Comparison of transvaginal cervical length and modified Bishop’s score as predictors for labor induction in nulliparous women
El Mekkawi SF, Hanafi S, Khalaf-Allah AE, Ibrahim A. Abdelazim,2✉, Mohammed EK
1Department of Obstetrics and Gynecology, Ain Shams University, Cairo, Egypt
2Department of Obstetrics and Gynecology, Ahmadi Hospital, Kuwait Oil Company, Ahmadi, Kuwait
3Department of Obstetrics and Gynaecology, Ministry of Health and Population, Cairo, Egypt
Keywords:Cervical length Labor induction Modified Bishop’s score
ABSTRACT Objective: To compare the transvaginal cervical length (TVCL) to the modified Bishop’s score for prediction of successful labor induction in nulliparous women. Methods: A total of 210 nulliparous women who were diagnosed as premature rupture of membranes were recruited in this comparative prospective study, which was carried out in the Obstetrics and Gynecology Department of Ain Shams University, Egypt over two years for labor induction.The studied women were examined by trans-vaginal ultrasound for measurement of the cervical length (CL) and vaginally to calculate the modified Bishop’s score, followed by induction of labor. Collected data were analyzed to compare the TVCL to the modified Bishop’s score for prediction of successful labor induction in nulliparous women. The success of induction process was defined as vaginal birth after the induction of labor.Results: One hundred and forty-three women of studied women had CL <28 mm; 122 of them delivered vaginally (P=0.030). One hundred and forty-six women of studied women had modified Bishop’s score >4; 128 of them delivered vaginally (P=0.006). The CL <28 mm was significantly more specific with more positive predictive value as predictor of successful labor induction compared to modified Bishop’s score. Induction to delivery time was significantly shorter in women with CL <28 mm than women with CL ≥28 mm (P=0.02;95% confidence interval: 4.9-8.4). In addition, induction to delivery time was significantly shorter in women with Bishop’s score >4 than women with Bishop’s score of ≤4 (P=0.01;95% confidence interval: 1.6-4.5). Conclusions: Both TVCL and the modified Bishop’s score are complementary tools in pre-induction cervical assessment before induction of labor, while the TVCL at <28 mm is significantly more specific with more positive predictive value as predictor of successful induction than the modified Bishop’s score.
1. Introduction
Induction of labor is defined as the use of surgical or medical means to start uterine contractions before the spontaneous onset of labor[1]. The reported rate of labor induction increased in the past decade[2]. Multipara, non-obese, tall women with estimated fetal weight <3.50 g are favourable factors for vaginal delivery[3,4].
In 1964, Dr. Edward Bishop developed his scoring system and stated the success of the process of labor induction depended on the pre-induction cervical condition[5,6]. Dr. Edward Bishop reported no failure with Bishop’s score ≥9 and the American College of Obstetricians and Gynecologists generally defines the cervix with Bishop’s score ≤6 as unfavourable cervix for the process of labor induction[1].
In an attempt to minimize the subjectivity of Bishop’s score, the original system has been modified to replace the cervical effacement with cervical length (CL), which is known as modified Bishop’s score[7], and it is commonly used in clinical practice. Another modification to the original Bishop’s score was proposed by Elghororiet alin which the ultrasound measurement of the CL was used instead of the clinical assessment of CL[8]. Ben-Harushet alconcluded that the CL of <28 mm was significantly associated with shorter delivery time[9].
Ultrasound is available in most of obstetrics centers, as it is safe,accurate and inexpensive. Transvaginal approach is preferred route for ultrasound assessment of the CL. Transvaginal sonography(TVS) for CL assessment was reported in the diagnosis of cervical incompetence, labor induction and prediction of preterm labor[10,11].This study is designed to compare the transvaginal cervical length(TVCL) to the modified Bishop’s score for predicting successful labor induction in nulliparous women.
2. Materials and methods
2.1. Location and time of study
A total of 210 nulliparous women who were diagnosed as premature rupture of membranes (PROM) were recruited in this comparative prospective study, which was carried out in the Obstetrics and Gynecology Department of Ain Shams University,Egypt from February 2013 to February 2015 for labor induction after written consent and approval of the Ethical Committee of the Obstetrics and Gynecology Department of Ain Shams University,Cairo, Egypt in January 2013.
