胶质瘤中的表观遗传学:一场基因革命
祁 婧,闵 彬,涂艳阳
(1空军军医大学唐都医院实验外科,陕西 西安710038;2空军工程大学门诊部,陕西西安710051)
0 引言
神经胶质瘤是渗透性的脑瘤,最常见的是星形细胞瘤和少突神经胶质瘤,被分为低级别(WHO等级Ⅰ和Ⅱ)和高级别肿瘤(WHO等级Ⅲ和Ⅳ)。胶质母细胞瘤(Ⅳ级星形细胞肿瘤)是最致命且最具有破坏性的神经胶质瘤。尽管经过几十年的研究,胶质母细胞瘤和高级别神经胶质瘤的预后仍然很差。这强调了阐明肿瘤发病机制的重要性。近年来在胶质瘤分子遗传学方面取得了许多新进展,并已应用于胶质瘤的分型中,其中许多基因和分子改变可导致细胞代谢的显著变化。
传统分子靶向治疗方法主要集中在诸如点突变、基因缺失和重排等基因的结构变化,这些改变参与了胶质瘤的发生及演进,对其诊断、治疗及预后判断也具有重要的作用。例如,胶质瘤中出现的各种基因改变(如EGFR扩增、PTEN损失、PDGFRA扩增)可导致受体酪氨酸激酶信号增强和PI3K/AKT通路的失调,从而刺激葡萄糖摄取和有氧糖酵解。在Ⅱ级和Ⅲ级星形细胞瘤、少突神经胶质瘤和胶质母细胞瘤中70%都存在NADP+依赖性酶异柠檬酸脱氢酶1(socitrate dehydrogenase 1,IDH1)的突变。IDH1催化氧化胞质内异柠檬酸脱羧生成 α-酮戊二酸(α-KG)。IDH1突变改变了细胞代谢,其代谢产物2-羟戊二酸(2-HG)的积累会在肿瘤的发生发展中发挥作用.
转录/翻译水平上的基因表达的调控机制是癌症研究中最新兴的领域。最近的研究[8-9]表明恶性转化是由遗传变异和表观遗传学改变的复杂相互作用所致的,从而影响各种细胞生物学过程的变化,包括细胞增殖和侵袭、DNA修复、凋亡、血管生成和细胞周期调控,最终导致肿瘤形成。
表观遗传学的现象很多,已知的有DNA甲基化、基因组印记、母体效应、基因沉默、核仁显性、休眠转座子激活以及RNA编辑等。DNA甲基化是恶性胶质瘤中研究最广泛的表观遗传现象。组蛋白是核小体形成过程中所必需的蛋白质。每一个核小体由约147个DNA碱基对缠绕在组蛋白八聚体上,组蛋白八聚体由H2A、H2B、H3和H4组成。组蛋白氨基酸的尾巴可以接受各种翻译后修饰如乙酰化、甲基化、磷酸化、泛素化和精氨酸(R)和赖氨酸(K)残基类泛素化。组蛋白赖氨酸残基的乙酰化作用通常激活转录,而甲基化(H3K9、H3K27、H4K20、H3K4 甲基化)可以激活或抑制转录相关因子。
1 DNA甲基化
研究最多的表观遗传修饰是胞嘧啶甲基化,在哺乳动物细胞中,DNA甲基化主要发生在胞嘧啶残基上,其次是鸟嘌呤。DNA甲基化是由DNMT(DNA甲基转移酶)家族的催化转移S-腺苷甲硫氨酸的甲基到DNA上。到目前为止,五个DNMT家族成员已被确定,分别为 DNMT1、DNMT2、DNMT3a、DNMT3b 和DNMT3L。DNA甲基化与转录活性相关。众所周知,在人类的癌症中DNA甲基化谱在肿瘤发生和进展中扮演着重要角色[15-16]。
人神经胶质瘤表现出甲基化模式的肿瘤典型变化[17-20]。低甲基化主要发生在 DNA 重复区域,并可通过激活致癌基因和增加基因组不稳定性来促进肿瘤生长。高甲基化主要发生在基因启动子CpG岛上,参与肿瘤形成和进展的过程,这些基因大都与肿瘤抑制[21-22]、 DNA 修复[23]、 细胞周期调控[24]、 凋亡[25-26]、侵袭[27-28]和迁移[29]相关(表 1)。 有趣的是,胶质瘤分级不同甲基化模式也不同,在胶质瘤WHO的Ⅱ级,Ⅲ级和Ⅳ级之间基因的甲基化的状态也呈现出明显差异[30]。
