Value of α-fetoprotein,β-HCG, inhibin A, and UE3 at second trimester for early screening of preeclampsia
Farah Farzaneh, Mohaddeseh Sharifi, Nasim Nourinasab, Sarang Younesi
Shahid Beheshti University of Medical Sciences, Iran
Keywords:Preeclampsia Screening Second trimester Biomarkers
ABSTRACT Objective: To study the value ofα-fetoprotein (α-FP),β-human chorionic gonadotropin(β-HCG), inhibin A, and uncojugated estriol (UE3) at the second trimester for early screening of preeclampsia. Methods: This cohort study was performed on 1 713 consecutive pregnant women with gestational age from 15 to 18 weeks. We measured the serum levels ofα-FP, β-HCG, inhibin A, and UE3 and they were followed-up for 48 h after delivery.Results: A total of 1 713 women were recruited and through the study 151 women (8.8%)were diagnosed with preeclampsia (n=123, 21.5% in the pregnant women with high risk,n=28, 2.5% in the pregnant women with low risk; P<0.000 1). The area under receiver operating characteristic curve was estimated to be 2.39 MOM forα-FP, 2.84 MOM for β-HCG, 1.92 MOM for inhibin A, and 0.77 MOM for UE3. The best cutoff value was specifically considered for each marker that was determined a positive predictive value ranged 19.60% forα-FP, 17.62% for β-HCG, 18.33% for inhibin A and 14.88% for UE3, a negative predictive value ranged 95.63% for α-FP, 93.89% for β-HCG, 94.28% for inhibin A and 93.57% for UE3, and an area under receiver operating characteristic curve ranged 0.70 forα-FP, 0.63 forβ-HCG, 0.65 for inhibin A and 0.61 for UE3. Conclusions: This study reveals that the new cutoff values are more valuable in screening preeclampsia. Although these markers have a low positive predictive value, they present a high negative predictive value. Also, the combination ofα-FP,β-HCG and inhibin A and the combination ofα-FP and inhibin A have the highest value in screening preeclampsia.
1. Introduction
Preeclampsia is a multidimensional pregnancy disorder manifesting with a combination of new onset raised blood pressure and proteinuria occurred usually after 20 weeks of gestation in pregnant women without previous hypertensive disease[1]. Because of its multi-system feature, some other manifestations may be seen in preeclampsia patients such as hemostatic disturbances,peripheral edema, liver or renal insufficiency, and increased risk for the hemolysis, elevated liver enzyme levels, and low platelet levels syndrome[2,3]. Various patterns of preeclampsia have been introduced according to the time of disease onset, its development and poor prognosis, as well as the effects on mother health and/or fetal abnormalities. So, preeclampsia may appear as early onset(usually before 34 weeks of gestation) or as late onset (starting after 34 weeks of gestation), with or without resulting in eclampsia,presenting a maternal disorder only or concurrently with neonatal abnormalities[4,5]. Due to the importance of preventing both maternal and neonatal adverse effect of preeclampsia, prevention would be crucial. Application of sensitive and specific biomarkers is an important approach in this era[6]. Recently, several markers are suggested as predicting markers for preeclampsia; however, the predictive role of this markers or their superiority for early screening remains uncertain[7,8]. Hence, in this study, the value of the serum markers includingα-fetoprotein (α-FP),β-human chorionic gonadotropin (β-HCG), inhibin A and uncojugated estriol (UE3) in the second trimester was assessed for screening preeclampsia, in the hope that maternal and neonatal complications could be prevented.
2. Materials and methods
This prospective cohort study was done on pregnant women that came for routine visiting and screening of pregnancy-related abnormalities in 2016-2017. All pregnant women with singleton pregnancy at the gestational age between 15-18 weeks with no important past-medical history (chronic hypertension, kidney disease, metabolic syndrome, lupus syndrome, overt diabetes and history of preeclampsia) were invited to participate in the study.
