Acupuncture plus bloodletting therapy for insomnia in blood stasis constitution: a clinical study
Kan Li-na (阚丽娜), Huang Na-na (黄娜娜), Chen Ya-jun (陈亚军), He Xi-jun (何希俊), Fan Min (范敏), Sun Zhao (孙曌)
1 Zhongshan Municipal Hospital of Traditional Chinese Medicine, Guangzhou University of Chinese Medicine, Guangdong 528400,China
2 College of Traditional Chinese Medicine, Hainan Medical University, Hainan 571101, China
Insomnia, also named ‘inability to sleep’ in traditional Chinese medicine (TCM), has an incidence of 38.2%among Chinese adult population, according to the research of Chinese Sleep Research Society in 2012[1]. It seriously affects people’s quality of life (QOL) and work.Western medicine often treats insomnia with oral administration of benzodiazepines, but these drugs may Induce dependence or even resistance when taken for a long term. Acupuncture-moxibustion can produce a significant efficacy in treating insomnia without noticeable adverse reactions[2-3]. With the development of human society, medicine has gradually transferred its focus from ‘disease’ to ‘person’. In TCM theory, there are 9 types of body constitution[4], which provides criteria for body constitution differentiation in clinic. We adopted acupuncture plus bloodletting to treat insomnia in those with a blood stasis constitution. The report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria of Western medicine
The subjects all conformed to the diagnostic criteria for primary insomnia inDiagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV)[5]. The predominant complaint is difficulty initiating or maintaining sleep, for at least 1 month; the sleep disturbance causes distress or impairment in social,occupational or other areas of functioning; narcolepsy,breathing-related sleep disorder and circadian rhythm sleep disorder are excluded; the sleep disturbance is not due to major depressive disorder or generalized anxiety disorder, etc.; sleep disturbance caused by physiological problems, alcohol or drugs is excluded.
1.1.2 TCM diagnostic criteria
The TCM diagnostic criteria were based on the definition of inability to sleep inInternal Medicine of Traditional Chinese Medicine[6]: frequent inability to obtain normal sleep; majorly manifested by insufficient sleep duration or depth, with difficulty initiating sleep,nonrestorative sleep, waking multiple times or unable to go back to sleep after awakening in mild cases, or staying awake throughout the night in severe cases.1.1.3 Criteria for determining body constitution
According to the diagnostic criteria for blood stasis constitution in the self-rating scale of classification and diagnosis of body constitution of TCM[7]: bearing a potential tendency of blocked blood circulation or pathological basis of blood stagnation, and the main features including: dark complexion, pigmentation,petechia, purple lips, purple or spotted purple tongue,widened or dark-purple sublingual vessels, rough pulse;irritable and forgetful.
1.2 Inclusion criteria
Conforming to the above diagnostic criteria for primary insomnia; in accordance with the criteria for blood stasis constitution in TCM body constitution classification; age ranged between 18 and 70 years old,without limit of gender; not on any drugs or other treatments in the recent week.
1.3 Exclusion criteria
Insomnia induced by systematic disease (e.g. pain,fever) or external interruptions; pregnant or breastfeeding women; accompanied by severe primary diseases involving cardiovascular system, lungs, liver,kidney or hematopoietic system; mental disorders;those who faint during acupuncture or those allergic to the drugs used in this trial.
1.4 Statistical method
The SPSS 22 version statistical software was used for data analyses. The measurement data in normal distribution were expressed by mean ± standard deviation (x±s) and analyzed by two dependent samplest-test. The measurement data in abnormal distribution were expressed by mean (the first quartile,the third quartile) [M (Q1, Q3)], two independent sample rank-sum test for inter-group comparisons;rank-sum test for intra-group comparisons. The enumerations data were expressed by ratio and processed by Chi-square test. The comparison of therapeutic efficacy was analyzed byRidittest. The significance level wasα=0.05, andP<0.05 indicated that the difference was statistically significant.