2.2. Method of data collection
Nulliparous women who were diagnosed as PROM, single fetus,cephalic presentation and estimated fetal weight between 2.5 and 4.0 kg by ultrasound and reactive pre-induction non-stress test were included in this study. Exclusion criteria included twin pregnancies,non-vertex presentation, previous cesarean delivery, estimated fetal weight >4.0 kg, abnormal bony pelvis and any contraindication of vaginal delivery.
PROM was defined as rupture of fetal membranes <37 gestational weeks and diagnosed by history of sudden gush of water, positive fern and nitrazine tests. PROM was confirmed by sterile speculum examination and visualization of amniotic fluid leaking from the uterine cervix followed by amniotic fluid index ≤5 cm by tansabdominal ultrasound (TAS)[12]. Gestational age of the studied women was calculated from the first day of the last menstrual and ultrasound imaging was performed <20 weeks’ gestation[12].
The studied women were subjected to thorough evaluation and TAS to confirm the fetal lie, fetal life, placental site, absence of congenital anomalies, estimated fetal weight and amount of the amniotic fluid.
TAS was followed by vaginal ultrasound to record the TVCL and vaginal examination for cervical assessment and calculation of the modified Bishop’s score. The studied women were examined for the TVS in lithotomy position and the vaginal probe of the TVS inserted after evacuation of the bladder. Cervical canal was located from the internal os to the external os by using the amniotic fluid, fetal presenting part and the urinary bladder as landmarks. The vaginal probe moved backward until the lightest touch on the vaginal probe provided good image of the uterine cervix and the cervical canal was from the internal to the external cervical openings[4]. TVCL examinations were carried out by sonographer who was unaware of the patients’ data, using Philips HD9 with two-dimensional convex probe (Philips; Amsterdam; Netherlands). Digital vaginal examination which was carried out to record the modified Bishop’s score by the clinical investigator blinded to the TVCL.
After measurement of the CL by TVS and calculation of the modified Bishop’s score, induction of labor was done by either prostaglandin E1 (25 micrograms vaginal tablets) or misoprostol(Cytotec®, Pfizer Limited, Ramsgate Road, UK), which was inserted in the posterior vaginal fornix. When the calculated modified Bishop’s score was <5 (unfavourable cervix), the prostaglandin E1 was used for induction of labor. Vaginal examination was done 6-hourly after prostaglandin E1 insertion and further prostaglandin E1 might be inserted if uterine contractions were inadequate (maximum three doses). Oxytocin started 2 h after the last prostaglandin E1 if the uterine contractions were inadequate,cervix was ≥3 cm and the fetal presenting part station was ≥ 0. In established labor with regular uterine contractions (4–5 contractions in 10 min, each lasting ≥45 s), vaginal examination to assess the progress of labor was done every 4 h[1,4].
Intrapartum fetal surveillance was done by intrapartum fetal heart monitoring using cardiotocography. After delivery, the success (defined as vaginal birth), duration of labor induction were statistically analyzed to compare the TVCL to the modified Bishop’s score for prediction of successful labor induction in nulliparous women.
2.3. Sample size
Required sample size was calculated using G* Power software for sample size calculation (*Heinrich Heine Universität; Düsseldorf;Germany). Sample size ≥202 women needed to produce statistically accepted figure.
2.4. Statistical analysis
Statistical Package for Social Sciences (SPSS) version 18 was used for statistical analysis of the collected data. The numerical data were presented as mean ± standard deviation (mean ± SD) and the categorical data were presented as number and percentage [(n(%)].The Student’st-test and theChi-square (χ2) were used for statistical analysis andP<0.05 was considered statistically significant.
3. Results
The 210 studied nulliparous women’s mean age was (24.13±2.34)years and the mean gestational age was (38.00±1.20) weeks’gestation. Nearly, 76.19% (160/210) of the studied women delivered vaginally, whereas 23.81% (50/210) delivered by cesarean sections.The cesarean sections were done because of failed induction in 32%(16/50), failure of labor progress in 40% (20/50) and fetal distress in 28% (14/50).
