Homeostatic relevance of vitamin D in maintaining male fertility in human: Downregulation of oxidative stress and up-regulation of anti-oxidative defense and steroidal hormones
Fahad Hussain, Arif Malik✉, Muhammad Saeed Qureshi, Muhammad Imran, Sulayman Waquar, Hassan Shafique, Zohaib Rana, Hnin Ei Thu, Zahid Hussain
1Institute of Molecular Biology and Biotechnology, The University of Lahore, Raiwind Road 55150, Lahore, Pakistan
2Department of Biochemistry, Akhtar Saeed Medical and Dental Collage, Lahore, Pakistan
3Department of Physiology, Nishtar Medical University, 66000, Multan, Pakistan
4Department of Biochemistry, University of Agriculture, Faisalabad, 38040, Pakistan
5Department of Pharmacology, Faculty of Medicine, Universiti Kebangsaan Malaysia, Jalan Yaacob Latif, Bandar Tun Razak, 56000, Cheras, Kuala Lumpur, Malaysia
6Department of Pharmaceutics, Faculty of Pharmacy, Universiti Teknologi MARA, Puncak Alam Campus, Bandar Puncak Alam 42300, Selangor,Malaysia
1. Introduction
Male infertility refers to a male’s inability to cause pregnancy in a fertile female. In humans it accounts for 40%–50% of infertility. It affects approximately 7% of all men. Male infertility is commonly due to deficiencies in the semen, and semen quality is used as a surrogate measure of male fecundity. Male infertility is associated with several types of endogenous and exogenous factors which result in the formation of defective sperms and thus affect the quality of life in human[1]. Among several factors, oxidative stress is one of the leading factors which influence sperm characteristics such as seminal volume, density, sperm motility, morphological featuresand their viability[2]. Male reproductive endocrine system majorly performs its biological functions via hypothalamus,anterior pituitary and testes axis. Male reproductive system contains epididymis, ductus deferens and testis. The common function of male reproductive system is to produce spermatozoa by regulating sex hormones. The anterior pituitary gland releases two types of hormonesvia the hypothalamus. These hormones are luteinizing hormone (LH) that initiates the process of testosterone production in leydig cells by the metabolism of cholesterol in mitochondria and endoplasmic reticulum and follicle-stimulating hormone (FSH) that initiates the process of spermatogenesis in sertoli cells with the help of testosterone[3]. The process of sperm production can be divided into three phases including diploid spermatogenesis proliferation,haploid spermatids occurring through spermatocytes meiosis and haploid spermatids differentiation during the process of sperm production. At the final stage of spermatogenesis, the round form of spermatids differentiates into elongated spermatozoa with tail and mid piece. During spermatogenesis, the condensed nucleuses are formed by the remodeling and compacting of chromatin. After this process, the basal compartment of seminiferous epithelium is filled with spermatozoa that release into seminiferous tubules, immature spermatocytes and spermatogonia. The seminiferous tubules are the main part of testis and also the site of sperm maturation and production[4].
Numerous studies have explored the role of vitamin D in upregulating the functioning of reproductive system. Their results presumably have a notable practical meaning in infertility treatment[5]. According to the National Health and Nutrition Examination Surveys within the North America, 36% of the American population is affected by deficiency of vitamin D over the past 10-15 years[6]. Deficiency of vitamin D (less than 20 ng/mL)and insufficient of vitamin-D (20-29 ng/mL) are linked with skeletal diseases like osteoporosis[7], reproductive disorders, osteomalacia and various chronic disorders such as autoimmune diseases like typeⅠdiabetes or multiple sclerosis, inflammatory bowel disease,hypertension leading to cardiovascular disturbance, heart failure,coronary artery disease, cancer include breast cancer, colon cancer,neurocognitive disorder including Alzheimer disease[6,8,9]. Vitamin D belongs to the family of steroid hormone. According to the photolytic mechanism, 7-Dehydrocholestrol binds with vitamin D-binding protein, migrates into hepatocytes and converted into 25(OH)D3 by the process of hydroxylation with the help of liver enzyme like 25-hydroxylase (CYP2R1). Then, finally it is converted into active vitamin D also known as 1, 25-dihydroxyvitamin-D with the action of kidney enzyme like 1-hydroxylase (CYP27B1) by hydroxylation process[10]. The active form of vitamin D plays its role in genome with the help of specific vitamin D nuclear receptor and may be non-genomic with the help of membrane vitamin D receptor that further activates secondary messenger system to signal transduction. Vitamin D receptor(VDR) is present in several types of tissue including intestine, immune cells parathyroid hormone,but it is not expressed in skeleton tissue[11]. The presence of VDR in testis, placenta, ovary, and uterus represents that vitamin D displayed regulatory activity in reproductive system. After the binding of ligand with specific receptor, the intracellular cascade reactions were initiated and induced the phosphorylation of receptor that linked with 9-cis retinoid receptor. The VDR/ 9-cis retinoid receptor heterodimer complexes and some other regulatory proteins include VDR–interacting proteins, co-regulator and co-activator. All of these components are involved in the transcription of specific region of mRNA also known as VDR response element[12,13].
