c-MET抑制剂联合EGFR-TKI对耐药肺癌细胞增殖、凋亡的影响及其机制
玄香兰,安昌善
(延边大学附属医院,吉林延吉133000)
c-MET抑制剂联合EGFR-TKI对耐药肺癌细胞增殖、凋亡的影响及其机制
玄香兰,安昌善
(延边大学附属医院,吉林延吉133000)
目的观察c-MET抑制剂SU11274联合表皮生长因子-酪氨酸激酶抑制剂(EGFR-TKI)吉非替尼或埃罗替尼对人肺癌细胞株PC9/R(PC9细胞的获得性吉非替尼EGFR-TKI耐药株)增殖、凋亡的影响,并探讨其作用机制。方法培养人肺癌细胞株PC9/R,将PC9/R细胞分为对照组(C组)、SU11274组(S组)、吉非替尼组(G组)、埃罗替尼组(E组)、吉非替尼联合SU11274组(GS组)、埃罗替尼联合SU11274组(ES组)。S组、G组、E组、GS组、ES组分别加入SU11274 5 μmol/L、吉非替尼1 μmol/L、埃罗替尼1 μmol/L、吉非替尼1 μmol/L+SU11274 5 μmol/L、埃罗替尼1 μmol/L+SU11274 5 μmol/L,C组不加药物。于给药72 h后采用MTT法检测细胞增殖活力,流式细胞仪技术检测细胞凋亡情况。采用Western blotting法检测各组细胞中的p-EGFR、p-AKT、p-STAT3蛋白。结果GS组、ES组细胞存活率分别低于G组、E组(P均<0.05),联合组细胞存活率均低于S组(P均<0.05),G组、E组、GS组、ES组细胞存活率均低于C组(P均<0.05)。GS组、ES组早期细胞凋亡比例分别高于G组、E组(P均<0.05),联合组早期细胞凋亡比例均高于S组(P均<0.05),GS、ES、S组早期细胞凋亡比例均高于C组(P均<0.05)。GS组、ES组p-EGFR、p-AKT、p-STAT蛋白相对表达量分别低于G组、E组(P均<0.05),联合组p-EGFR、p-AKT、p-STAT蛋白相对表达量均低于S组(P均<0.05),G组、E组、GS组、ES组蛋白相对表达量均低于C组(P均<0.05)。结论SU11274联合吉非替尼或埃罗替尼可抑制EGFR-TKI耐药的肺癌细胞增殖并促进其凋亡,作用机制可能与抑制EGFR信号通路功能有关。
非小细胞肺癌;肺癌细胞;耐药;表皮生长因子-酪氨酸激酶抑制剂;c-MET抑制剂;细胞增殖;细胞凋亡
肺癌是发病率与病死率非常高的恶性肿瘤,其中非小细胞肺癌(NSCLC)占总数的85%~90%[1]。NSCLC治疗除了传统的手术、化疗、放疗外,还有靶向药物治疗。研究发现,表皮生长因子(EGFR)在NSCLC组织中的阳性率为53.1%~69.7%[2]。30%~40%的NSCLC患者存在EGFR突变[3],多数为腺癌患者,合并EGFR突变者预后往往不良。吉非替尼和埃罗替尼是第一代EGFR-酪氨酸激酶抑制剂(EGFR-TKI),已成为EGFR突变的晚期NSCLC患者的首选治疗方案,然而在治疗后期仍会不可避免地出现耐药。研究[4,5]表明,c-MET通路异常激活是EGFR-TKI继发耐药的重要机制之一,因此c-MET成为了逆转耐药的新靶点。本研究将c-MET抑制剂SU11274与吉非替尼或埃罗替尼联合作用于人肺腺癌细胞株PC9/R(PC9细胞的获得性吉非替尼EGFR-TKI耐药株),观察细胞增殖、凋亡的变化,并探讨其机制。
