Anticholinergic syndrome induced by toxic plants
Stergios Soulaidopoulos, Emmanouil Sinakos, Despoina Dimopoulou, Christos Vettas, Evangelos Cholongitas,Alexandros Garyfallos
Fourth Department of Internal Medicine, Hippokration University Hospital, Medical School, Aristotle University of Thessaloniki, Thessaloniki, Greece
Case Letter
Anticholinergic syndrome induced by toxic plants
Stergios Soulaidopoulos, Emmanouil Sinakos, Despoina Dimopoulou, Christos Vettas, Evangelos Cholongitas,Alexandros Garyfallos
Fourth Department of Internal Medicine, Hippokration University Hospital, Medical School, Aristotle University of Thessaloniki, Thessaloniki, Greece
Dear editor,
Plant intoxication constitutes an issue of great interest in the literature, concerning both human and animal poisoning. Different herbs may produce multiple effects from human organ systems, depending on specific ingredients and metabolites that they contain. These effects may vary from gastroenteritis, hepatotoxicity, peripheral neuropathy, psychosis, rhabdomyolysis and blood count abnormalities to cardiotoxicity and multisystemic organ failure.[1,2]The ingestion of particular plants may induce an anticholinergic syndrome which is caused by their alkaloid metabolites (Table 1). This consists of typical clinical manifestations including altered mental status,hallucinations, mydriasis and tachycardia.[3]The class of plants that cause anticholinergic manifestations includes those that belong to the Solanaceae family, with Atropa Belladona and Datura Stramonium being the most common among them.
Atropa Belladona and Datura Stramonium are known for hundreds of years for their hallucinogenic effect.They are easily found all around the world and have beenused in humans for medical and religious purposes.[4–6]Intoxication can occur as a result of accidental ingestion,especially regarding children poisoning.[7,8]However,the majority of the reported cases, concern intoxication following deliberate use of halluciniogenic substances or overdose in medical use.[9–12]The high concentration of these plants in tropane alkaloids, such as atropine,scopolamine, and hyoscine, induces a pronounced anticholinergic toxicity, characterized by both central and peripheral nervous system clinical manifestations.The onset of symptoms is dose-dependent and includes ataxia, disorientation, short-term memory loss, confusion,hallucinations, psychosis, agitated delirium, seizures,coma, respiratory failure and cardiovascular collapse.[13]Furthermore, clinical signs due to peripheral blockage of the parasympathetic postganglionic muscarinic receptors, such as mydriasis with cycloplegia, dry mucous membranes, hyperreflexia, fl ushed skin, urinary retention,diminished bowel sounds, tachycardia, and hypertension or hypotension, may also be present.[3]As these findings can mimic several clinical entities, including severe central nervous system damage, the early diagnosis of plant intoxication may be crucial for the management of these patients.
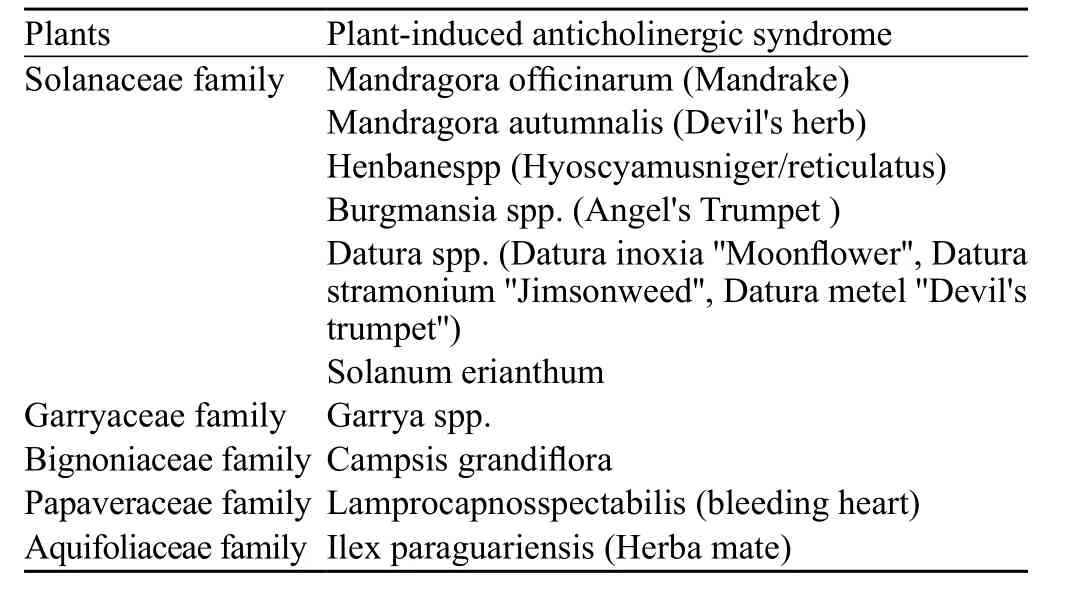
Table 1. Plants inducing anticholinergic syndrome
We report three cases of accidental plant intoxication that presented with anticholinergic manifestations and we then discuss the treatment options for these conditions.
