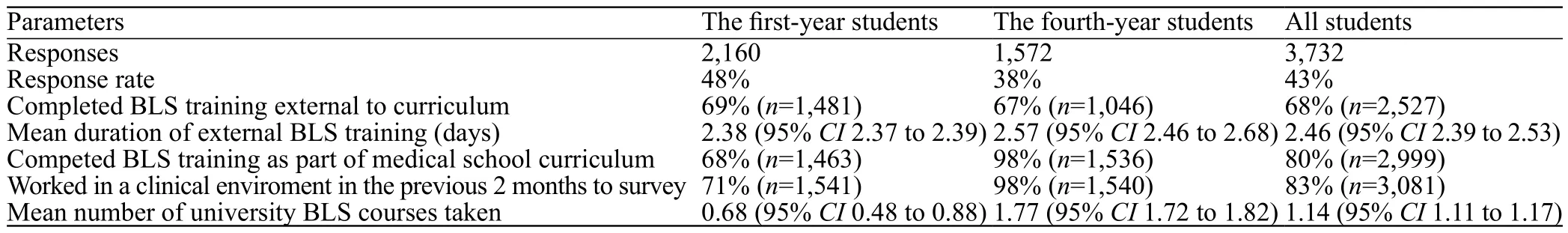
Table 1. Number of responses and training in BLS
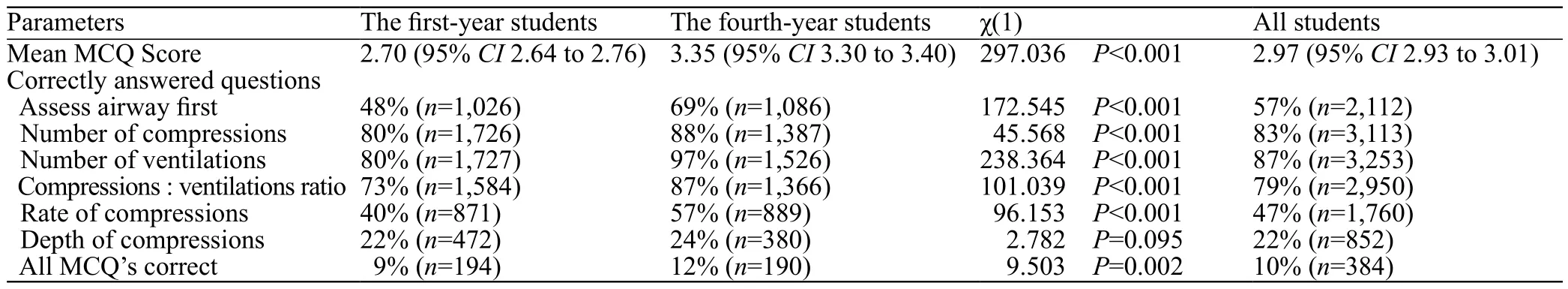
Table 2. Mean scores and correct responses to MCQ’s on adult BLS
Basic life support is an essential skill for all healthcare personnel including medical students. We found that only 10% of all students who responded had a complete factual knowledge of the aspects of BLS assessed in this study and therefore they have an inadequate factual knowledge of BLS compared with requirements of other healthcare professionals despite the majority of students receiving training both within and outside the undergraduate curriculum. There was a very small difference between the proportions of students in the two groups that could answer all questions correctly despite the additional training and clinicial exposure the fourth-year students have received. We demonstrated a positive correlation between the number of courses the fourth-year students had attended and the score they achieved. This study suggests that a single training session is inadequate to maintain BLS knowledge throughout medical school. There is a large disparity in knowledge between different medical schools in the UK with a wide range of mean scores and proportion of students achieving high scores. Students believed that there was an expectation that they should be able to manage a cardiac arrest out of hospital and wished for more training in this area. We recommend that a new UK wide recommendation should be published that requires annual BLS training for medical students to improve the overall poor understanding of basic life support resuscitation. Whilst authors understand the weak level of evidence observational studies provide the importance of a large-scale UK wide set of data with significant findings cannot be ignored.