1 材料与方法
1.1 细胞与主要实验材料 PC9、PC9/R均由上海市肺科医院中心实验室提供。吉非替尼和盐酸埃罗替尼原料购自济南汇丰达化工有限公司。SU11274购自美国Sigma公司。MTT试剂购自美国AMRESCO公司。细胞凋亡检测试剂盒(FITC Annexin V Apoptosis Detection Kit 1)购自美国BD公司。兔抗人c-MET、p-EGFR,p-AKT、p-STAT3、GAPDH购自美国EPITMICS公司。辣根过氧化物酶标记的羊抗兔购自美国JECTION公司。
1.2 细胞分组与给药方法 将PC9/R细胞分为对照组(C组)、SU11274组(S组)、吉非替尼组(G组)、埃罗替尼组(E组)、吉非替尼联合SU11274组(GS组)、埃罗替尼联合SU11274组(ES组)。S组、G组、E组、GS组、ES组分别加入SU11274 5 μmol/L、吉非替尼1 μmol/L、埃罗替尼1 μmol/L、吉非替尼1 μmol/L+SU11274 5 μmol/L、埃罗替尼1 μmol/L+SU11274 5 μmol/L,C组不加入药物。
1.3 细胞增殖观察 取对数生长期的细胞用胰酶消化,将100 μL(含5×103个细胞)悬液接种于96孔板。待细胞贴壁后,各组加入相应药物。72 h后,每孔内加入20 μL的MTT(5 mg/mL),放入细胞培养箱中孵育。4 h后,1 200 r/min离心10 min,弃上清液。每孔加入200 μL的DMSO,摇床上混匀30 min至结晶完全溶解。用酶标仪测量波长530 nm时的OD值。细胞存活率=(实验组OD值-空白组OD值)/(对照组OD值-空白组OD值)×100%。实验重复3次。
1.4 凋亡细胞检测 取1×105个对数生长期细胞接种于6孔板,培养24 h。贴壁后弃原培养液,各组加入相应药物。72 h后,胰酶消化并收集全部细胞到5 mL试管,1 500 r/min离心5 min,去上清液,生理盐水洗涤1次。加入1×Binding Buffer调整细胞浓度为1×106/mL,取100 μL(1×105个细胞)到新的5 mL试管。各管内加入5 μL的FITC和5 μL的PI,室温、避光15 min。上机前加入400 μL的1×Binding Buffer,1 h内上流式细胞仪观察细胞凋亡情况。实验重复3次。
1.5 细胞p-EGFR、p-AKT、p-STAT3蛋白检测 取对数生长的细胞,各组分别加药处理48 h,后立即冰上裂解细胞,4 ℃下12 000 r/min离心30 min,收集各组蛋白裂解液。用BCA蛋白定量法对蛋白定量。取30~40 μg蛋白经8%~10% SDS-PAGE电泳分离后,转印至NC膜上,用5%脱脂奶粉封闭1 h,一抗孵育4 ℃过夜,TBST洗膜10 min×3次,二抗室温摇床孵育1 h,TBST洗膜5 min×5次,ECL化学发光试剂显色、曝光成像。以目的蛋白与内参蛋白灰度值的百分比表示蛋白相对表达量。

2 结果
2.1 各组细胞存活率比较 C组、S组、G组、E组、GS组、ES组细胞存活率分别为100%、99.5%±2.0%、82.5%±4.2%、60.2%±3.2%、68.0%±5.3%、45.6%±3.3%,GS组、ES组细胞存活率分别低于G组、E组(P均<0.05),联合组细胞存活率均低于S组(P均<0.05),G组、E组、GS组、ES组细胞存活率均低于C组(P均<0.05),但S组与C组无统计学差异(P>0.05)。