In this study, 2 000 pregnant woman were recruited, among whom 287 women were excluded from the study due to exclusion criteria:1) Women who did not want to continue the study (219 women,76%); 2) Women with fetal anomalies such as trisomy 18 or 21 (68 women, 24%). Totally, 1 713 pregnant women ranging from 23 to 45 years were assessed with the mean age of (31.99±5.70) years. 49.4%were nulligravida, 50.0% were nullipar and 6.7% were obese (body mass index >30). Nullipara was a woman who had never given birth while nulligravida was a female who had never been pregnant.
All eligible women who accepted to take part in the study read and signed the consent form and filled the demographic questionnaire.Afterward, a venous blood sample (5 mL) was taken to measure the serum level of the markers (i.e.α-FP, β-HCG, inhibin A and UE3).The serum markers were analyzed with electrochemiluminescence with cobus kit and Hitachi instrument. After the test, the pregnant women were categorized into two groups based on the level of the quadruple screen test: Group 1: Abnormal level of serum markers(n=151); Group 2: Normal level of serum markers (n=1 562). The two groups were determined based on the cut-off points presented in the previous studies (α-FP > 2.5, β-HCG > 3, inhibin A > 2 and UE3 < 0.5).
The women were followed-up until delivery and also visited 48 h and two weeks after delivery to assess the presence of the manifestations of preeclampsia (hypertension, proteinuria, edema,and raised liver enzymes) for analysis the collected data. We usedChisquare and Fisher’s exact test for the qualitative variables andt-test for the quantitative variables, and demographic difference between the two groups were minimized by applying logistic regression.
Results were presented as mean±standard deviation (mean±SD) for quantitative variables and were summarized by absolute frequencies and percentages for categorical variables. Normality of data was analyzed using the Kolmogorov-Smirnoff test. Categorical variables were compared usingChi-square test or Fisher’s exact test when more than 20% of cells with expected count of less than 5 were observed. Quantitative variables were also compared withttest or Mann-Whitney test. The correlation between the study parameters was assessed using the Pearson’s correlation test. For the statistical analysis, the statistical software SPSS version 16.0 for windows(SPSS Inc., Chicago, IL) was used.P-values of 0.05 or less were considered statistically significant.
3. Results
Table 1 showed the standard deviation andP-value for the demographic variables and biomarkers for the women with abnormal serum markers and normal serum markers.P-value of the mean age for the women in group 1 and group 2 was 0.23. We divided the women between the two groups such that each of the factors age and gravid (the number of pregnancies) had the same average values in two groups and showed that preeclampsia was not affected by age and gravid (P>0.05).
We compared the levels of the serum markers for the women in group 1 and group 2. As Table 1 showed, for the women in group 1 the mean serum level ofα-FP was 2.65 MOM and for the women in group 2 it was 2.17 MOM. For the women in group 1 the mean serum level ofβ-HCG was 2.68 MOM and for the women in group 2 it was 2.27 MOM. For the women in group 1 the mean serum level of inhibin A was 1.98 MOM and for the women in group 2 it was1.67 MOM. For the women in group 1, the mean serum level of UE3 was 0.88 MOM and for the women in group 2 it was 1.08 MOM. In this study, all the markers were meaningful (P<0.000 1).

Table 1 Statistics of age, gravid and biomarkers for women with normal and abnormal serum marker.
Table 2 showed frequency and percent of preeclampsia for each biomarker. Forα-FP<2.5 andα-FP ≥ 2.5, respectively, 5.20% and 21.10% of women were diagnosed with preeclampsia (P<0.000 1).For β-HCG<3 and β-HCG ≥ 3, respectively, 6.70% and 19.60% of women were diagnosed with preeclampsia (P<0.000 1). For inhibin A<2 and inhibin A≥2, respectively, 6.20% and 20.70% of women were diagnosed with preeclampsia (P<0.000 1). For UE3<0.5 and UE3 ≥ 0.5, respectively, 7.20% and 24.70% of women were diagnosed with preeclampsia (P<0.000 1).