1.5 General data
The 72 subjects in this study were all recruited from the Prevention Treatment Center of Zhongshan Municipal Hospital of Traditional Chinese Medicine,Guangzhou University of Chinese Medicine between January 2016 and January 2017. They were divided into a treatment group and a control group by using the random number table, 36 cases each. There were no dropouts in the two groups. In the treatment group, the age ranged from 18 to 53 years old, and the disease duration ranged from 1 month to 50 months. In the control group, the age ranged from 26 to 51 years old,and the disease duration ranged from 1 month to 72 months. There were no significant differences in the data of gender, age or disease duration between the two groups (allP>0.05), indicating the comparability(Table 1).
2 Treatment Methods
2.1 Treatment group
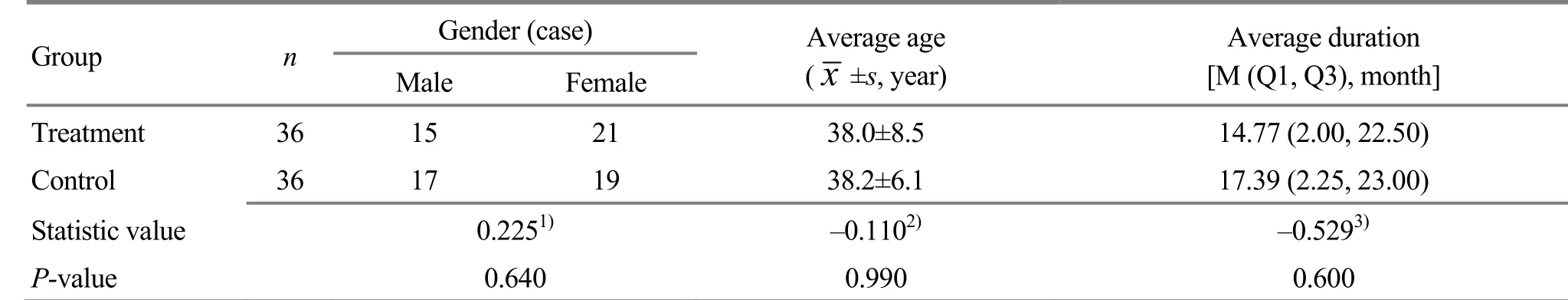
Table 1. Comparison of the general data
2.1.1 Acupuncture therapy
Acupoints: Baihui (GV 20) and bilateral Shenmen(HT 7), Sanyinjiao (SP 6), Zhaohai (KI 6), Shenmai (BL 62)and Anmian [Extra, locates at the midpoint between Yiming (EX-HN 14) and Fengchi (GB 20)].
Method: Patient took a supine position. After standard sterilization, the acupoints were punctured by filiform needles of 0.30 mm in diameter and 40 mm in length. The needles were retained for 30 min after needling qi was obtained. During the retaining, even reinforcing-reducing manipulation was applied once every 10 min.
2.1.2 Bloodletting therapy
Acupoint: Bilateral Geshu (BL 17) and Xinshu (BL 15).
Method: When acupuncture was finished, patient switched to a prone position. After sterilized by iodine,each acupoint was pricked 2-3 times by a three-edged needle, followed by cupping with cups retained for 3-5 min. The amount of bleeding was supposed to be 5-10 mL for each acupoint.
Treatment course: The acupuncture treatment was given once a day, 6 times a week; the bloodletting therapy was performed once a week. One-week treatment was taken as a course of treatment, and 3 successive courses were observed. A follow-up was done 3 months later.
2.2 Control group
Patients in the control group were intervened by oral administration of estazolam 30 min prior to sleep each night (batch number: 151102/T, Shandong Xinyi Pharmaceutical Co., Ltd., China), 1 mg per dose, once a day. The dose would be regulated to be 2 mg if the sleep quality did not show any improvement on the fourth day. The oral medication was taken once a day, 1 week as a course of treatment, for 3 successive courses in total. A follow-up study was conducted 3 months later.