2.2 各组细胞凋亡率比较 C组、S组、G组、E组、GS组、ES组早期凋亡细胞比例分别为2.7%±0.3%、10.2%±1.2%、5.1%±0.2%、3.3%±0.7%、39.3%±3.5%、23.4%±2.9%,晚期凋亡细胞比例分别为3.6%±1.0%、7.6±1.4%、4.5%±0.9%、8.4%±2.3%、6.5%±1.8%、12.0%±4.7%。GS组、ES组早期细胞凋亡比例分别高于G组、E组(P均<0.05),联合组早期细胞凋亡比例均高于S组(P均<0.05),GS组、ES组、S组早期细胞凋亡比例高于C组(P均<0.05),但G组、E组与C组无统计学差异(P均>0.05)。
2.3 各组细胞p-EGFR、p-AKT、p-STAT蛋白表达比较 GS组、ES组p-EGFR、p-AKT、p-STAT蛋白相对表达量分别低于G组、E组(P均<0.05),联合组p-EGFR、p-AKT、p-STAT蛋白相对表达量均低于S组(P均<0.05),G组、E组、GS组、ES组蛋白相对表达量均低于C组(P均<0.05),但S组与C组无统计学差异(P>0.05)。详见图1、表1。
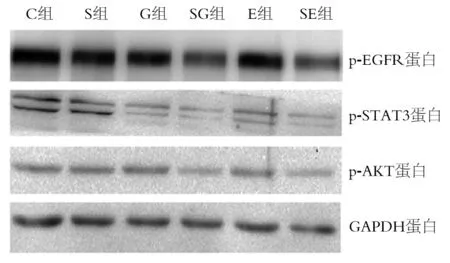
图1 各组细胞中p-EGFR、p-AKT、p-STAT蛋白表达情况
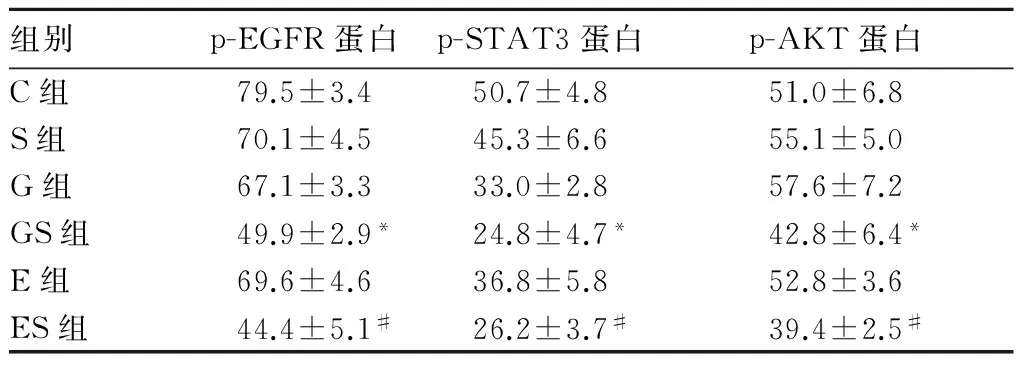
组别p-EGFR蛋白p-STAT3蛋白p-AKT蛋白C组79.5±3.450.7±4.851.0±6.8S组70.1±4.545.3±6.655.1±5.0G组67.1±3.333.0±2.857.6±7.2GS组49.9±2.9*24.8±4.7*42.8±6.4*E组69.6±4.636.8±5.852.8±3.6ES组44.4±5.1#26.2±3.7#39.4±2.5#
注:与G组相比,*P<0.05;与E组相比,#P<0.05。
3 讨论
EGFR是细胞表面跨膜蛋白,以同源或异源二聚体形式活化,通过激活细胞内PI3K-AKT、MEK/ERK、STAT3等信号通路,促进细胞增殖、分化、发育[6]。c-MET是由MET编码的一类具有自主磷酸化活性的跨膜受体,可激活细胞内多种信号通路,如PI3K-AKT、Ras-MAPK、STAT3通路等[7,8],从而促进肿瘤细胞间的相互作用、基质黏附、细胞迁移、侵袭和血管生成。约25%的NSCLC患者存在c-MET蛋白过表达,2%~4%的肺腺癌和肺鳞癌患者存在c-MET扩增[9,10],而c-MET扩增或过表达均与NSCLC的不良预后相关[11]。
吉非替尼和埃罗替尼用于治疗EGFR突变的NSCLC患者,已取得良好的疗效,但最终可因耐药导致肿瘤复发或进展。研究发现,在EGFR突变的EGFR-TKI获得性耐药的NSCLC患者中,约20%的患者存在MET扩增[12],且往往伴随着c-MET蛋白高表达[13]。SU11274可选择性抑制c-MET活化,对其他酪氨酸激酶无作用。据研究[15]报道,在c-MET扩增的耐药肺癌细胞中,c-MET抑制剂可明显提高EGFR-TKI耐药肺癌细胞的敏感性,但单用c-MET抑制剂无明显作用。