CASES 1 and 2
An 82-year-old woman and her 86-year-old husband presented to the emergency department due to acute onset of discount consciousness, hallucinations, excitation and delirium occurring within the previous hour. Both of them had accidentally consumed the foliage of Datura Stramonium along with other non-cultivated plants which they had collected from a neighboring field. The precise amount of the consumed plant was not possible to be estimated. They were both transferred immediately to the hospital after found fallen to the ground by their familiars in an estimated time of one hour after lunch.On physical examination both patients had normal vital signs except for mild tachycardia (approximately 90 pulses per minute). Glasgow Coma Scale was 9 and 10,respectively. Both patients were disoriented, agitated,making purposeless movements with irrepressible speech and hallucinations. Pupils were widely dilated and not responding to light in both patients, as well.In addition, abdominal examination revealed urinary retention and lessening intestinal peristalsis without abdominal distension, again in both of them. The 82-year-old woman, weighting 67 kg, had a medical history of arterial hypertension and atrial fibrillation while in her 86-year-old hausband, weighting 81 kg, medical history was significant for heart failure due to coronary artery disease, diabetes and benign prostatic hyperplasia.
Both patients were initially managed in the emergency room with gastric lavage, infusing 200 mL of normal saline and aspirating back through a nasogastric tube,repeating it until the returning fluid showed no further gastric contents. Subsequently, 80 g of activated charcoal where administered via the nasogastric tube and a bladder catheterization was performed to avoid urinary retention. After 30 minutes, they were transferred to the Internal Medicine ward where they stayed for a total of four days. Laboratory results had no major abnormalities.A computed tomography (CT) of the brain was performed to exclude acute stroke or other brain damage.Intravenous fl uids (normal saline and dextrose 5% water solution), diazepam 5 mg i.v. twice in the first 24 hours of hospitalization and haloperidol 5 mg i.v. three times a day were administered to control the patients' manifestations.
Symptoms resolved gradually in both patients with no serious sequleae. The wife had an improvement in her status of consciousness, with disappearance of hallucinations tachycardia and agitation on the second day of hospitalization, although, she remained disoriented. During the following days she showed a gradual improvement with total restoration of consciousness. The bladder catheter was removed and she was discharged home in good clinical condition.The husband had a similar clinical course although he remained confused and disoriented for a longer period of time. Quetiapine, 25 mg twice a day, had to be added to his medication to control the symptoms. Finally, all his neurologic manifestations resolved and he was also discharged in good clinical condition.
CASE 3
A 62-year-old man presented to the emergency department due to signs and symptoms of delirium,memory and consciousness disorders. His weight was 86 kg and his medical history was significant for arterial hypertension. His symptoms began twelve hours prior to his admission to our hospital when he complained for nausea, weakness and headache. A clinical diagnosis of stroke had been previously made in a local medical facility. Subsequently, the patient was transferred to our hospital due to constant deterioration of his condition.On clinical examination high blood pressure (180/90),sinus node tachycardia (115 beats/minute) and fever (38 °C)were detected. The remaining physical examination was normal. Of note, cervical stiffness was absent, but bilateral mydriasis was noted. The patient was confused, agitated,and had both memory and self-orientation disorders. He presented with a confused speech having an estimated Glasgow coma scale of 13. No signs of pyramidal damage were found.
A CT scan of the brain was performed to exclude ischemia, intracerebral hemorrhage and brain edema.Due to the fact that disorientation was combined with headache and fever, a lumbar puncture was decided to exclude a central nervous system infection, although there were no clear signs of meningeal irritation. A thorough physical examination, chest X-rays and urine analysis did not reveal any signs of infection. Serum laboratory values were within normal limits, as well. He was treated with intravenous fl uids and paracetamol.