3 Observation of Therapeutic Efficacy
3.1 Observation items
The scores of Pittsburgh sleep quality index (PSQI)[8]of the two groups were compared before and after the intervention, as well as in the follow-up. PSQI consists of subjective sleep quality, sleep latency, sleep duration,habitual sleep efficiency, sleep disturbances, use of sleep medication and daytime dysfunction. The global score of PSQI ranges from 0 to 21 points. The higher the score, the worse the sleep quality.
3.2 Criteria of therapeutic efficacy
The therapeutic efficacy was evaluated based on the reduction rate of PSQI score after the treatment[9].
Reduction rate of PSQI score = (Pre-treatment score -Post-treatment score) ÷ Pre-treatment score × 100%.
Recovered: Reduction rate of PSQI score ≥75%.
Markedly effective: Reduction rate of PSQI score≥50%, but <75%.
Effective: Reduction rate of PSQI score ≥25%, but<50%.
Invalid: Reduction rate of PSQI score <25%.
3.3 Treatment results
3.3.1 Comparison of PSQI score
There was no significant difference in PSQI score between the two groups before the intervention(P>0.05). The PSQI scores dropped significantly in both groups after the treatment (P<0.05); there was a significant difference in the global score of PSQI between the treatment group and control group(P<0.05), (Table 2).
3.3.2 Comparison of clinical efficacy
After the treatment, the total effective rate was88.9%in the treatment group, higher than 83.3% in the control group.Ridittest showedU=0.37 andP=0.03,indicating a significant difference between the two groups. It’s indicated that the therapeutic efficacy of acupuncture plus bloodletting therapy should be more marked than that of oral administration of estazolam(Table 3).
3.3.3 Comparison of the global score of PSQI in the 3-month follow-up study
The 3-month follow-up study showed that there was a significant difference in the global score of PSQI between the two groups according to two dependent samples rank-sum test (P<0.05), indicating that acupuncture plus bloodletting therapy can produce a more lasting efficacy in treating insomnia in a blood stasis body constitution (Table 4).

Table 2. Comparison of the global score of PSQI [M (Q1, Q3), point]
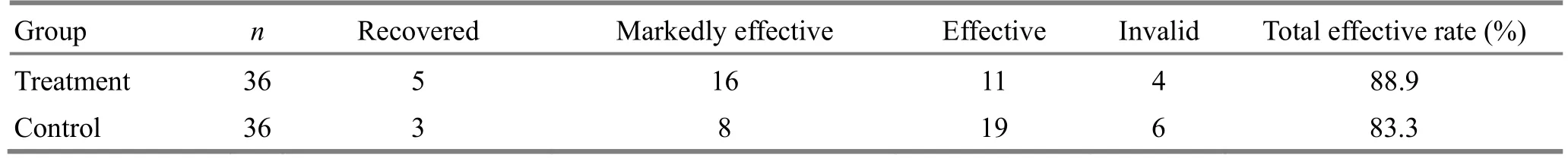
Table 3. Comparison of clinical efficacy (case)

Table 4. Comparison of the integrate score of PSQI in the follow-up study [M (Q1, Q3), point]
4 Discussion
InHuang Di Nei Jing(Yellow Emperor’s Classic of Internal Medicine), insomnia is named ‘Bu De Wo’(inability to sleep), ‘Mu Bu Ming’ (inability to close the eyes), believed to be caused by pathogenic qi invading the Zang-fu organs, or the defensive qi failed to enter yin. The risk factors include improper diet, emotional disorders, fatigue, over-anxiety, chronic disease and aging, which will lead to uneasiness. When the spirit fails to guard the internal and body fails to transit from movement to stillness, insomnia will occur. The treatment of insomnia should be based on syndrome differentiation. However, the syndrome of insomnia is rather complicated, not to mention that it will vary during the treatment, making it difficult to focus on the key point[10]. Body constitution is a comparatively stable comprehensive innate feature of morphological structure, physiological function and mental state on the basis of prenatal endowment and postnatal acquisition. Body constitution runs through the whole process of disease, thus becoming an essential factor restricting and influencing the onset and development of the disease[11]. Therefore, better treatment result can be achieved with less effort paid when body constitution is well regulated.