本研究所用的人肺腺癌细胞株PC9/R具有EGFR 19外显子E746~A750的缺失突变,是由PC9细胞株进行诱变和筛选获得的耐药性细胞株[14]。本研究将c-MET抑制剂与吉非替尼或埃罗替尼联合作用于PC9/R细胞,结果显示,GS组、ES组细胞存活率分别低于G组、E组,联合组细胞存活率均低于S组,G组、E组、GS组、ES组细胞存活率均低于C组,而S组与C组无差异。GS组、ES组早期细胞凋亡比例分别高于G组、E组,联合早期细胞凋亡比例均高于S组,GS组、ES组、S组早期细胞凋亡比例高于C组,而G组、E组与C组无统计学差异。这说明单用SU11274对PC9/R细胞株的增殖抑制和促凋亡作用并不明显,但与吉非替尼或埃罗替尼联用可显著抑制细胞增殖、促进细胞凋亡,提示SU11274可增强EGFR-TKI对获得性耐药肺癌细胞的敏感性。
肿瘤的发生及发展通过多种信号的作用,下游信号分子可以重叠,所以抑制单一信号通路在实体肿瘤可能不会产生明显的抑瘤作用[16]。EGFR突变及EGFR活化,激活细胞内PI3K/AKT、STAT3、MEK/ERK等EGFR下游信号通路,促进肿瘤细胞增殖、侵袭、血管生成。本研究结果显示,单用吉非替尼、埃罗替尼或SU11274对EGFR、AKT、STAT3的磷酸化无明显影响,吉非替尼或埃罗替尼联合SU11274能够显著抑制EGFR及下游信号分子AKT及STAT3的磷酸化,提示吉非替尼或埃罗替尼联合SU11274对PC9/R的细胞增殖抑制作用可能与抑制EGFR信号通路功能有关。
总之,SU11274联合吉非替尼或埃罗替尼对PC9/R细胞具有显著抑制增殖和促凋亡作用,可阻断EGFR通路下游分子AKT、STAT3的活化。上述研究结果为c-MET抑制剂联合EGFR-TKI方案的应用研究奠定了基础。有研究[17,18]表明,c-MET抑制剂对于原发MET扩增的患者效果明显,与EGFR-TKI联合用药的效果并不优于c-MET抑制剂单药方案[19~21]。对于EGFR-TKI耐药后MET扩增,患者的EGFR通路功能仍然活跃,需要采取与EGFR-TKI联合用药。目前c-MET抑制剂及MET单克隆抗体如Capmatinib(ICN280)联合吉非替尼[22]、Emibetuzumab(LY2875358)联合埃罗替尼[23]的临床试验正在进行中。
[1] DeSantis CE, Lin CC, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2014[J]. CA Cancer J Clin, 2014,64(4):252-271.
[2] 王洋,梁岳培.抗VEGF和抗EGFR靶向治疗非小细胞肺癌的研究进展[J].临床医学工程,2011,18(2):312-314.
[3] 罗承逊,陈易华.非小细胞肺癌的靶点及靶向治疗药物的应用[J].西南军医,2017,19(1):63-65.
[4] Engelman JA, Zejnullahu K, Mitsudomi T, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling[J]. Science, 2007,316(5827): 1039-1043.