Deficiency of vitamin D in serum is very common with an approximately 32% of healthy population in the United States.It has been associated with various health disorders such as cardiovascular diseases, cancer, bone health, neuropsycologic,infectious and reproductive disorders[14]. Deficiency of vitamin D may affect spermatogenesis indirectly because the normal levels of calcium have positive correlation with testosterone production in endoplasmic reticulum[15]. The concentration of vitamin D has shown positive affiliation with the concentration of androgen sex hormone in man[16,17]. It is suggested that deficiency of vitamin-D may alter the function of reproductive system by calcium-dependent mechanism[18]. Reactive oxygen species(ROS) also play major role in damaging the spermatozoa by the process of lipid peroxidation.In the presence of excess amount of ROS, the process of lipid peroxidation takes place in spermatozoa[19]. To counteract the action of ROS, a number of antioxidant mechanisms play important protective roles in spermatozoa such as glutathione peroxidase(GSH), catalase (CAT), vitamin E, ascorbic acid and superoxide dismutase(SOD)[20].
The present study was performed to investigate the biochemical relevance of vitamin D in male infertility. For that, the levels of sex hormones (LH, FSH, and testosterone), antioxidant defenses (SOD,CAT, and GSH), and oxidative stress markers [malondialdehyde(MDA) and nitric oxide (NO) species] in infertile males compared to healthy individuals were evaluated.
2. Materials and methods
2.1. Materials
Enzyme linked immunosorbent assay kits were purchased from Sigma Chemicals Co. St. Louis, MO, USA. All other chemicals and reagents were sourced from biochemical laboratories of University of Lahore, Pakistan.
2.2. Experimental design
There were two test groups of human male adults. The first group consisted of 145 human male adults diagnosed with male infertility.The second group consisted of 130 human healthy male adults used as control group.
2.3. Inclusion criteria
Male adults having all biochemical tests were normal; however,those who were diagnosed with male infertility were included in the present study.
2.4. Exclusion criteria
Male infertile adults suffering from diabetes mellitus, hypertension,myocardial infarction or any other hepatic, pulmonary pancreatic or renal diseases were excluded from the present study.
2.5. Collection of blood and separation of serum
The blood samples of all human male infertile and healthy individuals were collected from their venous vessels, and serum samples were separated from the blood samples by centrifugation at 4 000 revolutions/min for 10 min. The collected serum samples were then stored at -60 ℃ until further biochemical analyses.
2.6. Biochemical assays
2.6.1.Biochemical markers tested usingenzyme linked immunosorbent assay
The levels of isoprostanes F 2αα(pg/mL), 8-hydroxy-2´-deoxyguanosine (pg/mL), 4-hydroxynonenal (µmol/L), vitamin D(ng/mL), calcium (mg/dL), estradiol (pg/mL), FSH (mU/mL), LH(mU/mL), cortisol (µg/dL) and testosterone (ng/dL) were analyzed using enzyme linked immunosorbent assay methods.
2.6.2.Biochemical markers tested using spectrophotometric methods
To evaluate the biochemical relevance of levels of vitamin D with antioxidant defense and oxidative stress occurring in the infertile male adults compared to the healthy males, the serum samples of all human individuals were tested using spectrophotometric methods for estimation of SOD, MDA, CAT, GSH, NO, and inducible nitric oxide synthase (iNOS).
2.6.3.Biochemical markers tested using calorimetric method
Moreover, the biochemical difference between the infertile human males and healthy individuals was also assessed by measuring the levels of glutathione peroxidase (GPx) and glutathione reductase(GRx) in the serum samples of all individuals using the calorimetric methods.
2.7. Statistical analysis
Results were expressed as mean± standard deviation (mean ±SD). Statistical significance was determined by one way analysis of variance (one way ANOVA) and spearman correlation (two tailed)were used to correlate the different variables. The difference was considered significant when P<0.05.