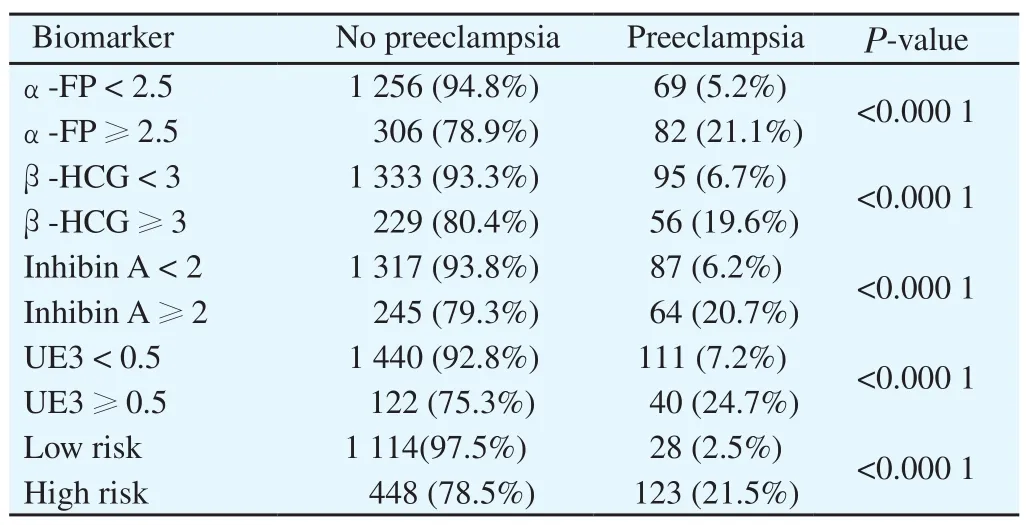
Table 2 Frequency and percentage of preeclampsia for each biomarker.
Based on the clinical and laboratory assessment, 151 women(8.8%) were diagnosed with preeclampsia. Among the highrisk patients (571 cases), 123 cases (21.5%) were diagnosed with preeclampsia and among the low-risk patients (1 142 cases), 28 cases (2.5%) were diagnosed with preeclampsia. The difference was statically significant between the two groups (P<0.000 1).
The present study showed that diagnostic accuracy indices for four biomakers with the current point. According to the cutoff value suggested in previous study, we determined a sensitivity value of 54.30% forα-FP, 37.10% for β-HCG, 42.40% for inhibin A,26.50% for UE3 and 81.46% for the combination of four markers,and a specificity ranged from 80.40% forα-FP, 85.30% forβ-HCG,84.30% for inhibin A, 92.20% for UE3 and 71.32% for combination of four markers. We also determined positive predictive value (PPV)and negative predictive value (NPV) ranged from, respectively,21.10% and 94.80% forα-FP, 19.60% and 93.30% for β-HCG,20.70% and 93.80% for inhibin A, 24.70% and 92.80% for UE3,21.54% and 97.55% for combination of four markers. The area under receiver operating characteristic curve (AUC) ranged 0.67 for α-FP, 0.61 for β-HCG, 0.63 for inhibin A, 0.59 for UE3 and 0.76 for combination of four markers. According to the results, it can be concluded that although these markers have a low PPV, they present a high NPV.
As shown in Table 3, AUC was estimated to be 2.39 MOM forα-FP, 2.84 MOM forβ-HCG, 0.77 MOM for UE3, and 1.92 MOM for inhibin A. A best cutoff value was specifically considered for each marker, which determined a sensitivity value of 64.90% forα-FP, 47.20% forβ-HCG, 50.99% for inhibin A and 47.68% for UE3,and a specificity ranged from 74.26% forα-FP, 78.75% forβ-HCG,78.04% for inhibin A and 73.62% for UE3. The values for AUC for new cutoff point were higher than that for the previous cutoff points.This revealed that this new values were more valuable in screening preeclampsia. Although these markers had a low PPV, they present a high NPV. This showed that the women in group 2 were not likely to become clinically preeclamptic. Among these biomarkers,α-FP had the highest value of screening.
