Vulvar inflammation as a manifestation of Crohn's disease
Michael E. Abboud, Sarah E. Frasure
Department of Emergency Medicine, Brigham and Women's Hospital, Boston, MA 02115, USA
Case Letter
Vulvar inflammation as a manifestation of Crohn's disease
Michael E. Abboud, Sarah E. Frasure
Department of Emergency Medicine, Brigham and Women's Hospital, Boston, MA 02115, USA
Dear editor,
Crohn's disease is a chronic inflammatory bowel disease that is also associated with extra-intestinal complications, such as arthritis, erythema nodosum,deep venous thrombosis, and uveitis. Involvement of the vulva, however, is a rare finding in female patients with Crohn's disease. We present a case of vulvar Crohn's disease and discuss the disease process and treatment options for affected patients.
CASE
A 47-year-old female with a history of fistulizing Crohn's disease, status-post subtotal colectomy and end ileostomy, on methotrexate, presented to the emergency department (ED) with abdominal pain and a painful rash.The patient noted five days of worsening abdominal pain associated with low-grade fevers, decreased stool output,nausea, decreased appetite, and skin excoriations across her lower abdomen. These symptoms were consistent with her prior Crohn's flares. In addition, however, she had also noted increasingly severe perineal pain and marked swelling of the left vulva, symptoms which she had never had before.
The patient was hemodynamically stable in the ED.Her physical exam was notable for a soft abdomen with normoactive bowel sounds. She was diffusely tender throughout, however, and the ostomy contained liquid green stool. Excoriations were noted across the lower abdomen. The patient's genitourinary exam revealed significant edema and erythema of the left vulva.Moreover, the left vulvar was exquisitely tender to palpation with a small area of fl uctuance. Her bloodwork was notable for a white blood cell count of 16.84 K/uL. The patient subsequently underwent computed tomography(CT) imaging of the abdomen and pelvis. Although there was no evidence of Crohn's colitis or enteritis,the CT scan demonstrated a 2.2 cm left labial fluid collection, concerning for an abscess, with surrounding inflammation (Figures 1, 2).

Figure 1. Coronal view of the patient's abdominal computed tomography scan with a vulvar abscess and surrounding inflammation (arrow).
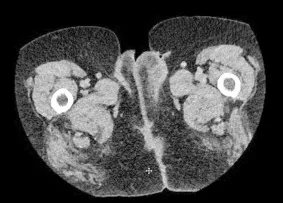
Figure 2. Axial view of the patient's abdominal computed tomography scan with a vulvar abscess and surrounding inflammation (arrow).
The emergency physician consulted both the gastroenterology and gynecology services. The gastroenterology service recommended incision and drainage, intravenous antibiotics, and cessation of immunosuppressant medication. The gynecology service,however, recommended against incision and drainage given the concern for vulvar tissue breakdown, abscess recurrence, and poor skin healing in Crohn's patients.The patient was provided with IV vancomycin and IV ciprofloxacin in the ED and admitted to the medical service in stable condition. Her symptoms improved markedly within 48 hours. During the second day of her admission, the abscess spontaneously drained purulent fluid; a wound culture subsequently grew Proteus mirabilis. She was discharged with a two-week course of oral ciprofloxacin and clindamycin.
DISCUSSION
Crohn's disease is a chronic granulomatous inflammatory disorder that usually affects sections of the gastrointestinal tract. In addition, Crohn's disease is associated with various extra-intestinal manifestations. Genitourinary manifestations, including ovarian Crohn's and rectovaginal fistulas, are well described.[1,2]Genital complications, such as vulvar lesions, however, are very rare.[3]Fewer than 200 cases of vulvar Crohn's disease have been reported in the literature since it was first described by Parks et al[4,5]in 1965. The development of vulvar lesions may occur due to the contiguous spread of Crohn's disease (i.e. direct extension from intestinal involvement), or as a non-contiguous (or metastatic)complication, in which there is no direct connection between the gastrointestinal tract and genitalia.[6]Patients with vulvar Crohn's disease may present with erythema,edema, pain, and pruritis of the vulva.[7]If untreated,patients may develop vulvar abscesses or "knife-cut"ulcers that are highly specific for extra-intestinal Crohn's disease.
Diagnosis of vulvar Crohn's disease is challenging for several reasons. Studies show that 20%–36% of patients with vulvar Crohn's disease will not exhibit any gastrointestinal symptoms, and vulvar Crohn's may be the first manifestation of their underlying autoimmune disease.[3,8,9]In addition, the differential diagnosis of vulvar inflammation and ulceration is extensive. Noninfectious causes of genital ulcers include aphthous ulcers, Lipschutz ulcers, pressure ulcers,Behcet's disease, pyoderma gangrenosum, hidradenitis suppurativa, and malignancy.[10]Infectious causes include cutaneous abscesses (often due to methicillin-resistant Staphylococcus aureus), Bartholin gland abscesses,necrotizing fasciitis, various sexually transmitted diseases, and bacterial superinfection of noninfectious lesions.[11]In most cases, the diagnosis of vulvar Crohn's disease is confirmed on histopathology by the presence of inflammatory infiltrates, epidermal ulceration, and noncaseating granulomas.[5]
Treatment recommendations for vulvar Crohn's disease have not been well established, as the natural course of disease is unpredictable. While some lesions resolve spontaneously, others fail both medical management and surgical debridement.[12]The majority of patients are treated with a prolonged course of antibiotic therapy (classically metronidazole), often in combination with mesalamine or immunosuppressive medications (including topical steroids and monoclonal antibody therapy).[3,8]Unfortunately, several case reports describe rapid recurrence of vulvar lesions when antibiotic therapy is stopped.[13–15]Surgical intervention is less commonly described as the initial treatment modality for vulvar lesions, but may be employed as a second-line treatment for vulvar Crohn's disease that is refractory to medical management. While localized surgical excision has low success rates due to frequent localized recurrence of vulvar lesions and suboptimal wound healing, vulvectomy has been described as a radical, yet more definitive treatment option.[3,16–18]
Our patient was treated with a two-week course of oral antibiotic therapy (clindamycin and ciprofloxacin),as well as continued immunotherapy with methotrexate.At a follow-up visit, the patient's primary care physician noted scarring and deformity of the left vulva; there was no evidence, however, of active inflammation or recurrent infection. Vulvar involvement of Crohn's disease is a serious yet rare complication. It is imperative, therefore,that emergency physicians are aware of this particular disease complication, in order to improve both diagnostic accuracy and patient care.