3. Results
3.1. Relevance of oxidative stress and male infertility
Oxidative stress was one of the leading causes of inducing spermatozoa damage and male infertility. In this study, several critical markers of oxidative stress including MDA, NO, iNOS,isoprostanes F 2α, 8-hydroxy-2´-deoxyguanosine, 4-hydroxynonenal were evaluated. The results demonstrated that the levels of these oxidative stresses inducing markers were significantly increased in infertile male adults compared to healthy individuals (Table 1).
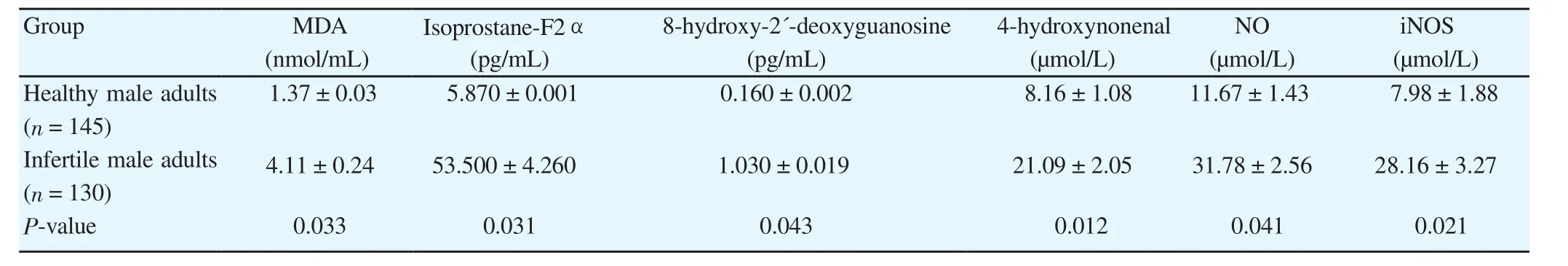
Table 1 Relevance of oxidative stress to male infertility in human individuals.
3.2. Relevance of antioxidant defense and male infertility
To prevent spermatozoa injury, human body adopted various physiologic anti-oxidative regulatory mechanisms including GSH,CAT, and SOD. These enzymes were capable of preventing damage to important cellular components caused by ROS such as free radicals, peroxides, and lipid peroxides. The study results indicated that the anti-oxidant defense was significantly reduced in infertile male adults compared to the healthy ale adults (Table 2).
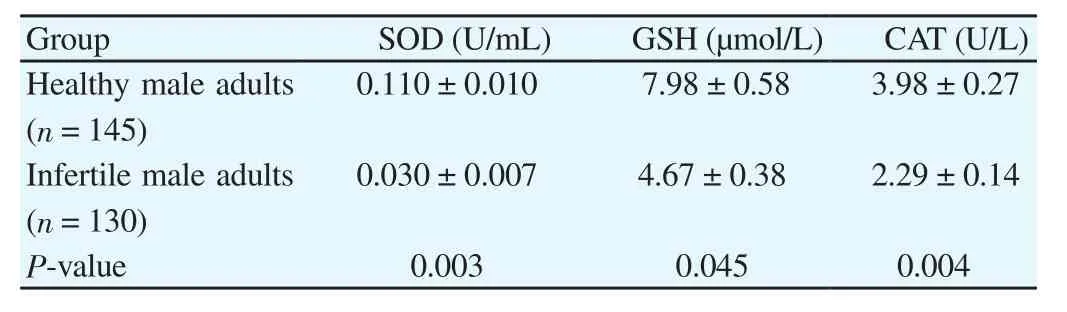
Table 2 Relevance of antioxidant defense to male infertility in human individuals.
3.3. Levels of vitamin D and calcium
The study results indicated that levels of vitamin D [(17.17±2.3) ng/mL] and calcium [(6.29±0.31) mg/dL] were also found to be lowered in infertile male adults compared tolevels of vitamin D[(36.26±3.09) ng/mL] and calcium [(9.33±0.62) ng/mL] in healthy individuals.
3.4. Levels of glutathione peroxidase (GPx) and glutathione reductase (GRx)
This study also estimated the levels of GPx and GRx in infertile male adults compared to healthy male adults. Results showed that the level of GPx [(5.88±0.21) µmol/L] and GRx [(2.87±0.21) µmol/L] were significantly lower in infertile male adults compared to the level of GPx [(7.87±0.48) µmol/L] and GRx [(5.53±0.15) µmol/L] in healthy individuals.