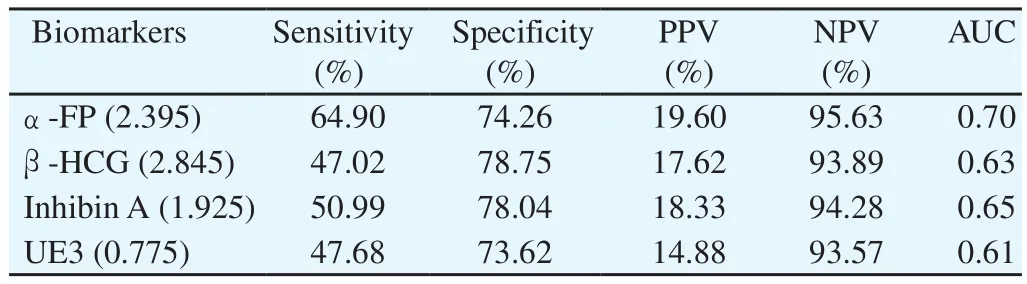
Table 3 Diagnostic accuracy indices for four biomarkers with new cutoff points.
Table 4 showed AUC among all combination of the four biomarkers for current and new cut points and 95% confidence intervals. Since the combination of all the four biomarkers has the highest AUC,it has the highest value in screening of preeclampsia. In the next levels, respectively, the combination ofα-FP, β-HCG and inhibin A and the combination ofα-FP and inhibin A had the highest value in screening preeclampsia.
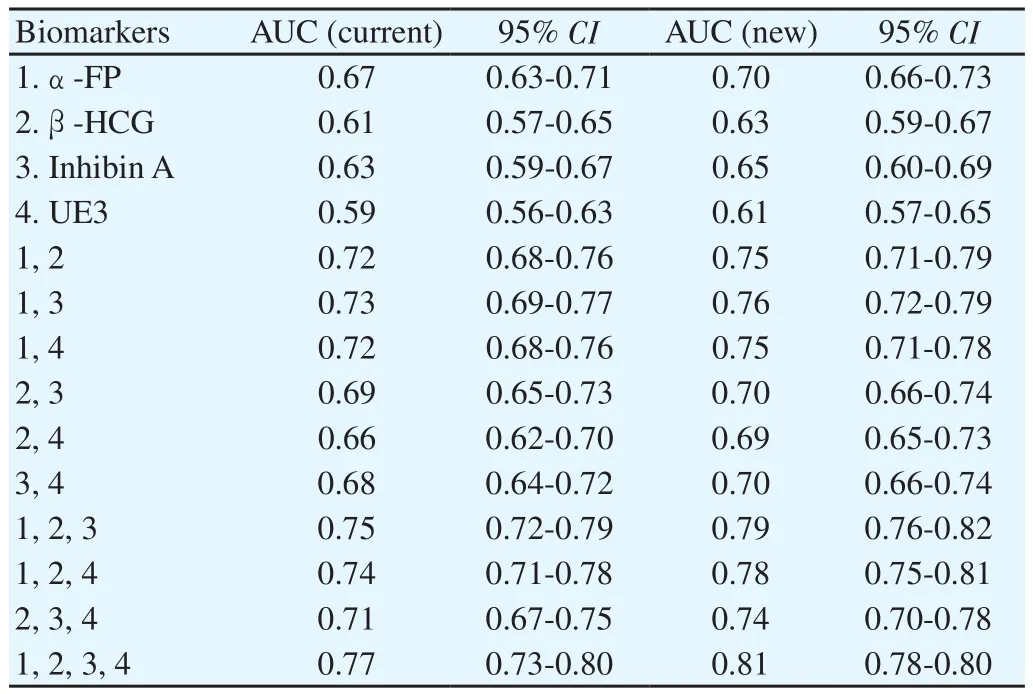
Table 4 Comparison of AUC among all combination of the four biomarkers (current and new cut points) and 95% confidence intervals.