His clinical course was uneventful with quick improvement of his mental and physical status from the second day of hospitalization, although mydriasis persisted for a longer period of time. There was no need for antibiotic treatment due to the non-persistent character of the fever.He was discharged after seven days in apparently good clinical condition. Detailed history taking revealed that the patient had consumed a rather small amount of unknown fruits and herbals, ignoring the possibility of poisoning,during an excursion the day his symptoms began. As samples of these herbals were available, an analysis was performed to identify the exact species. Atropa Belladonna, a plant with known anticholinergic properties,was confirmed to have been ingested and thought to be responsible for the confronting clinical syndrome.
DIS CUSSION
Solanceae family constitutes a large, widespread group of plant species with a remarkable high concentration of alkaloids, which are secondary metabolic products that form a defense mechanism against insects, predator and disease.[14]Alkaloids are pharmacologically active,nitrogen-containing compounds that are divided in several subgroups. An important subgroup of alkaloids,commonly found in plants of the Solonceae family, is tropane alkaloids. They typically have anticholinergic and anesthetic properties.[15]Atropine, hyoscyamine and scopolamine are the most important and extensively studied members of tropane alkaloids. All these substances are found in high concentrations in both Datura Stramonium and AtropaBelladona. Their properties arise from the competitive binding to central nervous system and parasympathetic postganglionic muscarinic receptors which ultimately lead to several clinical manifestations.[16]
Datura Stramonium, also known as "Jimson weed"and "Angel's trumpet", probably represents one of the most commonly encountered plants containing tropane alkaloids. It consists of coarse toothed leaves, trumpet shaped fl owers with white pale violet colored petals and fruits consisting of spiny egg-shaped capsules (Figure 1). Historically, Datura has been used for spiritual purposes, due to its hallucinogenic properties, as well as in traditional medicine to treat asthma and relief pain. All of its parts may become toxic due to their high in tropane alkaloids. It is estimated that the average concentration of atropine and scopolamine is 0.20 and 0.65 mg per blossom, respectively.[11]Several reports in the literature describe different aspects of the anticholinergic syndrome concerning adult, children and animal intoxication.[17–19]Regarding our first two cases, Datura Stramonium was confirmed as the etiology of their clinical syndrome as no other causes were identified and the patients reported eating plants that had similar appearance to Datura Stramonium, a plant that exists in abundance in Greece.

Figure 1. Datura Stramonium.
Atropa belladonna, another widely known member of the Solonseae family, was confirmed after chemical analysis as the cause of the anticholinergic intoxication in our third case. This plant is also known as "deadly nightshade" and has a long history of use as a pharmaceutical cosmetic or deleterious agent (Figure 2). Both the foliage and the berries of the plant are extremely toxic due to their high concentration in tropane alkaloids.[20]The risk of poisoning is important as the berries of the plant are black, globular and sweet and may be easily confused with other edible berries. Remarkably, Atropa Belladonna intoxication may lead to liver function impairment besides its anticholinergic syndrome.[21]However, cases of Atropa Belladonna intoxication are relatively infrequently reported in the literature.
In all of our cases, symptomatic treatment was given to the patients. As soon as the diagnosis of tropane intoxication through plant digestion was suspected,nasogastric lavage was performed according to published recommendations.[22]Gastric lavage and activated charcoal may prove to be useful in the first 24 hours after plant digestion, as they prevent the prolonged alkaloid absorption due to decreased gastric motility. Intubation should be considered before performing gastric lavage,in those cases with great loss of consciousness, unable to protect their airway. In addition, close hemodynamic monitoring was performed and intravenous fluids were administered in order to avoid sudden circulatory collapse in all of our cases. There was no need to provide respiratory support. However, maintenance of airway patency must be secured in the more severe cases of anticholinergic syndrome, as these result in loss of consciousness. Finally, it must be highlighted that bladder catheterization should always be considered as a measure for urinary retention management.

Figure 2. Atropa belladonna.
It has to be mentioned that anticholinergic syndrome,due to its central nervous manifestations, may mimic other central nervous system disorders. These have to be always excluded as the diagnosis of tropane alkaloid toxicity is usually based on medical history. Further investigation may be needed to exclude other clinical entities. Therefore, a brain CT scan was performed in all of our cases to confirm the suspected diagnosis and exclude an alternative diagnosis that could explain the clinical syndrome of our patients. A lumbar puncture also excluded a central nervous system infection in case 3. Fever was finally attributed to a rather clinically nonsignificant, short-term infection, unable to be specified by laboratory and imaging methods.