在癌症基因组图谱(the cancer genome atlas,TCGA)项目的框架内,Noushmehr等[6]研究甲基化谱分析确定了GBM肿瘤表型,其特征在于大量基因位点的协同高甲基化,被称为G-CIMP。G-CIMP与延长生存期以及基因表达谱(突变表达模式)有关[31]。此外,发现IDH突变导致酶活性的变化,α-KG产生减少,产生代谢物2-羟基戊二酸(2-HG),其竞争性地抑制调节DNA和组蛋白甲基化的酶的活性(α-KG依赖性双加氧酶),包括组蛋白脱甲基酶[32]和TET5mC羟化酶家族[33-35]。 TET 蛋白能通过转化 5-甲基胞嘧啶(5mC)至5-羟甲基胞嘧啶(5hmC)改变DNA甲基化状态。5hmC的生物学功能尚未得到确凿的阐明。与正常脑相比,在人类胶质瘤中,5hmC显著减少,并且已经有研究显示5hmC水平与细胞增殖之间呈现反比关系[36-37]。这些发现揭示了基因调节的另一种水平,并证明与胶质瘤发生中遗传和表观遗传密切相关[38-39]。
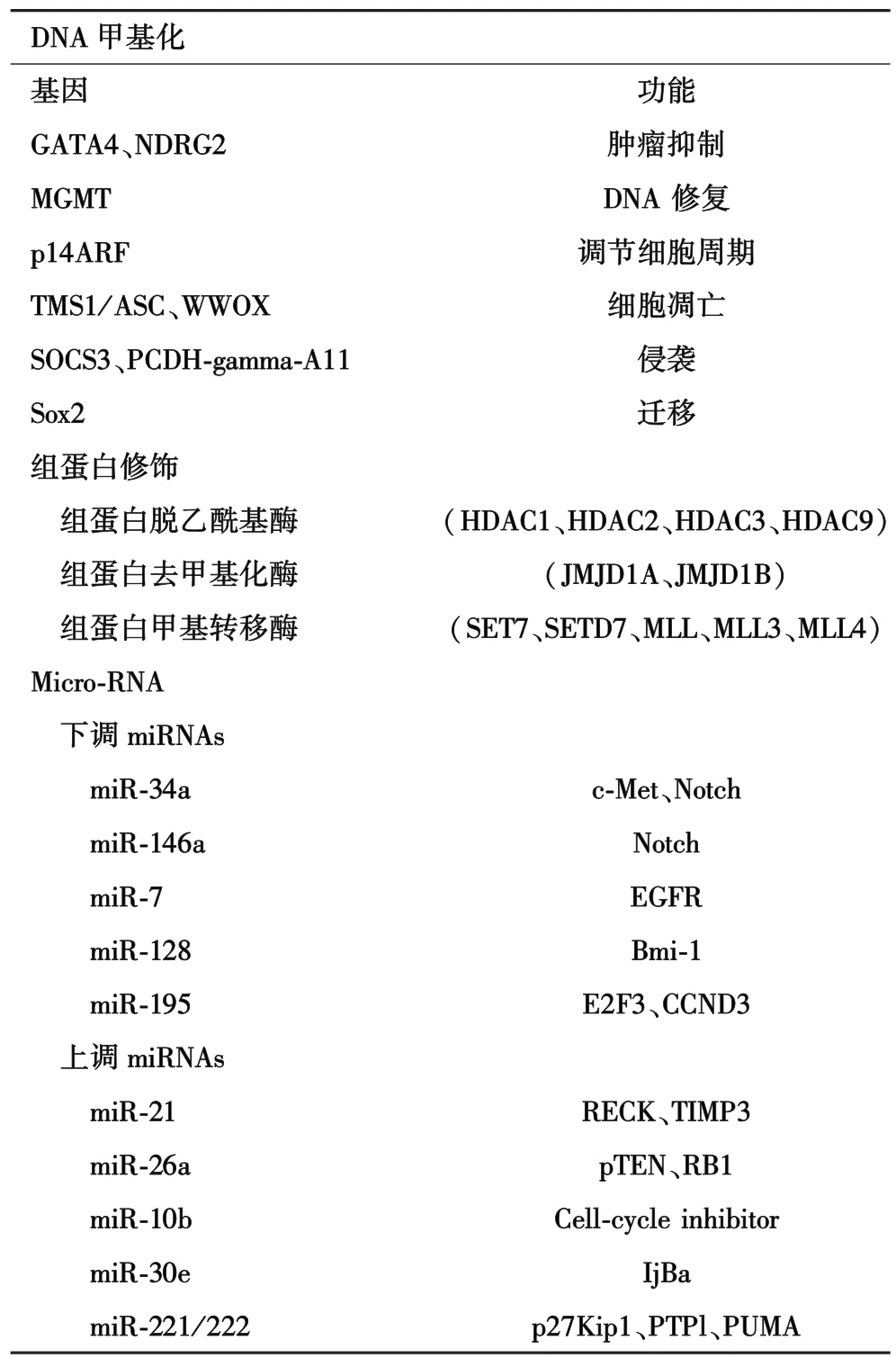
表1 人类胶质瘤中主要的表观遗传改变
在过去十年中,关于DNA甲基化过程的研究发现了许多肿瘤重要的生物标志物。O6-甲基鸟嘌呤-DNA甲基转移酶(methylguanine methyl transferase,MGMT)是一种DNA修复酶,其去除鸟嘌呤O6位置的烷基加合物,从而保护正常细胞免受致癌物质的侵害,相反的是,MGMT也可以来保护接受化疗的肿瘤细胞。MGMT表达可以通过启动子甲基化进行表观遗传沉默,这种情况出现在35%~45%的恶性胶质瘤和80%的WHOⅡ级胶质瘤中[40-41]。启动子甲基化状态已被确定为恶性胶质瘤患者进行烷基化剂化疗中治疗效果明显且独立的预测因子。通常与未甲基化的MGMT启动子相比,存在MGMT启动子甲基化形式的患者用替莫唑胺治疗效果更加显著[42-43]。这说明MGMT启动子甲基化状态已被确定为神经肿瘤学的重要临床标志物。然而不是所有MGMT启动子甲基化的患者在替莫唑胺治疗后均有显著的治疗效果。在这些患者中,已经发现MGMT启动子甲基化和MGMT的mRNA表达不一致,不论MGMT启动子甲基化或是未甲基化,在25%的胶质母细胞瘤中检测到MGMT的mRNA表达异常;携带低转录活性的MGMT患者具有更好的治疗效果,这一结果与MGMT启动子甲基化结果正好相反,这种不一致的基本机制尚不清楚。我们假设,MGMT低表达水平与未甲基化的启动子组合的情况可能由转录物不稳定和/或转录抑制因子如miRNA调节或组蛋白修饰引起[44]。
2 组蛋白修饰
染色质是细胞核中DNA和组蛋白的缩合形式。在真核生物中,染色质由147个碱基对的DNA组成,紧紧缠绕在两个拷贝的四个核心组蛋白H2A,H2B,H3和H4八聚体周围的。
所得到的核小体是染色质的基础重复单元[45]。由于每个核心组蛋白具有从核小体突出的氨基末端“尾”,组蛋白,特别是其尾巴可能存在一定数量的翻译后修饰。组蛋白修饰包括乙酰化、甲基化和磷酸化,但也存在研究较少的修饰,如泛素化、ADP核糖基化、脱氨基和脯氨酸异构化[46]。这些组蛋白修饰中的每一种都能够影响染色质结构,从而导致DNA修复以及基因转录的改变。组蛋白修饰可以广泛地分为主动标记和被动标记。特别是组蛋白乙酰化和甲基化在致癌机制中发挥显著作用[15,47]。
赖氨酸残基的乙酰化由组蛋白乙酰转移酶(HATs)和组蛋白脱乙酰酶(HDAC)的相反作用调节。乙酰化中和赖氨酸残基的正电荷,从而削弱DNA和组蛋白尾部之间的键。因此,组蛋白乙酰化与转录激活相关,而脱乙酰化通常与抑制转录有关。组蛋白甲基化主要发生在赖氨酸和精氨酸的侧链上,其影响转录机制的效应蛋白的活性。组蛋白甲基化可以激活(例如 H3K4me2、H3K4me3)或抑制(H3K9me2,H3K27me3)转录,这取决于各自的甲基化位点[48-50]。