Insomnia due to blood stasis is not rare in clinic. With extremely varied disease duration but comparatively long average duration, this type of insomnia belongs to intractable insomnia[12-13]. The onset time of blood stasis-related diseases in blood stasis constitution depends on genetic factor[14]. External traumas and internal injuries all can disturb with the production and circulation of blood, gradually forming up a blood stasis constitution. Blood stasis is usually accompanied by qi deficiency, qi stagnation and phlegm stagnation, which can block the heart vessels or impair the nutrition supply to heart and spirit, subsequently preventing yang from entering yin, and then insomnia develops when spirit fails to guard its position. InYi Lin Gai Cuo(Correction of Errors in Medical Classics), Wang Qing-ren explained deeply the insomnia of blood stasis type, and suggested to treat it withXue Fu Zhu Yudecoction[15].Acupuncture can produce improving effect for multiple symptoms caused by blood stasis which is featured by blood circulation disturbance and blocking of meridians[16-17]. It’s been proven by numerous clinical trials that acupuncture is safe and effective in treating insomnia[18-19], though the features of different types of insomnia and the acupuncture-moxibustion treatment for intractable insomnia still expect further study.
In this study, Baihui (GV 20) was selected for acupuncture because the Governor Vessel connects with the brain, able to regulate and calm the mind, and clear the head and eyes; the Yuan-Primary point of Heart Meridian Shenmen (HT 7) can calm the heart and tranquilize the mind; as the crossing point of Liver,Spleen and Kidney Meridians, Sanyinjiao (SP 6) can nourish blood and calm the mind; Zhaohai (KI 6)connects with the Yin Heel Vessel and Shenmai (BL 62)connects with the Yang Heel Vessel, together working to regulate and harmonize yin and yang; as an empirical point for insomnia, Anmian [Extra, locates at the midpoint between Yiming (EX-HN 14) and Fengchi(GB 20)] can tranquilize the mind and benefit sleep. The above points joining together can unblock meridians and collaterals, and regulate and harmonize yin and yang[20]. Bloodletting therapy can dredge the stagnated qi and blood in meridians and collaterals, improving the pathogenic status of blood stasis and also the biased body constitution, and finally ameliorate insomnia by targeting both causes and symptoms[21]. This study conducted a 3-month follow-up and found that the treatment group had a more stable therapeutic efficacy,indicating that this treatment protocol is worth promoting in clinic.
Conflict of Interest
The authors declared that there was no potential conflict of interest in this article.
Statement of Informed Consent
Informed consent was obtained from all individual participants or their relatives in this study.
[1] Sleep Disorder Group, Chinese Society of Neurology.Guideline on diagnosis and treatment of insomnia in Chinese adults. Zhonghua Shenjingke Zazhi, 2012, 45(7):534-540.
[2] Yeung WF, Chung KF, Zhang ZJ, Chan WC, Zhang SP, Ng RM, Chan CL, Ho LM, Yu YM, Lao LX.Electroacupuncture for tapering off long-term benzodiazepine use: study protocol of randomized controlled trial. BMC Complement Altern Med, 2017,17(1): 183.
[3] Bai YP, Zhang WL, Liu EJ, Wang SQ, Liu Q. Factors influencing acupuncture for insomnia. Zhongguo Zhen Jiu,2015, 35(10): 1057-1059.
[4] Wang Q. Traditional Chinese Medical Constitution. Beijing:People’s Medical Publishing House, 2005: 68.
[5] Pan JY, Ma WB, Zhang JH, Liang HJ, Ma P. Differences between objective and subjective sleep quality in chronic primary insomniacs and the correlated factors. Zhongguo Shenjing Jingshen Jibing Zazhi, 2007, 33(2): 69-72.
[6] Zhou ZY. Internal Medicine of Traditional Chinese Medicine. Beijing: China Press of Traditional Chinese Medicine, 2007: 146-150.
[7] Wang Q. Classification and diagnosis basis of nine basic constitutions in Chinese medicine. Beijing Zhongyiyao Daxue Xuebao, 2005, 28(4): 1-8.