A growing number of medical schools are moving away from a traditional curriculum in favour of earlier clinical attachments and early interaction with patients,both in hospital and in the community, as recommended by the GMC.[13]In our study the majority of UK medical students sampled felt there was an expectation they should be able to manage a cardiac arrest with BLS skills until advanced clinical help arrived. The UK Resuscitation Council states that staff in contact with patients receive at least annual training and updates in CPR.[5]Medical students, despite being in training,should be included within this requirement as they take an active role in healthcare teams both in hospital and in the community.
This study assessed factual knowledge of BLS and therefore cannot determine the ability or skills of students in delivery of BLS. However, Brown et al[14]demonstrated that accurate knowledge of CPR guidelines is associated with increased odds of correct performance in chest compression depth and compression to ventilation ratio.
McKenna and Glendon discovered that BLS trained individual’s experienced 50% “skill-fade” 2 months after training.[15]Further studies of BLS training have shown only 2.4% of trained individuals can perform effective CPR 2 years following attendance of a course.[15]We found that 49% of the fourth-year students had attended a single BLS course therefore it is unlikely they could retain practical skills over the entirety of their studies.
Research shows that the recommended compression rates are associated with the greatest survival to hospital discharge.[17]Over a third of the fourth-year students could not identify the correct rate of compressions and hence may fail to provide adequate CPR to an arrested patient according to UK Resuscitation Council Guidelines.
These data suggest a huge disparity in the standards of knowledge across different institutions in the UK and further research may identify effective methods of BLS training to target medical schools who performed poorly.We must address such wide differences in standards of knowledge by encouraging education collaboration between those that excel with the institutions which lag behind their rivals (54% vs. 2% of students answering all MCQ’s correctly).
Authors acknowledge the limitations of this study and that fewer the fourth-year medical students took part in the study compared to the first-year students, which may result in a degree of response bias. This may have been further compounded by respondents with poor factual knowledge not wishing to participate in the study,as it may highlight weaknesses in their knowledge as a cumulative group. In addition, the study only collected data regarding two year groups for logistical reasons.This study assessed factual knowledge of the BLS algorithm and cannot therefore assess ability to deliver resuscitation skills. However, it is unlikely adequate skill level could be achieved without correct factual knowledge of the BLS guidelines.
Numerous publications have suggested that regular training should be delivered to medical students but current UK guidelines have yet to implement this recommendation.[11,18-20]This study has identified both a need and a desire for additional BLS training to be put in place for medical students on a regular basis in line with guidelines for other healthcare professionals.
Funding:None.
Ethical approval:Ethical approval was granted by the Faculty of Health Sciences Research Ethics Committee (FREC) at the University of Bristol Faculty of Health Sciences under the application number 26542. Further approval was required and granted by the Faculty of Medicine and Health Research Office,School of Medicine Research Ethics Committee (SoMREC) at Leeds University for application MREC15-026. Participants gave informed consent before taking part in this study.
Conflicts of Interest:We have read and understood the journal’s and ICJME policy on declaration of interests and declare that we have no competing interests.
Contributors:Lead author and guarantor RW was responsible for the study concept and delivery in addition to affirming that the manuscript is an honest, accurate, and transparent account of the study being reported and that no important aspects of the study have been omitted. All authors made a significant contribution to collection, analysis and interpretation of the data in the study.All authors additionally critically revised the manuscript for intellectual content and approved the final version to be published.
 World journal of emergency medicine2019年2期
World journal of emergency medicine2019年2期
- World journal of emergency medicine的其它文章
- Keeping nephrotic syndrome on the emergency department edema differential: A case report
- Instructions for Authors
- A patient presenting painful chest wall swelling:Tietze syndrome
- Central nervous system manifestations due to iatrogenic adrenal insufficiency in a Ewing sarcoma patient
- Perceived effectiveness of infection control practices in Laundry of a tertiary healthcare centre
- Can an 8th grade student learn point of care ultrasound?