组蛋白表达水平的改变也可能在胶质瘤发生中发挥作用。这些改变包括参与组蛋白修饰的基因的异常表达以及各基因的组蛋白修饰模式的变化(表1)。组蛋白水平的畸变来源于调节基因突变,如GBM(包括HDAC2和HDAC9),组蛋白去甲基化酶(JMJD1A和 JMJD1B),组蛋白甲基转移酶(SET7、SETD7、MLL、MLL3 和 MLL4)[5]。 此外,HDAC 的表达水平的改变已被报道与肿瘤复发和进展相关(HDAC1、HDAC2 和 HDAC3)[51-52]。 在几项研究中已经报道了组蛋白修饰调节单个基因。例如,抑制肿瘤抑制因子RRP22和细胞周期调节因子p21的表达以及促增殖转录因子HOXA9的增强表达与组蛋白修饰模式的改变相关[53-55]。 但是,组蛋白修饰实际功能在胶质瘤中的作用及其作为生物标志物和/或治疗靶标的潜力仍有待充分阐明。
3 MicroRNAs
近来已发现非编码RNA在基因表达的表观遗传调控中起重要作用[56-57]。其中miRNA是约22个核苷酸(nt)长度的双链RNA分子,起源于人类基因组转录物前体。通过结合目标mRNA的3’-UTR内的特异性识别序列,抑制翻译或mRNA降解调节基因表达[58-59]。 目标识别主要通过 miRNA 的 5’区域的8个核苷酸短序列的碱基配对进行介导[60]。虽然一些miRNA调节特定的目标,但是来自多个研究的证据表明某些关键的miRNA可以调节高达几百个靶基因,并且许多类型的 miRNA 协同调节其靶标[61-62]。研究人员使用计算预测方法和不同测序技术相结合等技术手段,已经确定了大量的调节分子[63-64]。 目前发布的mirbase数据库,存在超过140种物种中含有的超过17,000个成熟miRNA序列[65]。最近的研究[66]表明大部分的转录组受到miRNAs调控。这些结论说明miRNA表达的调节异常与病理学特征及其预后相关联。
已经在许多类型的人类肿瘤中检测出miRNA的异常表达,包括神经胶质瘤[67-68]。 然而,miRNA 不仅仅作为肿瘤抑制因子起作用,而且还依赖靶向mRNA的功能作为一种癌基因[69-71]。 因此,改变的 miRNA表达水平会对致癌过程产生重大影响。与正常细胞相比,miRNA在恶性肿瘤中的差异表达的原因尚未完全阐明。然而,miRNA的转录调控序列中的表观遗传修饰以及基因突变,基因组缺失或基因扩增等遗传改变可能影响miRNA成熟和/或与mRNA靶标相互作用[72-74]。
在GBM中,高通量分析已经确定了miRNA的差异表达[75-77]。因此,miRNA被认为是GBM多重生物学特征的重要介质,包括细胞增殖、G1/S细胞周期进程、细胞存活、细胞迁移和细胞侵袭[78]。尽管尚未阐明神经胶质瘤复杂网络中miRNA的确切功能,但越来越多的研究集中于miRNA在神经胶质瘤发生和进展过程中的不同功能(表1)。例如,与正常脑相比,在神经胶质瘤中下调的miRNA已经被发现通过直接靶向致癌基因 c-Met、Notch[79-80]、Bmi-1[76]、表皮生长因子受体[81]、受体酪氨酸激酶[82]和细胞周期成分[83]发挥抑癌作用。相反,在胶质瘤中具有高表达的miRNA可能被确定为致癌基因,例如miR-21通过靶向基质金属蛋白酶的调节剂,miR-26a靶向PTEN和miR-10b 靶向细胞周期抑制剂[84-90]。
4 表观遗传网络
表观遗传调节途径通过相互作用形成复杂的调控网络:①miRNA本身的表达可以通过由组蛋白和/或DNA甲基化的共价修饰引起的染色质结构的变化来修饰[91-92]。②肿瘤可以相互利用 miRNA来靶向表观遗传。例如,发现miR-29b在急性骨髓性白血病中靶向DNMT3a和3b,miR-449a控制前列腺癌细胞中的HDAC1。在人神经胶质瘤中,miR-185最近被证实作为DNMT1的调节因子,其过表达导致整体DNA 低甲基化[93-95]。 此外,已经发现 miR-101 靶向组蛋白甲基转移酶EZH2且在人类GBM中下调,从而促进肿瘤生长[96-97]。③组氨酸修饰酶可能被CpG高甲基化沉默。例如,NSD1基因编码参与染色质调节的组蛋白甲基转移酶,其沉默导致组蛋白残基H4K20和H3K36的甲基化减少,同时又导致致癌基因MEIS1的活化[98]。我们需要在全基因组范围进一步研究,以充分阐明神经胶质瘤中的表观遗传模式,这将为阐明胶质瘤等高度异质性肿瘤的表观遗传学网络的复杂模式提供理论依据[99]。