[8] Wang XD, Wang XL, Ma H. Rating Scales for Mental Health (Expanded Edition). Beijing: Department of Chinese Mental Health Journal, 1999: 31-35.
[9] Chen XH, Li Y, Kui Y, Wang C, Fang F, Zhou DJ, Li Y,Zhang SH, Xian YD. Sleep disorder treated mainly with flying needling therapy, a clinical randomized controlled research. Zhongguo Zhen Jiu, 2013, 33(2): 97-100.
[10] Chen LJ, Xu BY, Ka J, Liu QY, Zhang BL, Pan YM.Blinding randomization and control design in study of syndrome differentiation-based treatment for primary insomnia. Zhongxiyi Jiehe Xinnaoxueguanbing Zazhi,2016, 14(1): 82-84.
[11] Wang L, Li L. Analysis of the Body Constitution of 2 361 Insomnia Patients. Xi’an: Theses Collection of the Fourth Re-election Conference of Psychosomatic Medicine Committee, China Society of Integrated Traditional Chinese and Western Medicine; the Seventh National Forum on Psychosomatic Medicine of Integrated Traditional Chinese and Western Medicine, 2013: 114-119.
[12] Chen C, Song YM. Research on rules of famous traditional Chinese medicine doctors in differentiation and treatment of blood-stasis type insomnia. Liaoning Zhongyi Zazhi,2017, 44(4): 723-725.
[13] Pan SB, Dong MJ, Tian JZ. Relationship of insomnia and stasis of blood. Hubei Zhongyi Xueyuan Xuebao, 2005,7(4): 43-44.
[14] Ma XJ, Yin HJ, Chen KJ. Investigation of gene expression profiles in patients with blood stasis syndrome. Zhong Xi Yi Jie He Xue Bao, 2008, 6(4): 355-360.
[15] Wang QR.Yi Lin Gai Cuo(Correction of Errors in Medical Classics). Beijing: People’s Medical Publishing House,2005: 8.
[16] Sun ZL, Xi YJ, Pu YX, Xi DP, Chen HP, Xi GF. Study on relationship of blood stasis syndrome in traditional Chinese medicine and rheumatoid arthritis. Zhen Ci Yan Jiu, 1995,20(2): 71-75.
[17] Zhao HJ, Wang Y, Lu Y, Han BB, Wang SJ. Experimental study on acupuncture improving blood stasis syndromes in cerebral ischemia with characteristics of poor blood and clogging the meridians. Liaoning Zhongyi Zazhi, 2013,40(12): 2587-2590.
[18] Dong B, Chen Z, Yin X, Li D, Ma J, Yin P, Cao Y, Lao L,Xu S. The efficacy of acupuncture for treating depressionrelated insomnia compared with a control group: a systematic review and meta-analysis. Biomed Res Int, 2017,2017: 9614810.
[19] Huang W, Kutner N, Bliwise DL. A systematic review of the effects of acupuncture in treating insomnia. Sleep Med Rev, 2009, 13(1): 73-104.
[20] Wang H. Science of Acupuncture and Moxibustion. Beijing:China Press of Traditional Chinese Medicine, 2012: 248.
[21] Wang Y. Talk about syndromes of blood stasis and promoting blood circulation to remove blood stasis.Changchun Zhongyiyao Daxue Xuebao, 2007, 23(5): 5-6.
 Journal of Acupuncture and Tuina Science2018年1期
Journal of Acupuncture and Tuina Science2018年1期
- Journal of Acupuncture and Tuina Science的其它文章
- Points selection pattern in acupuncture-moxibustion treatment of gouty arthritis: an analysis based on bibliometrics
- Analysis of points selection pattern in acupuncture treatment of sleep apnea syndrome based on data mining
- Clinical observation of Shu-acupuncture method in Nei Jing (Classic of Internal Medicine) for shoulder and arm pain
- Efficacy observation on acupuncture plus moving cupping with compound white mustard oil for lumbar myofascitis
- Music electric stimulation of points for anxiety:a multi-center randomized controlled clinical trial
- Development of workplace-related Liver Meridian-depression scale