4. Discussion
According to this study, the biomarkers, alone or in combination,can identify patients with a low risk of preeclampsia with high AUC and 95% confidence intervals, while presenting a poor PPV for these markers. The combination of all the serum markers has the highest value for predicting preeclampsia with a AUC of 0.81 (with our new cutoff). Among these biomarkers,α- FP has been able to distinguish between patients with high risk and low risk with the best diagnostic value. Therefore, it is possible to predict the risk of preeclampsia by using these markers. Combination of all the serum markers has the highest value for predicting preeclampsia with a sensitivity of 99.1%and a specificity of 74.1%. As previously noted, there is no specific marker for screening preeclampsia and some peptides produced and secreted by placenta may be predictive for preeclampsia. In the present study, we well showed that the markersα-FP,β-HCG,inhibin A, and UE3 can potentially predict preeclampsia with a valuable diagnostic accuracy.
Our study was partially comparable with the previous reports.As shown in a study on Canadian pregnant women[9], considering pregnancy associated plasma protein A<0.4 MOM andβ-HCG<0.5 MOM at the first trimester andα-FP>2.5 MOM,β-HCG>3 MOM,inhibin A>2 MOM, and UE3<0.5 MOM at the second trimester were associated with preeclampsia. As shown by Lambert-Messerlianet al[10], inhibin A and endoglin were consistently associated with preeclampsia, especially for early onset disease. A multivariate model using the three markers could identify 50% of the pregnancies with early onset preeclampsia with a 2% false positive rate. In a cohort study by Kang[11] in China, a mid-trimester inhibin A concentration of 1.5 MOM or greater had a sensitivity of 60% and a false-positive rate of 16% for the prediction of preeclampsia and thus inhibin A was the best predictor of preeclampsia. Yazdaniet al[12] showed that the risk of having pre-eclampsia significantly increased in patients with abnormal markers. Zand Vakiliet al[13] studied the relationship between preeclampsia and high levels of inhibin A and human chorionic gonadotropin. They recommend further studies on these markers to evaluate their usefulness in screening preeclampsia. In the study by Longet al[14], all four biomarkers assessed in our survey had predictive value for screening preeclampsia. The difference in the power of each marker for discriminating preeclampsia may refer to some baseline factors including the type of study, the power of studies, as well as the techniques used for measuring these markers.An important point that should be noted is that, since these markers are usually used for predicting fetal anomaly, exploiting these serum markers for predicting preeclampsia imposes no extra cost on the patients.
We can conclude that for patients with financial problems or in the laboratory’s limitations to check for serum markers, a combination of two markers can be used (e.g.combination ofα-FP and inhibin A or combination ofα-FP and UE3). Because it has a higher sensitivity in our study’s cut off, it is better that an extensive study be done to better determine cut off.
Conflict of interest statement
All authors hereby state that there is no conflict of interest.
 Asian Pacific Journal of Reproduction2019年1期
Asian Pacific Journal of Reproduction2019年1期
- Asian Pacific Journal of Reproduction的其它文章
- Infertility in China: Culture, society and a need for fertility counselling
- Total segmental aplasia of uterus body in bitch
- Chronic atrophic endometritis and pyometra in a ferret: A case report
- Comparison of transvaginal cervical length and modified Bishop’s score as predictors for labor induction in nulliparous women
- Blood indicators of dry cows before and after administration of a drug STEMB
- Effect of butylated hydroxytoluene on quality of pre-frozen and frozen buffalo semen