5 结论与展望
分子生物标志物的研究进展改变了目前在世界卫生组织分类框架内的诊断精确度,同时有利于揭示相同WHO级别但是不同预后和治疗反应的神经胶质瘤亚群之间的差异[2]。1p/19共缺失检测与化疗和/或放疗后的预后结果相关[100-101]。 筛查 IDH1/2突变有助于区分来自弥漫性星形细胞瘤的WHOⅠ级毛细胞星形细胞瘤和室管膜瘤(不含IDH突变)。IDH突变与间变性星形细胞瘤和胶质母细胞瘤的良好预后相关[102-103]。 鉴于在实际病例中Ⅱ~Ⅳ级神经胶质瘤难以进行完全肿瘤切除,不完全切除术通常不能获得相应的预后效果,微创分子表征策略的发展受到越来越多的关注[104]。最近,组织病理学诊断与新颖的分子立体定向活检程序相结合已经在DNA和RNA水平上实现高度可重复和有效的结果;MGMT启动子甲基化,MGMT mRNA表达以及TP53突变状态和1p/19q-状态的信息可以从1 mm3的立体定向组织样品中精确定义的位点收集[105-106]。
引入大规模的“二代”测序(next-generation sequencing,NGS)技术手段标志着基因组研究革命的开始[107]。目前,全基因组、转录组和甲基化测序在很小的肿瘤组织样本中也可以进行研究。NGS平台提供了对基因组和表观基因组更加全面的理论支持,并且基于NGS的数据的整合对于了解和鉴定神经胶质瘤的发生和发展的细胞内途径的致密网络是至关重要的[108]。随着NGS技术的成本下降和生物信息数据处理的改善,对于同一生物样品的转录组和遗传变异相结合的多个表观遗传修饰的基因组测序可能成为未来的临床研究方法。在这种情况下,通过微创方法(如分子立体定向程序)收集肿瘤样本将是特别有价值的。从这种方法获得的信息可以为每名患者创建个性化的治疗方案。将胶质瘤中研究发现的表观遗传学现象应用到胶质瘤的早期诊断,高危人群的监测,肿瘤风险评估,判断肿瘤复发情况,预测肿瘤疗效和预后,开发特异新靶点药物等方面具有很大的潜力,相信随着检测手段和实验方法的日臻完善,胶质瘤预防、诊断和治疗等领域必将取得喜人的成果。
[1]Stupp R,Hegi ME,van den Bent MJ,et al.Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phaseⅢstudy:5-year analysis of the EORTC-NCIC trial[J].Lancet Oncol,2009,10(5):459-466.
[2]Westphal M,Lamszus K.The neurobiology of gliomas:from cell biology to the development of therapeutic approaches[J].Nat Rev Neurosci,2011,12(9):495-508.
[3]Kreth FW,Faist M,Grau S,et al.Interstitial 125I radiosurgery of supratentorial de novo WHO Grade 2 astrocytoma and oligoastrocytoma in adults:long-term results and prognostic factors[J].Cancer,2006,106(6):1372-1381.