3.5. Relevance of steroidal hormones and male infertility
The levels of steroidal hormones including estradiol, cortisol, LH,FSH and testosterone were also measured in the present study (Table 3). Results demonstrated that the levels of steroidal hormones were significantly lowered in infertile male adults compared to healthy individuals.
4. Discussion
Male infertility is an inability of a male to cause pregnancy in a fertile female. Approximately 15% of population suffer infertility in both male and female. Male infertility occurs due to several exogenous and endogenous factors[21]. Vitamin-D deficiency has been associated with various reproductive problems including hypogonadism, infertility, miscarriage as well as preterm birth. ROS and reactive nitrogen species (RNS) are among the major factors that play key roles to damage spermatozoa by the process of lipid peroxidation[22]. Spermatozoa consist of low levels of anti-oxidative defense mechanism such as GPx, CAT, vitamin E, ascorbic acid and SOD[23]. Toxic levels of NO cause damage to the plasma membrane of sperms and catalyze the membrane into small fragments that are called MDA by the process of oxidation of polyunsaturated fatty acid. Specifically, the polyunsaturated fatty acid is very sensitive to the action of free radicals such as RNS and ROS[24,25]. Testosterone synthesizes by leydig cells and plays crucial roles in primary and secondary sex characteristics in males. Testosterone is regulated by the placental human chorionic gonadotropin and the production of testosterones is regulated by the secretion of LH from anterior pituitary gland in response to gonadotropic releasing hormone from hypothalamus. LH is involved in steroidogenesis by increasing the production of cyclic adenosine monophosphate and maintaining the concentration of calcium for the post translation modification of protein in ER leydig cell[26].The supplementation of vitamin D might be beneficial to increase the chance of pregnancy due to the production of testosterone in leydig cell by the stimulation of LH from anterior pituitary gland[27]. According to a previous study, the level of sex hormone-binding globulin exhibits positive correlation with vitamin D in young adults but not in older men[28].Calcium supplementation also restores fertility in male and female rats. Vitamin D regulates the homeostasis of calcium which have significant role in spermatogenesis in sertoli cells. Deficiency of vitamin D may alter the function of reproductive system by calciumdependent mechanism[29,30]. When the levels of calcium decreases in serum, mitochondrial calcium influx is increased, this may cause oxidative stress in mitochondria and ER. According to previousstudies, the normal sperm count, physiology, and morphology of sperm are regulated by the concentration of vitamin D[14]. The concentration of vitamin D showed a positive relationship with the concentration of androgen sex hormone in man by calcium depending mechanism[31,32]. The high levels of ROS and RNS induce adverse effects on the DNA and RNA as well as activate proapoptotic proteins to stimulate the process of apoptosis. The process of apoptosis increases with age due to imbalance between the production of free radicals and antioxidants activity, deficiency of vitamin D, sex hormones (LH, FSH) and cholesterol metabolism[33].
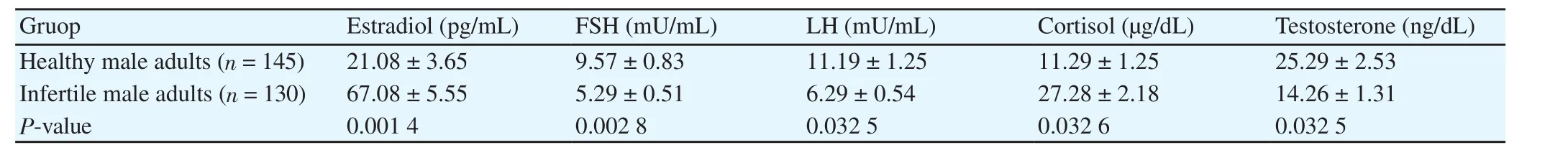
Table 3 Relevance of steroidal hormones to male infertility in human individuals.
The desire level of testosterone also triggers sertoli cells for spermatogenesis and maintains the count of sperm, sperm motility,sperm density, and maintains the volume of semen[34]. Vitamin D exhibits a positive correlation with the level of testosterone to improve cholesterol metabolism, antioxidant free radical scavenging activity, and reduce the production of free radicals[35,36]. Vitamin D is also necessary to maintain the levels of calcium in the leydig cells in order to regulate the testosterone levels and spermatogenesis to prevent the male infertility[37].
