高强度聚焦超声对子宫肌瘤患者免疫功能的影响
弓 瑜 王 璐
高强度聚焦超声对子宫肌瘤患者免疫功能的影响
弓 瑜 王 璐
目的比较高强度聚焦超声(HIFU)和子宫肌瘤切除术(Myomectomy)对子宫肌瘤患者的免疫功能的影响。方法将子宫肌瘤患者80例,随机分为HIFU组或Myo组。于入院时和术后24 h采集静脉血样,流式细胞术检测患者CD4+、CD8+、CD4+/CD8+、NK细胞水平,酶联免疫吸附法(ELISA)检测患者血清IL-2,IL-6 和IL-10水平。结果HIFU组患者恢复快,术后并发症较少,住院时间较短(P<0.05)。行HIFU术后患者CD4+T细胞、CD8+T细胞、CD4+/CD8+、NK细胞水平无显著变化(P>0.05);与之相反,手术切除后24 h,患者CD4+T细胞、CD8+T细胞、NK细胞水平均显著下降(P<0.05),CD4+/CD8+比例也显著下降(P<0.05)。治疗后,两组患者血清IL-6和IL-10水平均显著升高,IL-2水平显著降低;HIFU组患者IL-6和IL-10水平显著低于Myo组,Myo组患者IL-2水平明显高于HIFU组。结论HIFU对患者免疫功能影响较小,更好的免疫功能可能与组织创伤应激减少有关,并有助于减少术后并发症的发生。
高强度聚焦超声;子宫肌瘤;免疫功能
手术创伤应激可导致组织器官产生神经、内分泌、代谢及免疫功能的变化等一系列应激反应[1-2],从而影响患者的预后和转归[3],处理不当会发生严重后果。手术技术的改进导致微创手术替代传统开放性手术。高强度聚焦超声(HIFU)是1种新型微创技术,已广泛用于治疗子宫肌瘤[4]。HIFU可诱导目标肌瘤完全凝固坏死,避免手术暴露[5],有效地减轻了子宫肌瘤患者月经过多,月经延长,后背疼痛,盆腔不适和尿频等症状。与传统开放手术相比,行HIFU手术的患者恢复快,复发率低,预后更好[6]。本研究通过临床试验,比较HIFU和手术切除对子宫肌瘤患者免疫功能及炎症因子的影响。
1 资料与方法
1.1 病例资料
前瞻性纳入2012年2月至2016年12月我院收治的子宫肌瘤患者80例,按奇偶数法随机分为两组。Myo组(n=40)行子宫肌瘤切除术;HIFU组(n=40)行高强度聚焦超声。本研究由我院伦理委员会批准实施,所有入组的患者均签署了知情同意书。
1.2 入选标准
纳入标准:①经临床检查和超声检查确诊为子宫肌瘤;②符合手术指征(异常子宫出血,盆腔区压迫症状,反复妊娠丢失)[7]。排除标准:①合并阴道炎,盆腔炎,卵巢肿瘤和子宫内膜异位症等其它妇科疾病者;②结缔组织病或曾用大剂量放射治疗者;③麻醉禁忌征者。
1.3 治疗方法
高强度聚焦超声(HIFU):在超声引导下,给予超声消融治疗(聚焦超声肿瘤治疗系统,重庆海扶医疗科技股份有限公司,国械注准:20153230178)。患者取俯卧位,静注瑞芬太尼50~400 μg和咪达唑仑1~4 mg镇静镇痛,治疗期间患者均保持清醒状态。灰度变化为HIFU超声消融导致靶肿瘤组织坏死,当整个靶肌瘤灰度增加时停止治疗。治疗功率为300~400 w。手术切除(Myo):患者经气管插管和全身麻醉(初始:芬太尼0.02 mg,异丙酚100 mg,维库溴铵:6 mg,咪达唑仑2 mg;维持:异丙酚6~10 mg/kg/h),经腹横切口切除子宫肌瘤。
1.4 观察指标
所有患者于治疗前后采外周血5 ml。免疫功能:流式细胞术检测治疗前后CD4+、CD8+、CD4+/CD8+、NK细胞水平。炎症因子:酶联免疫吸附法(ELISA)检测治疗前后IL-2,IL-6 和IL-10水平。不良反应:术后患者不良反应发生情况。
1.5 统计学方法
2 结果
2.1 患者一般资料及手术指标比较