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors declare that there are no conflicts of interest relevant to the content of the article.
Contributors: Abboud ME proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
1 Andreani SM, Dang HH, Edwards DP, Baig MK, Khan M,Payne JG. Ovarian Crohn's disease: contiguous or metastatic?Inflamm Bowel Dis. 2006;12(11):1091–2.
2 Andreani SM, Dang HH, Grondona P, Khan AZ, Edwards DP.Rectovaginal fistula in Crohn's disease. Dis Colon Rectum.2007;50(12):2215–22.
3 Andreani SM, Ratnasingham K, Dang HH, Gravante G, Giordano P. Crohn's disease of the vulva. Int J Surg. 2010;8(1):2–5.
4 Parks AG, Morson BC, Pegum JS. Crohn's disease with cutaneous involvement. Proc R Soc Med. 1965;58:241–2.
5 Barret M, de Parades V, Battistella M, Sokol H, Lemarchand N, Marteau P. Crohn's disease of the vulva. J Crohns Colitis.2014;8(7):563–70.
6 Bohl TG. Vulvar ulcers and erosions – a dermatologist's viewpoint. Dermatol Ther. 2004;17(1):55–67.
7 Madnani NA, Desai D, Gandhi N, Khan KJ. Isolated Crohn's disease of the vulva. Indian J Dermatol Venereol Leprol.2011;77(3):342–4.
8 Laftah Z, Bailey C, Zaheri S, Setterfield J, Fuller LC, Lewis F.Vulval Crohn's disease: a clinical study of 22 patients. J Crohns Colitis. 2015;9(4):318–25.
9 Zhang AJ, Zhan SH, Chang H, Gao YQ, Li YQ. Crohn disease of the vulva without gastrointestinal manifestations in a 16-yearold girl. J Cutan Med Surg. 2015;19(1):81–3.
10 Kirshen C, Edwards L. Noninfectious genital ulcers. Semin Cutan Med Surg. 2015;34(4):187–91.
11 Wood SC. Clinical manifestations and therapeutic management of vulvar cellulitis and abscess: methicillin-resistant staphlycoccus aureus, necrotizing fasciitis, Bartholin absess,Crohn disease of the vulva, hidradenitis suppurativa. Clin Obstet Gynecol. 2015;58(3):503–11.
12 Shen RN, Cybulska BA, Thin RN, McKee PH. Vulvar Crohn's disease mimicking genital herpes. Int J STD AIDS.1993;4(1):54–6.
13 Holohan M, Coughlan M, O'Loughlin S, Dervan P. Crohn's disease of the vulva. Case report. Br J Obstet Gynaecol.1988;95(9):943–5.
14 Levine EM, Barton JJ, Grier EA. Metastatic Crohn disease of the vulva. Obstet Gynecol. 1982;60(3):395–7.
15 Brandt LJ, Bernstein LH, Boey SJ, Frank MS. Metronidazole therapy for perineal Crohn's disease: a follow-up study.Gastroenterology. 1982;83(2):383–7.
16 Ansell ID, Hogbin B. Crohn's disease of the vulva. J Obstet Gynaecol Br Commonw. 1973;80(4):376–8.
17 Reyman L, Milano A, Demopoulos R, Mayron J, Schuster S. Metastatic vulvar ulceration in Crohn's disease. Am J Gastroenterol. 1986;81(1):46–9.
18 Kao MS, Paulson JD, Askin FB. Crohn's disease of the vulva.Obstet Gynecol. 1975;46(3):329–33.
Sarah E. Frasure, Email: sarahfrasure@yahoo.com
World J Emerg Med 2017;8(4):305–307
10.5847/wjem.j.1920–8642.2017.04.011
October 15, 2016
Accepted after revision March 28, 2017
 World journal of emergency medicine2017年4期
World journal of emergency medicine2017年4期
- World journal of emergency medicine的其它文章
- Evaluation of a point of care ultrasound curriculum for Indonesian physicians taught by first-year medical students
- Instructions for Authors
- Evaluation of modified Alvarado scoring system and RIPASA scoring system as diagnostic tools of acute appendicitis
- Education in cardiopulmonary resuscitation in Russia:A systematic review of the available evidence
- Rehabilitation of vulnerable groups in emergencies and disasters: A systematic review
- Paediatric-appropriate facilities in emergency departments of community hospitals in Ontario:A cross-sectional study