Conclusively, it is evident that vitamin D exhibits positive correlation with the male fertility by maintaining the levels of sex hormones (LH, FSH, and testosterone), up-regulating the antioxidant defense (SOD, CAT, and GSH), and down-regulating the oxidative stress (MDA, NO, and iNOS species) induced by ROS and RNS.Therefore, the levels of vitamin D are of prime importance in maintaining the sexual health of human.
Conflict of interest statement
The authors declare that they have no conflict of interest.
[1] Koppers AJ, Garg ML, Aitken RJ. Stimulation of mitochondrial reactive oxygen species production by unesterified, unsaturated fatty acids in defective human spermatozoa. Free Radic Biol Med 2010; 48(1): 112-119.
[2] Radi R. Peroxynitrite, a stealthy biological oxidant. J Biol Chem 2013;288(37): 26464-26472.
[3] Golan R, Scovell JM, Ramasamy R. Age-related testosterone decline is due to waning of both testicular and hypothalamic-pituitary function.Aging Male 2015; 18(3): 201-204.
[4] Chung SSW, Wang X, Wolgemuth DJ. Expression of retinoic acid receptor alpha in the germline is essential for proper cellular association and spermiogenesis during spermatogenesis. Development 2009; 136:2091-2100.
[5] Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA.National, regional, and global trends in infertility prevalence since 1990:A systematic analysis of 277 health surveys. PLoS Med 2012; 9(12):e1001356
[6] Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyviramin D status of the US population: 1998-1994 compared with 2000-2004. Am J Clin Nutr 2008; 88: 1519-1527.
[7] Lisse TS, Chun RF, Rieger S, Adams JS, Hewison M. Vitamin D activation of functionally distinct regulatory miRNAs in primary human osteoblasts. J Bone Miner 2013; 28: 1478-1488.
[8] Wacker M, Holick MF. Vitamin D effects on skeletal and extraskeletal health and the need for supplementation. Nutrients 2013; 5: 111-148.
[9] Rahman T, Hosen I, Islam MT, Shekhar HU. Oxidative stress and human health. Adv Biosci Biotechnol 2012; 3(7A): 25130.
[10] Christakos S, Dhawan P, Benn B, Porta A, Hediger M, Oh GT, et al.Vitamin D: Molecular mechanism of action. Ann N Y Acad Sci 2007;1116: 340-348.
[11] Lerchbaum E, Obermayer-Pietsch B. Vitamin D and fertility: A systematic review. Eur J Endocrinol 2012; 166(5): 765-778.
[12] Choudhary R, Chawala VK, Soni ND, Kumar J, Vyas RK. Oxidative stress and role of antioxidants in male infertility. Pak J Physiol 2010; 6:54-59.
[13] Haussler MR, Jurutka PW, Mizwicki M, Norman AW. Vitamin D receptor (VDR)-mediated actions of 1α, 25(OH)2vitamin D3: Genomic and non-genomic mechanisms. Best Pract Res Clin Endocrinol Metab 2011; 25: 543-559.
[14] Ramlau-Hansen CH, Moeller UK, Bonde JP, Olsen J, Thulstrup AM. Are serum levels of vitamin D associated with semen quality? Results from a cross-sectional study in young healthy men. Fertil Steril 2011; 95: 1000-1004.
[15] De Angelis C, Galdiero M, Pivonello C, Garifalos F, Menafra D, Cariati F, et al. The role of vitamin D in male fertility: A focus on the testis. Rev Endocr Metab Disord 2017; 18(3): 285-305.
[16] Wehr E, Pilz S, Boehm BO, Marz W, Obermayer-Pietsch B. Association of vitamin D status with serum androgen levels in men. Clin Endocrinol(Oxf) 2010; 73: 243-248.
[17] Jensen MB, Lawaetz JG, Andersson AM, Petersen JH, Nordkap L, Bang AK, et al. Vitamin D deficiency and low ionized calcium are linked with semen quality and sex steroid levels in infertile men. Hum Reprod 2016;31(8): 1875-1885.
[18] Bisht S, Faiq M, Tolahunase M, Dada R. Oxidative stress and male infertility. Nat Rev Urol 2017; 14(8): 470-485.
[19] Beattie MC, Adekola L, Papadopoulos V, Chen H, Zirkin BR. Leydig cell aging and hypogonadism. Exp Gerontol 2015; 68: 87-91.