80例患者手术均顺利完成。HIFU组与Myo组患者年龄、体质指数、子宫体积、肿瘤体积的差异均无统计学意义(P>0.05),两组数据具有临床可比性。HIFU组与Myo组在手术时间上无统计学差异,Myo组的平均术中出血量为100 ml,HIFU组术中出血量为0 ml。HIFU组的术后住院时间,日常活动恢复正常时间均显著短于Myo组(P<0.05)。见表1。

表1 患者一般资料和手术指标比较
2.2 HIFU和手术切除对患者免疫功能的影响
行HIFU术后患者CD4+T细胞、CD8+T细胞、CD4+/CD8+、NK细胞水平无显著变化(P>0.05);与之相反,手术切除后24 h,患者CD4+T细胞、CD8+T细胞、NK细胞水平均显著下降(P<0.05),CD4+/CD8+比例也显著下降(P<0.05),且显著低于HIFU组(P<0.05)。见表2。

表2 两种方式对患者免疫功能的影响
注:与治疗前比较,*为P<0.05;与治疗后HIFU组比较,#为P<0.05。
2.3 HIFU和手术切除对患者炎症因子的影响
治疗后两组患者血清IL-6和IL-10水平均显著升高,HIFU组IL-6和IL-10水平显著低于Myo组(P<0.05);血清IL-2水平显著降低,Myo组明显高于HIFU组(P<0.05)。见表3。

表3 两种手术方式对炎症因子的影响
注:与治疗前比较,*为P<0.05;与治疗后HIFU组比较,#为P<0.05。
2.4 HIFU和手术切除不良反应比较
HIFU组患者不良反应发生率显著低于Myo组(χ2=4.501,P=0.034)。两组疼痛、便秘腹泻发生率相比,差异无统计学意义(P>0.05),阴道出血、呕吐/腹胀等不良反应发生率HIFU组明显更低(P<0.05)。见表4。
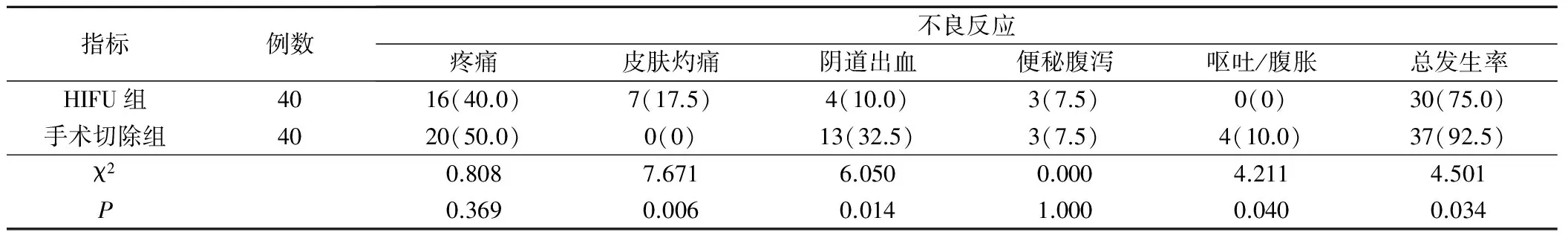
表4 不良反应发生情况比较(例,%)
3 讨论
与开放的子宫肌瘤切除术比较,高强度聚焦超声(HIFU)有恢复快,术后并发症少,住院时间短等优点,我们的研究也证实了这一点,这些结果可能与微创技术减少了创伤和对腹腔的影响有关[8]。此外,HIFU消融的肿瘤裂解物可激活人体的免疫系统,诱发特异性免疫反应[9]。本研究中,与行常规切除术患者术后免疫功能相比,行HIFU患者特异和非特异免疫功能更好,具体表现为行HIFU术后患者免疫细胞百分比无显著变化(P>0.05),而手术切除后患者免疫细胞百分比显著下降。这阐明了行HIFU患者术后并发症较少的可能原因,也表明了HIFU治疗潜在的抗肿瘤优势;因为HIFU热消融导致的全身免疫反应对转移性肿瘤的生长控制非常重要[10]。
Th1和Th2细胞是CD4+T淋巴细胞亚群,在体液免疫和细胞免疫调节中发挥重要作用。Th1细胞主要分泌干扰素-γ(IFN-γ)和IL-2,Th2细胞主要分泌IL-4,IL-6和IL-10。在生理条件下,机体会维持Th1/Th2亚群功能平衡。手术应激诱使Th2型免疫应答增加,导致体液免疫应答增强,细胞免疫应答减弱[11]。这与本研究结论一致:HIFU/手术切除后,两组患者血清IL-6和IL-10均显著升高;IL-2水平显著降低。有文献表明,IL-6的浓度与术后组织创伤程度成正比[12],IL-6水平在术后早期不断增加,诱导急性期反应并上调IL-10[8]。这表明了无论哪一种手术方式,均会导致患者术后IL-6,IL-10同时增加。
综上所述,我们证实了HIFU消融术后,患者特异和非特异性免疫功能更好,有利于降低患者围手术期并发症发生率。因此,在符合HIFU指征的条件下,HIFU应成为治疗子宫肌瘤的首选方式。
[1] Sylla P,Kirman I,Whelan RL.Immunological advantages of advanced laparoscopy〔J〕.Surg Clin North Am,2005,85(1):1-18.