[4]Ohgaki H,Kleihues P.Genetic alterations and signaling pathways in the evolution of gliomas[J].Cancer Sci,2009,100(12):2235-2241.
[5]Parsons DW,Jones S,Zhang X,et al.An integrated genomic analysis of human glioblastoma multiforme[J].Science,2008,321(5897):1807-1812.
[6]Noushmehr H,Weisenberger DJ,Diefes K,et al.Identification of a CpG island methylator phenotype that defines a distinct subgroup of glioma[J].Cancer Cell,2010,17(5):510-522.
[7]Network TC.Corrigendum:Comprehensive genomic characterization defines human glioblastoma genes and core pathways[J].Nature,2013,494(7438):506-510.
[8]Berdasco M,Esteller M.Aberrant epigenetic landscape in cancer:How cellular identity goes awry[J].Dev Cell,2010,19(5):698-711.
[9]Portela A,Esteller M.Epigenetic modifications and human disease.Nat Biotechnol 28:1057-1068[J].Nat Biotechnol,2010,28(10):1057-1068.
[10]Suvà ML.Genetics and epigenetics of gliomas[J].Swiss Med Wkly,2014,144:w14018.
[11]Suzuki MM,Bird A.DNA methylation landscapes:provocative insights from epigenomics[J].Nat Rev Genet,2008,9(6):465-476.
[12]Irizarry R A,Ladd-Acosta C,Wen B,et al.The human colon cancer methylome shows similar hypo-and hypermethylation at conserved tissue-specific CpG island shores[J].Nature Genetics,2009,41(2):178-186.
[13]Chen ZX,Riggs AD.DNA methylation and demethylation in mammals[J].J Biol Chem,2011,286(21):18347-18353.
[14]Hellman A,Chess A.Gene body-specific methylation on the active X chromosome[J].Science,2007,315(5815):1141-1143.
[15]Esteller M.Cancer epigenomics:DNA methylomes and histone-modification maps[J].Nat Rev Genet,2007,8(4):286-298.
[16]Venneti S,Thompson CB.Metabolic modulation of epigenetics in gliomas[J].Brain Pathol,2013,23(2):217-221.
[17]Yong RL,Tsankova NM.Emerging interplay of genetics and epigenetics in gliomas:a new hope for targeted therapy.[J].Semin Pediatr Neurol,2015,22(1):14-22.
[18]Cadieux B,Ching TT,Vandenberg SR,et al.Genome-wide hypomethylation in human glioblastomas associated with specific copy number alteration,methylenetetrahydrofolate reductase allele status,and increased proliferation[J].Cancer Res,2006,66(17):8469-8476.
[19]Martinez R,Martin-Subero JI,Rohde V,et al.A microarray-based DNA methylation study of glioblastoma multiforme[J].Epigenetics,2009,4(4):255-264.
[20]Wu X,Rauch TA,Zhong X,et al.CpG island hypermethylation in human astrocytomas.[J].Cancer Res,2010,70(7):2718-2727.
[21]Sameer A,Amparo W,Munoz DM,et al.A GATA4-regulated tumor suppressor network represses formation of malignant human astrocytomas[J].J Exp Med,2011,208(4):689-702.
[22]Tepel M,Roerig P,Wolter M,et al.Frequent promoter hypermethylation and transcriptional downregulation of the NDRG2,gene at 14q11.2 in primary glioblastoma[J].Int J Cancer,2008,123(9):2080-2086.
[23]Tsankova NM,Canoll P.Advances in genetic and epigenetic analyses of gliomas:a neuropathological perspective.[ J].J Neuro-Oncol,2014,119(3):481-490.
[24]Yang X,Yang L,Dai W,et al.Role of p14ARF and p15INK4B promoter methylation in patients with lung cancer:a systematic metaanalysis[J].Onco Targets Ther,2016,9:6977-6985.
[25]Stone AR,Bobo W,Brat DJ,et al.Aberrant methylation and downregulation of TMS1/ASC in human glioblastoma.[J].Am J Pathol,2004,165(4):1151-1161.
[26]Kosla K,Pluciennik E,Kurzyk A,et al.Molecular analysis of WWOX expression correlation with proliferation and apoptosis in glioblastoma multiforme[J].J Neurooncol,2011,101(2):207-213.
[27]Waha A,Güntner S,Huang TH,et al.Epigenetic silencing of the protocadherin family member PCDH-γ-all in astrocytomas 1 [ J].Neoplasia,2005,7(3):193-199.
[28]Lindemann C,Hackmann O,Delic S,et al.SOCS3 promoter methylation is mutually exclusive to EGFR amplification in gliomas and promotes glioma cell invasion through STAT3 and FAK activation[J].2011,122(2):241-251.
[29]Alonso MM,Diez-Valle R,Manterola L,et al.Genetic and epigenetic modifications of Sox2 contribute to the invasive phenotype of malignant gliomas[J].Plos One,2011,6(11):e26740.
[30]Mur P,Rodríguez de Lope Á,Díaz-Crespo FJ,et al.Impact on prognosis of the regional distribution of MGMT methylation with respect to the CpG island methylator phenotype and age in glioma patients[J].J Neurooncol,2015,122(3):441-450.
[31]Verhaak RG,Hoadley KA,Purdom E,et al.Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA,IDH1,EGFR,and NF1[J].Cancer Cell,2010,17(1):98-110.