Sedatives are recommended for the supportive management of tropane alkaloid intoxication,[23]whereas benzodiazepine administration is recommended for those patients whose predominant symptom is mild to moderate agitation.[24]However, it has to be noted that escalating doses of benzodiazepines enhance the risk of intubation.[25]Severe delirium or difficulty in the management of agitation could also be treated with antipsychotic drugs in low doses, such as haloperidol and droperidol. In such cases, patients should be always monitored for QT prolongation.[26,27]In the second case of our series, we added low doses of quetiapine to the patient's treatment (benzodiazepines), which proved to be more effective in the management of his psychiatric manifestations.
Physostigmine is a reversible acetylcholinesterase inhibitor that increases acetylcholine concentration in the synaptic cleft, acting like an antidote to anticholinergic syndrome, capable of reversing both central and peripheral toxicity. Although there are conflicting reports about the role of physostigmine in anticholinergic toxicity, regarding both its efficacy and safety, the general consensus is that it may be considered as a therapeutic option when signs of severe intoxication are present.[28–30]These include tachydysrhythmia causing hemodynamic instability and collapsus, severe agitation or coma, persistent seizures and respiratory depression. The ability of physostigmine to cross the blood-brain barrier can be beneficial and lead to a significant decrease in agitation and other manifestation of central anticholinergic toxicity.[25]On the other hand, contraindications for its use include bronchial asthma, ECG abnormalities, coronary artery disease and mechanical obstruction of the gastrointestinal and urinary tract, while adverse events include seizures, atrioventricular block and asystole.[24]Although physostigmine administration is considered as an alternative therapeutic option, we did not use it in our cases. Taking advanced age and concomitant heart disease into consideration in our first two cases, physostigmine was deferred and was considered only as a salvage treatment. Finally, in the third case there was no need for physostigmine at all due to the low delirium severity and the immediate improvement of the patient's clinical situation.
CONCLUSION
Intoxication by poisonous plants containing tropane alkaloids may constitute a real medical emergency,presenting difficulties in early diagnosis and management.Physicians should be aware of plant intoxication whenever acute onset of consciousness alterations is combined with signs of anticholinergic toxicity and a medical history of vegetal abuse or digestion. Finally, public education about the possibility of serious and fatal poisoning by hallucinogenic or unknown herbs is of great importance.
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors have no financial or other conflicts of interest related to the submitted article to declare.
Contributors: Soulaidopoulos S proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
1 de Boer YS, Sherker AH. Herbal and dietary supplement–induced liver injury. Clin Liver Dis. 2017;21(1):135–49.
2 Teschke R, Wolff A, Frenzel C, Schulze J. Herbal hepatotoxicity- an update on traditional Chinese medicine preparations.Aliment Pharmacol Ther. 2014;40(1):32–50.
3 Chowański S, Adamski Z, Marciniak P, Rosiński G, Büyükgüzel E, Büyükgüzel K, et al. A Review of Bioinsecticidal Activity of Solanaceae Alkaloids. Toxins (Basel). 2016;8(3). pii: E60.
4 Chang SS, Wu ML, Deng JF, Lee CC, Chin TF, Liao SJ.Poisoning by Datura leaves used as edible wild vegetables. Vet Hum Toxicol. 1999;41(4):242–5.
5 He J, Hou XY. The potential contributions of traditional Chinese medicine to emergency medicine. World J Emerg Med.2013;4(2):92–7.
6 Gowdy JM. Stramonium intoxication: review of symptomatology in 212 cases. JAMA. 1972;221(6):585–7.
7 Disel NR, Yilma M, Kekec Z, Karanlik M. Poisoned after dinner: Dolma with datura stramonium. Turk J Emerg Med.2016;15(1):51–5.
8 Rakotomavo F, Andriamasy C, Rasamoelina N, Raveloson N.Datura stramonium intoxication in two children. Pediatr Int.2014;56(3):e14–6. .
9 Guharoy SR, Barajas M. Atropine intoxication from the ingestion and smoking of jimson weed (Datura stramonium). Vet Hum Toxicol. 1991;33(6):588–9.
10 Shervette RE, Schydlower M, Fearnow RG, Lampe RM. Jimson"loco" weed abuse in adolescents. Pediatrics. 1979;63(4):520–3.
11 Diker D, Markovitz D, Rothman M, Sendovski U. Coma as a presenting sign of Datura stramonium seed tea poisoning. Eur J Intern Med. 2007;18(4):336–8.