[20] Agarwal A, Virk G, Ong C, du Plessis SS. Effect of oxidative stress on male reproduction. World J Mens Health 2014; 32(1): 1-17.
[21] Holick MF. The vitamin D deficiency pandemic: A forgotten hormone important for health. Public Health Rev 2010; 32: 267-283.
[22] Wright C, Milne S, Leeson H. Sperm DNA damage caused by oxidative stress: Modifiable clinical, lifestyle and nutritional factors in male infertility. Reprod Biomed Online 2014; 28(6): 684-703.
[23] Irani M, Merhi Z. Role of vitamin D in ovarian physiology and its implication in reproduction: A systematic review. Fertil Steril 2014; 102:460-468.
[24] Semenova AV, Tomilova IK, Panikratov KD, Kadykova EL, Basharin AV.The role of nitric oxide in fertility disorders in men. Urologiia 2005; 6:31-36.
[25] Hussain F, Malik A, Ayyaz U, Shafique H, Rana Z, Hussain Z. Efficient hepatoprotective activity of cranberry extract against CCl4-induced hepatotoxicity in Wistar albino rat model: Down-regulation of liver enzymes and strong antioxidant activity. Asian Pac J Trop Med 2017;10(11): 1054-1058.
[26] Rosario ER, Carroll JC, Pike CJ. Evaluation of the effects of testosterone and luteinizing hormone on regulation ofβ-amyloid in male 3xTg-AD mice. Brain Res 2012; 1466: 137-145.
[27] Lorenzen M, Boisen IM, Mortensen LJ, Lanske B, Juul A, Jensen MB.Reproductive endocrinology of vitamin D. Mol Cell Endocrinol 2017;453: 103-112.
[28] Wehr E, Pilz S, Boehm BO, Marz W, Obermayer-Pietsch B. Association of vitamin D status with serum androgen levels in men. Clin Endocrinol 2010; 73: 243-248.
[29] Hammoud AO, Meikle AW, Peterson CM, Stanford J, Gibson M,Carrell DT. Association of 25-hydroxy-vitamin D levels with semen and hormonal parameters. Asian J Androl 2012; 14: 855-859.
[30] Chandra AK, Sengupta P, Goswami H, Sarkar M. Excessive dietary calcium in the disruption of structural and functional status of adult male reproductive system in rat with possible mechanism. Mol Cell Biochem 2012; 364: 181-191.
[31] Jensen MB. Vitamin D and male reproduction. Nat Rev Endocrinol 2014;10(3): 175-186.
[32] Lerchbaum E, Obermayer-Pietsch B. Vitamin D and fertility: Asystematic review. Eur J Endocrinol 2012; 166: 765-778.
[33] Shima Y, Miyabayashi K, Haraguchi S, Arakawa T, Otake H, Baba T, et al. Contribution of leydig and sertoli cells to testosterone production in mouse fetal testes. Mol Endocrinol 2013; 27(1): 63-73.
[34] Shukla KK, Mahdi AA, Rajender S. Apoptosis, spermatogenesis and male infertility. Front Biosci (Elite Ed) 2012; 4: 746-754.
[35] Doshi SB, Khullar K, Sharma RK, Agarwal A. Role of reactive nitrogen species in male infertility. Reprod Biol Endocrinol 2012; 10: 109.
[36] Makker K, Agarwal A, Sharma R. Oxidative stress & male infertility.Indian J Med Res 2009; 129(4): 357-367.
[37] Raucci F, D’Aniello A, Di Fiore MM. Stimulation of androgen production by D-aspartate through the enhancement of StAR, P450scc and 3β-HSD mRNA levels in vivo rat testis and in culture of immature rat Leydig cells. Steroids 2014; 84: 103-110.
 Asian Pacific Journal of Reproduction2018年2期
Asian Pacific Journal of Reproduction2018年2期
- Asian Pacific Journal of Reproduction的其它文章
- Effect of tris-extender supplemented with various concentrations of strawberry(Fragaria spp.) on bull semen preservability
- Sperm counts in Asian men: Reviewing the trend of past 50 years
- Effect of exogenous progesterone on cumulus characteristics of buffalo oocytes by allowing passage of more number of sperm through cumulus but not essentially fertilization
- Improvement in cryosurvival of buffalo bull (Bubalus bubalis) sperm by altering freezing rate within critical temperature range
- Effect of voltage-gated sodium channels blockers on motility and viability of human sperm in vitro
- Germline cells derived from mesenchymal stem cells, with the focus on Wharton's jelly