There was no significant difference between the women who delivered vaginally and those who delivered by cesarean delivery regarding the mean maternal age [(24.89±4.01) yearsvs.(24.67±3.34) years; respectively], the mean gestational age at labor induction [(39.60±1.82) weeks’ gestationvs.(39.92±1.62) weeks’gestation; respectively], and the mean fetal birth weight [(2.77±0.85)kgvs.(2.71±1.22) kg; respectively].
One hundred and forty-three women of studied women had CL<28 mm; 122 of them delivered vaginally, while 21 delivered by cesarean delivery (P=0.030). One hundred and forty-six women of studied women had modified Bishop’s score >4; 128 of them delivered vaginally, while 18 delivered by cesarean delivery(P=0.006). Thirty-eight out of 67 women who had CL ≥28 mm delivered vaginally (P=0.002). Thirty-two out of 64 women who had modified Bishop’s score ≤4 delivered vaginally (P>0.050).
Receiver operator characteristics curve analysis showed that CL<28 mm had 87.50% sensitivity, 86.25% specificity, 61.40% positive predictive value and 96.50% negative predictive value for successful labor induction, whereas the modified Bishop’s score >4 had 62.50%sensitivity, 50.00% specificity, 23.80% positive predictive value and 84.20% negative predictive value for prediction of successful labor induction (Figure 1).
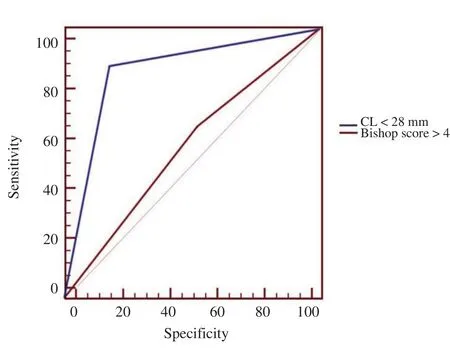
Figure 1. Receiver operating characteristic curve of modified Bishop’s score and CL as predictors of successful labor induction.
The CL <28 mm was significantly more specific with more positive predictive value as predictor of successful labor induction (86.25%and 61.40%; respectively) compared to the modified Bishop’s score(50.00% and 23.80%; respectively).
Induction to delivery time was significantly less in women with CL<28 mm than women with CL ≥28 mm (P=0.02; 95% confidence interval: 4.9-8.4). In addition, induction to delivery time was significantly less with Bishop’s score >4 compared to Bishop’s score of ≤4 (P=0.01; 95% confidence interval: 1.6-4.5) (Table 1).
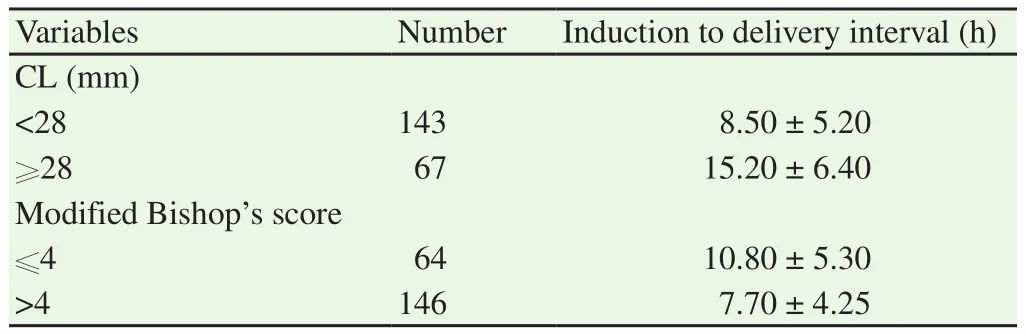
Table 1 Duration of labor induction according to CL and modified Bishop’s score(mean ± SD).
4. Discussion
Since the introduction of Bishop’s score in 1964, various scoring systems have been suggested to evaluate the cervical condition before induction of labor[7,8]. Verhoevenet al[13] and Wareet al[14] suggested that the cervical shortening by TVS should be equal to cervical effacement detected during the digital vaginal examination. In fact, conflicting results were detected in different studies comparing the TVCL versus the modified Bishop’s score as predictors for successful labor induction.