[32]Lu C,Ward PS,Kapoor GS,et al.IDH mutation impairs histone demethylation and results in a block to cell differentiation[J].Nature,2012,483(7390):474-478.
[33]Dang L,White DW,Gross S,et al.Cancer-associated IDH1 mutations produce 2-hydroxyglutarate[J].Nature,2010,465(7300):966.
[34]Xu W,Yang H,Liu Y,et al.Oncometabolite 2-hydroxyglutarate is a competitive inhibitor of α-ketoglutarate-dependent dioxygenases[J].Cancer Cell,2011,19(1):17-30.
[35]Guo JU,Su Y,Zhong C,et al.Hydroxylation of 5-methylcytosine by TET1 promotes active DNA demethylation in the adult brain[J].Cell,2011,145(3):423-434.
[36]Jin SG,Jiang Y,Qiu R,et al.5-hydroxymethylcytosine is strongly depleted in human cancers but its levels do not correlate with IDH1 mutations[J].Cancer Res,2011,71(24):7360-7365.
[37]Kraus TF,Globisch D,Wagner M,et al.Low values of 5-hydroxymethylcytosine(5hmC),the “sixth base,”are associated with anaplasia in human brain tumors[J].Int J Cancer,2012,131(7):1577-1590.
[38]Figueroa ME,Abdel-Wahab O,Lu C,et al.Leukemic IDH1 and IDH2 mutations result in a hypermethylation phenotype,disrupt TET2 function,and impair hematopoietic differentiation[J].Cancer Cell,2010,18(6):553-567.
[39]Williams K,Christensen J,Pedersen MT,et al.TET1 and hydroxymethylcytosine in transcription and DNA methylation fidelity[J].Nature,2011,473(7347):343-348.
[40]Hegi ME,Diserens AC,Gorlia T,et al.MGMT gene silencing and benefit from temozolomide in glioblastoma[J].N Engl J Med,2005,352(10):997-1003.
[41]Thon N,Eigenbrod S,Kreth S,et al.IDH1,mutations in gradeⅡastrocytomas are associated with unfavorable progression-free survival and prolonged postrecurrence survival[J].Cancer,2012,118(2):452-460.
[42]Wick W,Hartmann C,Engel C,et al.NOA-04 randomized phaseⅢtrial of sequential radiochemotherapy of anaplastic glioma with procarbazine,lomustine,and vincristine or temozolomide[J].J Clin Oncol,2009,27(35):5874-5880.
[43]Stupp R,Mason WP,van den Bent MJ,et al.Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma[J].N Engl J Med,2005,352(10):987-996.
[44]Kreth S,Thon N,Eigenbrod S,et al.O-methylguanine-DNA methyltransferase(MGMT)mRNA expression predicts outcome in malignant glioma independent of MGMT promoter methylation.[J].PloS One,2011,6(2):e17156.
[45]Margueron D,Reinberg D.Chromatin Structure and the Inheritanceof Epigenetic Information[J].Nat Rev Genet,2010,11(4):285-296.
[46]Kouzarides T.Chromatin modifications and their function.[J].Cell,2007,128(4):693-705.
[47]Jbara M,Guttmann-Raviv N,Maity S K,et al.Total chemical synthesis of methylated analogues of histone 3 revealed KDM4D as a potential regulator of H3K79me3[J].Bioorganic& Medicinal Chemistry,2017.
[48]KarliR,Chung HR,Lasserre J,et al.Histone modification levels are predictive for gene expression[J].Proc Natl Acad Sci U S A,2010,107(7):2926-2931.
[49]Bannister AJ,Kouzarides T.Regulation of chromatin by histone modifications[J].Cell Res,2011,21(3):381-395.
[50]Araki Y,Tsuzuki Wada T,Aizaki Y,et al.Histone methylation and stat-3 differentially regulate interleukin-6-induced matrix metalloproteinase gene activation in rheumatoid arthritis synovial fibroblasts[J].Arthritis Rheumatol,2016,68(5):1111-1123.
[51]Campos B,Bermejo JL,Han L,et al.Expression of nuclear receptor corepressors and class I histone deacetylases in astrocytic gliomas[J].Cancer Sci,2011,102(2):387-392.
[52]Lucio-Eterovic AK,Cortez MA,Valera ET,et al.Differential expression of 12 histone deacetylase(HDAC)genes in astrocytomas and normal brain tissue:classⅡand IV are hypoexpressed in glioblastomas[J].BMC Cancer,2008,8:243.
[53]Schmidt N,Windmann S,Reifenberger G,et al.DNA hypermethylation and histone modifications downregulate the candidate tumor suppressor gene RRP22 on 22q12 in human gliomas[J].Brain Pathol,2012,22(1):17-25.
[54]Mottet D,Pirotte S,Lamour V,et al.HDAC4 represses p21(WAF1/Cip1)expression in human cancer cells through a Sp1-dependent,p53-independent mechanism [J].Oncogene,2009,28(2):243-256.
[55]Costa BM,Smith JS,Chen Y,et al.Reversing HOXA9 oncogene activation by PI3K inhibition:epigenetic mechanism and prognostic significance in human glioblastoma[J].Cancer Res,2010,70(2):453-462.