[2] Buunen M,Gholghesaei M,Veldkamp R,et al.Stress response to laparoscopic surgery:a review〔J〕.Surg Endosc,2004,18(7):1022-1028.
[3] Allendorf JD,Bessler M,Horvath KD,et al.Increased tumor establishment and growth after open vs laparoscopic surgery in mice may be related to differences in postoperative T-cell function〔J〕.Surg Endosc,1999,13(3):233-235.
[4] Funaki K,Fukunishi H,Sawada K.Clinical outcomes of m-agnetic resonance-guided focused ultrasound surgery for uterine myomas:24-month follow-up〔J〕.Ultrasound Obstet Gynecol,2009,34(5):584-589.
[5] Chen WS,Liu HL,Tung YS,et al.Reducing lesion aberration by dual-frequency focused ultrasound ablations〔J〕.Int J Hyperthermia,2011,27(7):637-647.
[6] Taran FA,Tempany CM,Regan L,et al.Magnetic resonan-ce-guided focused ultrasound (MRgFUS) compared with abdominal hysterectomy for treatment of uterine leiomyomas〔J〕.Ultrasound Obstet Gynecol,2009,34(5):572-578.
[7] Bulun SE.Uterine fibroids〔J〕.N Engl J Med,2013,369(14):1344-1355.
[8] Maruszynski M,Pojda Z.Interleukin 6 (IL-6) levels in the monitoring of surgical trauma〔J〕.Surg Endosc,1995,9(8):882-885.
[9] Mace TA,Zhong L,Kokolus KM,et al.Effector CD8+T c-ell IFN-γ production and cytotoxicity are enhanced by mild hyperthermia〔J〕.Int J Hyperthermia,2012,28(1):9-18.
[10] Wu F,Zhou L,Chen WR.Host antitumour immune responses to HIFU ablation〔J〕.Int J Hyperthermia,2007,23(2):165-171.
[11] Decker D,Schondorf M,Bidlingmaier F,et al.Surgical stre-ss induces a shift in the type-1/type-2 T-helper cell balance,suggesting down-regulation of cell-mediated and up-regulation of antibody-mediated immunity commensurate to the trauma〔J〕.Surgery,1996,119(3):316-325.
[12] Frick VO,Justinger C,Rubie C,et al.Thoracotomy procedures effect cytokine levels after thoracoabdominal esophagectomy〔J〕.Oncology Reports,2012,27(1):258-264
InhibitoryEffectoftheSteroidSaponinsfromtheFlowersofCestrumNocturnum,Linn(SSFCN)onProliferationofLeukemiaK562CellsandPI3K/AKtPathwayRegulation
GONGYu,WANGLu.
WomenandInfantsHospitalofZhengzhou,Zhengzhou,450000
ObjectiveTo compare the effect of high-intensity focused ultrasound(HIFU) and conventional myomectomy on immune function in patients with uterine fibroids.Methods80 patients with uterine fibroids were divided into the HIFU or Myo group randomly.Venous blood samples were collected 24 h before and after operation.The percentages of CD4+and CD8+T cells and natural killer (NK) cells were quantified by flow cytometry (FCM).Serum levels of interleukin-2 (IL-2),IL-6 and IL-10 were determined by enzyme-linked immunosorbent assay.ResultsHIFU was associated with earlier recovery,fewer post-operative complications,and shorter hospital stay (P<0.05).The levels of CD4+and CD8+T cells and NK cells in the HIFU group were not significantly altered after treatment compared with before treatment.In contrast,the levels of these cells in the Myo group decreased significantly after conventional myomectomy (P<0.05).The CD4+/CD8+T cell ratios also decreased significantly (P<0.05).Serum levels of IL-6 and IL-10 increased after treatment in both groups.IL-6 and IL-10 levels were significantly lower in the HIFU group than in the Myo group (P<0.05).In contrast,IL-2 level decreased significantly in the Myo group compared to the HIFU group(P<0.05).ConclusionHIFU treatment has little influence on immune functions.Better preserved immune function may reflect a reduction in tissue trauma after HIFU treatment and has less complications.
High-intensity focused ultrasound(HIFU);Uterine fibroids;Immune function
(ThePracticalJournalofCancer,2017,32:2067~2069)
450000 河南省郑州市妇幼保健院(弓 瑜);450000 郑州大学第一附属医院(王 璐)
10.3969/j.issn.1001-5930.2017.12.047
R737.33
A
1001-5930(2017)12-2067-03
2017-06-09
2017-08-29)
(编辑:吴小红)