12 Pereira CA, Nishioka S de D. Poisoning by the use of Datura leaves in a homemade toothpaste. J Toxicol Clin Toxicol. 1994;32(3):329–31.
13 Vearrier D, Greenberg MI. Anticholinergic delirium following Datura stramonium ingestion: Implications for the Internet age. J Emerg Trauma Shock. 2010;3(3):303.
14 Jerzykiewicz J. Alkaloids of Solanaceae (nightshade plants).Postepy Biochem. 2007;53(3):280–6.
15 Pigatto AGS, Blanco CC, Mentz LA, Soares GLG. Tropane alkaloids and calystegines as chemotaxonomic markers in the Solanaceae. An Acad Bras Cienc. 2015;87:2139–49.
16 European Food Safety Authority (EFSA). Tropane alkaloids(from Datura sp.) as undesirable substances in animal feed -Scientific Opinion of the Panel on Contaminants in the Food Chain. EFSA J. 2008;6(8):691.
17 Adegoke S, Alo L. Datura stramonium poisoning in children.Niger J Clin Pract. 2013;16(1):116–8
18 Pekdemir M, Yanturali S, Akay S, Alagoz G. Acute anticholinergic syndrome due to Datura innoxia Miller mixed with lime tea leaves. Vet Hum Toxicol. 2004;46(4):176–7.
19 Cortinovis C, Caloni F. Alkaloid-Containing Plants Poisonous to Cattle and Horses in Europe. Toxins (Basel). 2015;7(12):5301–7.
20 Caksen H, Odabaş D, Akbayram S, Cesur Y, Arslan S, Uner A,et al. Deadly nightshade (Atropa belladonna) intoxication: an analysis of 49 children. Hum Exp Toxicol. 2003;22(12):665–8.
21 Berdai MA, Labib S, Chetouani K, Harandou M. Atropa Belladonna intoxication: A case report. Pan Afr Med J. 2012;11:72. Epub 2012 Apr 17.
22 Kemmerer DA. Anticholinergic syndrome. J Emerg Nurs.2007;33(1):76–8
23 Hanna JP, Schmidley JW, Braselton WE. Datura delirium. Clin Neuropharmacol. 1992;15(2):109–13.
24 Dawson AH, Buckley NA. Pharmacological management of anticholinergic delirium - Theory, evidence and practice. Br J Clin Pharmacol. 2016;81(3):516–24.
25 Burns MJ, Linden CH, Graudins A, Brown RM, Fletcher KE. A comparison of physostigmine and benzodiazepines for the treatment of anticholinergic poisoning. Ann Emerg Med.2000;35(4):374–81.
26 Powney MJ, Adams CE, Jones H. Haloperidol for psychosisinduced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2012;11:CD009377.
27 Isbister GK, Calver LA, Page CB, Stokes B, Bryant JL, Downes MA. Randomized controlled trial of intramuscular droperidol versus midazolam for violence and acute behavioral disturbance:the DORM study. Ann Emerg Med. 2010;56(4):392–401.e1.
28 Schneir AB, Offerman SR, Ly BT, Davis JM, Baldwin RT,Williams SR, et al. Complications of diagnostic physostigmine administration to emergency department patients. Ann Emerg Med. 2003;42(1):14–9.
29 Watkins JW, Schwarz ES, Arroyo-Plasencia AM, Mullins ME.The use of physostigmine by toxicologists in anticholinergic toxicity. J Med Toxicol. 2015;11(2):179–84.
30 Salen P, Shih R, Sierzenski P, Reed J. Effect of physostigmine and gastric lavage in a Datura stramonium-induced anticholinergic poisoning epidemic. Am J Emerg Med. 2003;21(4):316–7.
Stergios Soulaidopoulos, Email: soulaidopoulos@hotmail.com
World J Emerg Med 2017;8(4):297–301
10.5847/wjem.j.1920–8642.2017.04.009
March 25, 2017
Accepted after revision August 20, 2017
 World journal of emergency medicine2017年4期
World journal of emergency medicine2017年4期
- World journal of emergency medicine的其它文章
- Evaluation of a point of care ultrasound curriculum for Indonesian physicians taught by first-year medical students
- Instructions for Authors
- Evaluation of modified Alvarado scoring system and RIPASA scoring system as diagnostic tools of acute appendicitis
- Education in cardiopulmonary resuscitation in Russia:A systematic review of the available evidence
- Rehabilitation of vulnerable groups in emergencies and disasters: A systematic review
- Paediatric-appropriate facilities in emergency departments of community hospitals in Ontario:A cross-sectional study