[56]Costa FF.Non-coding RNAs,epigenetics and complexity[J].Gene,2008,410(1):9-17.
[57]Esteller M.Non-coding RNAs in human disease[J].Nat Rev Genet,2011,12(12):861-874.
[58]Maldonado L,Hoque MO.Epigenomics and ovarian carcinoma[J].Biomark Med,2010,4(4):543-570.
[59]Mendell JT.MicroRNAs:critical regulators of development,cellular physiology and malignancy[J].Cell Cycle,2005,4(9):1179-1184.
[60]Lewis BP,Burge CB,Bartel DP.Conserved seed pairing,often flanked by adenosines,indicates that thousands of human genes are microrna targets[J].Cell,2005,120(1):15-20.
[61]Bose M,Barman B,Goswami A,et al.Spatiotemporal uncoupling of miRNA-mediated translational repression and target RNA degradation controls miRNP recycling in mammalian cells[J].Mol Cell Biol,2017,37(4):e00464-e004616.
[62]Wang H.Predicting MicroRNA biomarkers for cancer using phylogenetic tree and microarray analysis[J].Int J Mol Sci,2016,17(5):773-786.
[63]John B,Sander C,Marks DS.Prediction of human microRNA targets[J].Methods Mol Biol,2006,342:101-113.
[64]Gunaratne PH,Coarfa C,Soibam B,et al.miRNA data analysis:next-gen sequencing[J].Methods Mol Biol,2012,822:273-288.
[65]Kozomara A,Griffiths-Jones S.miRBase:integrating microRNA annotation and deep-sequencing data[J].Nucleic Acids Res,2010,39(Database issue):D152-D157.
[66]Selbach M,Schwanhäusser B,Thierfelder N,et al.Widespread changes in protein synthesis induced by microRNAs[J].Nature,2008,455(7209):58-63.
[67]Soifer HS,Rossi JJ,Saetrom P.MicroRNAs in disease and potential therapeutic applications[J].Mol Ther,2007,15(12):2070-2079.
[68]Croce CM.Causes and consequences of microRNA dysregulation in cancer[J].Nat Rev Genet,2009,10(10):704-714.
[69]Carninci P,Kasukawa T,Katayama S,et al.The transcriptional landscape of the mammalian genome[J].Science,2005,309(5740):1559-1563.
[70]Lee YS,Dutta A.MicroRNAs:small but potent oncogenes or tumor suppressors[J].Curr Opin Investig Drugs,2006,7(6):560-564.
[71]Chen CZ.MicroRNAs as oncogenes and tumor suppressors[J].Devel Biol,2007,302(1):1-12.
[72]Calin GA,Croce CM.MicroRNAs and chromosomal abnormalities in cancer cells.[J].Oncogene,2006,25(46):6202-6210.
[73]Kumar MS,Lu J,Mercer KL,et al.Impaired microRNA processing enhances cellular transformation and tumorigenesis[J].Nat Genet,2007,39(5):673-677.
[74]Lujambio A,Esteller M.CpG island hypermethylation of tumor suppressor microRNAs in human cancer[J].Cell Cycle,2007,6(12):1455-1459.
[75]Kim H,Huang W,Jiang X,et al.Integrative genome analysis reveals an oncomir/oncogene cluster regulating glioblastoma survivorship[J].Proc Natl Acad Sci U S A,2010,107(5):2183-2188.
[76]Godlewski J,Nowicki MA,Williams S,et al.Targeting of the Bmi-1 oncogene/stem cell renewal factor by microRNA-128 inhibits glioma proliferation and self-renewal[J].Cancer Res,2008,68(22):9125-9130.
[77]Gaur A,Jewell DA,Liang Y,et al.Characterization of microrna expression levels and their biological correlates in human cancer cell lines[J].Cancer Res,2007,67(6):2456-2468.
[78]Pang JC,Kwok WK,Chen Z,et al.Oncogenic role of microRNAs in brain tumors[J].Acta Neuropathol,2009,117(6):599-611.
[79]Li Y,Guessous F,Zhang Y,et al.MicroRNA-34a inhibits glioblastoma growth by targeting multiple oncogenes[J].Cancer Res,2009,69(19):7569-7576.
[80]Mei J,Bachoo R,Zhang CL.MicroRNA-146a inhibits glioma development by targeting notch1[J].Mol Cell Biol,2011,31(17):3584-3592.
[81]Kefas B,Godlewski J,Comeau L,et al.microRNA-7 inhibits the epidermal growth factor receptor and the Akt pathway and is down-regulated in glioblastoma[J].Cancer Res,2008,68(10):3566-3572.
[82]Papagiannakopoulos T,Friedmann-Morvinski D,Neveu P,et al.Pro-neural miR-128 is a glioma tumor suppressor that targets mito-genic kinases[J].Oncogene,2011,31(15):1884-1895.
[83]Zhang QQ,Xu H,Huang MB,et al.MicroRNA-195 plays a tumorsuppressor role in human glioblastoma cells by targeting signaling pathways involved in cellular proliferation and invasion[J].Neuro-Oncology,2012,14(3):278-287.
[84]Gabriely G,Yi M,Narayan RS,et al.Human glioma growth is controlled by microRNA-10b[J].Cancer Res,2011,71(10):3563-3572.