In this study and the study conducted by Abdelazimet al[4], both the modified Bishop’s score and the TVCL were good predictors for successful labor induction. In a multicenter study, Pandiset alassessed the pre-induction of modified Bishop’s score and the TVCL, and reported that both methods were significantly related to induction to delivery interval[15]. Pandiset alconcluded that the TVCL at 28 mm cut-off point and the modified Bishop’s score at 3 cut-off point were good predictors for successful induction of labor[15].
Previous studies concluded that both the modified Bishop’s score and the TVCL can predict successful labor induction and were associated with successful vaginal delivery[14-16]. The systematic review conducted by Crane[17] reported that the successful labor induction may be predicted by the modified Bishop’s score as well as the sonographic cervical assessment and recommended further studies for better evaluation of these predictors.
Recently, Stuparet alhave found that the TVCL and the modified Bishop’s score are reliable predictors for labor induction. They concluded that both the TVCL and the modified Bishop’s score were complementary for pre-induction cervical assessment[18], while Hatfieldet alin a systematic review claimed that the TVCL was not good predictor of successful induction of labor[19]. Ezebialuet alstated in their systematic review that the two methods (TVCL and modified Bishop’s score) for pre-induction cervical assessment were equal and no one method was superior to the other[5].
Both the TVCL and the modified Bishop’s score could be complementary for pre-induction cervical assessment and for prediction of successful induction of labor, while the choice of one particular method for pre-induction cervical assessment depends on the available tools and the environment of practice[5]. Ware and Raynor[14] pointed out that both the TVCL and the modified Bishop’s score can predict the duration of labor and the successful induction. Besides, they indicated that the TVCL and modified Bishop’s score were good predictors for the delivery mode[14]. In this study, the TVCL <28 mm was statistically more specific with more positive predictive value as predictor for successful induction of labor than the modified Bishop’s score.
Tanet alconcluded that the TVCL was more tolerated than the digital vaginal assessment for calculation of the modified Bishop’s score and both the TVCL and the modified Bishop’s score were good predictors for failed induction and cesarean delivery[20]. They also summarized that the TVCL >20 mm was good predictor and associated with high incidence of cesarean delivery after induction labor at term[20]. Uzunet alconfirmed that the modified Bishop’s score was good predictor for cesarean delivery compared to the TVCL in nulliparous women with prolonged pregnancy[21]. Maitraet aldrew a conclusion that that the pre-induction TVCL can independently predict the success of the vaginal delivery. They also concluded that the probability of cesarean section was <30%at TVCL cut-off point of ≤3 cm and the probability of cesarean section increased by 45% with one unit increase in the TVCL[22]. In addition, Parket alexpressed that the amount of prostaglandin used during induction of labor reduced by 50% at pre-induction TVCL of≥28 mm[23].
Recently, Papillon-Smith and Abenhaim[24] have said that studies did not demonstrate the superiority of TVCL compared to the modified Bishop’s score, and they concluded that the TVCL was useful to plan the labor induction and significantly reduce the amount of prostaglandins needed for cervical ripening.
Women who refused to give consent are the limitation of this study,while the comparative nature and the proper sample size are the strengths of the study. This study concludes that both TVCL and the modified Bishop’s score are complementary tools in pre-induction cervical assessment before induction of labor, while the TVCL at<28 mm is significantly more specific with more positive predictive value as predictor for successful induction than the modified Bishop’s score. Further studies are needed to confirm whether the TVCL is superior to the modified Bishop’s score or both are complementary tools in pre-induction cervical assessment.
Conflict of interest statement
All authors declare that there is no conflict of interest.
Acknowledgments
We would like to express our great appreciation to the women who gave consent and participated in the study.
 Asian Pacific Journal of Reproduction2019年1期
Asian Pacific Journal of Reproduction2019年1期
- Asian Pacific Journal of Reproduction的其它文章
- Infertility in China: Culture, society and a need for fertility counselling
- Total segmental aplasia of uterus body in bitch
- Chronic atrophic endometritis and pyometra in a ferret: A case report
- Value of α-fetoprotein,β-HCG, inhibin A, and UE3 at second trimester for early screening of preeclampsia
- Blood indicators of dry cows before and after administration of a drug STEMB
- Effect of butylated hydroxytoluene on quality of pre-frozen and frozen buffalo semen