[85]Gabriely G,Wurdinger T,Kesari S,et al.MicroRNA 21 promotes glioma invasion by targeting matrix metalloproteinase regulators[J].Mol Cell Biol,2008,28(17):5369-5380.
[86]Huse JT,Brennan C,Hambardzumyan D,et al.The PTEN-regulating microRNA miR-26a is amplified in high-grade glioma and facilitates gliomagenesis[J].Genes Dev,2009,23(11):1327-1337.
[87]Jiang L,Lin C,Song L,et al.MicroRNA-30e*promotes human glioma cell invasiveness in an orthotopic xenotransplantation model by disrupting the NF-κB/IκBα negative feedback loop[J].J Clin Invest,2012,122(1):33-47.
[88]Quintavalle C,Garofalo M,Zanca C,et al.miR-221/222 overexpession in human glioblastoma increases invasiveness by targeting the protein phosphate PTPμ[J].Oncogene,2012,31(7):858-868.
[89]Zhang CZ,Zhang JX,Zhang AL,et al.MiR-221 and miR-222 target PUMA to induce cell survival in glioblastoma[J].Mol Cancer,2010,9:229.
[90]Lorimer IA.Regulation of p27Kip1 by miRNA 221/222 in glioblastoma[J].Cell Cycle,2009,8(17):2685.
[91]Saito Y,Liang G,Egger G,et al.Specific activation of microRNA-127 with downregulation of the proto-oncogene BCL6 by chromatinmodifying drugs in human cancer cells.[ J].Cancer Cell,2006,9(6):435-443.
[92]Lujambio A,Ropero S,Ballestar E,et al.Genetic unmasking of an epigenetically silenced microRNA in human cancer cells.[J].Cancer Res,2007,67(4):1424-1429.
[93]Garzon R,Liu S,Fabbri M,et al.MicroRNA-29b induces global DNA hypomethylation and tumor suppressor gene reexpression in acute myeloid leukemia by targeting directly DNMT3A and 3B and indirectly DNMT1[J].Blood,2009,113(25):6411-6418.
[94]Noonan EJ,Place RF,Pookot D,et al.miR-449a targets HDAC-1 and induces growth arrest in prostate cancer[J].Oncogene,2009,28(14):1714-1724.
[95]Zhang Z,Tang H,Wang Z,et al.MiR-185 targets the DNA methyltransferases 1 and regulates global DNA methylation in human glioma[J].Mol Cancer,2011,10(1):1-16.
[96]Varambally S,Cao Q,Mani RS,et al.Genomic loss of microRNA-101 leads to overexpression of histone methyltransferase EZH2 in cancer[J].Science,2008,322(5908):1695-1699.
[97]Smits M,Nilsson J,Mir SE,et al.miR-101 is down-regulated in glioblastoma resulting in EZH2-induced proliferation,migration,and angiogenesis[J].Oncotarget,2010,1(8):710-720.
[98]Berdasco M,Ropero S,Setien F,et al.Epigenetic inactivation of the Sotos overgrowth syndrome gene histone methyltransferase NSD1 in human neuroblastoma and glioma[J].Proc Natl Acad Sci,2009,106(51):21830-21835.
[99]Wang M,Xie H,Stellpflug W,et al.BTECH:a platform to integrate genomic,transcriptomic and epigenomic alterations in brain tumors[J].Neuroinformatics,2011,9(1):59-67.
[100]van den Bent MJ,Brandes AA,Taphoorn MJ,et al.Adjuvant procarbazine,lomustine,and vincristine chemotherapy in newly diagnosed anaplastic oligodendroglioma:long-term follow-up of EORTC brain tumor group study 26951[J].J Clin Oncol,2013,31(3):344-350.
[101]Ohgaki H,Kleihues P.Genetic profile of astrocytic and oligodendroglial gliomas[J].Brain Tumor Pathol,2011,28(3):177-183.
[102]Kim Y H,Nobusawa S,Mittelbronn M,et al.Molecular classification of low-grade diffuse gliomas[J].Am J Pathol,2010,177(6):2708-2714.
[103]Stummer W,Pichlmeier U,Meinel T,et al.Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma:a randomised controlled multicentre phase Ⅲ trial[J].Lancet Oncology,2006,7(7):392-401.
[104]Thon N,Eigenbrod S,Grasbon-Frodl EM,et al.Novel molecular stereotactic biopsy procedures reveal intratumoral homogeneity of loss of heterozygosity of 1p/19q and TP53 mutations in World Health Organization grade Ⅱ gliomas[J].J Neuropathol Exp Neurol,2009,68(11):1219-1228.
[105]Thon N,Eigenbrod S,Grasbon-Frodl EM,et al.Predominant influence of MGMT methylation in non-resectable glioblastoma after radiotherapy plus temozolomide[J].J Neurol Neurosurg Psychiatry,2011,82(4):441-446.
[106]Mardis ER.A decade's perspective on DNA sequencing technology[J].Nature,2011,470(7333):198-203.
[107]Meaburn E,Schulz R.Next generation sequencing in epigenetics:insights and challenges[J].Semin Cell Dev Biol,2012,23(2):192-199.
[108]Riddick G,Fine HA.Integration and analysis of genome-scale data from gliomas[J].Nat Rev Neurol,2011,7(8):439-450.