[5] Soh J, Okumura N, Lockwood WW, et al. Oncogene mutations, copy number gains and mutant allele specific imbalance (MASI) frequently occur together in tumor cells[J]. PLoS One, 2009,4(10):7464.
[6] Turke AB, Zejnullahu K, Wu YL, et al.Preexistence and clonal selection of MET amplication in EGFR mutant NSCLC[J]. Cancer Cell, 2010,17(1):77-88.
[7] Goyal L, Muzumdar MD, Zhu AX. Targeting the HGF/c-MET pathway in hepatocellular carcinoma[J].Clin Cancer Res, 2013,19(9): 2310-2318.
[8] Trovato M, Torre ML, Ragonese M, et al. HGF/c-met system targeting PI3K/AKT and STAT3/phosphorylated-STAT3 pathways in pituitary adenomas: an immunohistochemical characterization in view of targeted therapies[J]. Endocrine, 2013,44(3): 735-743.
[9] Cancer Genome Atlas Research Network. Comprehensive genomic characterization of squamous cell lung cancers[J]. Nature, 2012,489(7417):519-525.
[10] Cancer Genome Atlas Research Network. Comprehensive molecular profiling of lung adenocarcinoma[J]. Nature, 2014,511(7511):543-550.
[11] Christensen JG, Burrows J, Salgia R. c-Met as a target for human cancer and characterization of inhibitors for therapeutic intervention[J]. Cancer Lett, 2005,225(1):1-26.
[12] Bean J, Brennan C, Shih JY, et al. MET amplification occurs with or without T790M mutations in EGFR mutant lung tumors with acquired resistance to gefitinib or erlotinib[J]. Proc Natl Acad Sci U S A, 2007,104(52): 20932-20937.
[13] Park S, Koh J, Kim DW, et al. MET amplification, protein expression, and mutations in pulmonary adenocarcinoma[J]. Lung Cancer, 2015,90(3): 381-387.
[14] 鞠立霞,周彩存,唐亮,等.吉非替尼获得性耐药的非小细胞肺癌细胞株PC9/AB2相关耐药机制研究[J].中华结核和呼吸杂志,2010,33(5):354-358.
[15] Suda K, Tomizawa K, Osada H, et al. Conversion from the “oncogene addiction” to “drug addiction” by intensive inhibition of the EGFR and MET in lung cancer with activating EGFR mutation[J]. Lung Cancer, 2012,76(3): 292-299.
[16] Liu X, Yao W, Newton RC, et al. Targeting the c-MET signaling pathway for cancer therapy[J]. Expert Opin Investig Drugs, 2008,17(7): 997-1011.
[17] Noonan SA, Berry L, Lu X, et al. Identifying the appropriate FISH criteria for defining MET copy number-driven lung adenocarcinoma through oncogene overlap analysis[J]. J Thorac Oncol, 2016,11(8): 1293-1304.
[18] Rabeau A, Rouquette I, Vantelon JM, et al. Interest of crizotinib in a lung cancer patient with de novo amplification of MET[J]. Rev Mal Respir, 2017,34(1):57-60.
[19] Neal JW, Dahlberg SE, Wakelee HA, et al. Erlotinib, cabozantinib, or erlotinib plus cabozantinib as second-line or third-line treatment of patients with EGFR wild-type advanced non-small-cell lung cancer (ECOG-ACRIN 1512): a randomised, controlled, open-label, multicentre, phase 2 trial[J]. Lancet Oncol, 2016,17(12):1661-1671.
[20] Scagliotti G, von Pawel J, Novello S, et al. Phase III multinational,randomized, double-blind, placebo-controlled study of tivantinib (ARQ197) plus erlotinib versus erlotinib alone in previously treated patients with locally advanced or metastatic nonsquamous non-small-cell lung cancer[J]. J Clin Oncol, 2015,33(24):2667-2674.
[21] Yoshioka H, Azuma K, Yamamoto N, et al. A randomized, double-blind, placebo-controlled, phase III trial of erlotinib with or without a c-Met inhibitor tivantinib (ARQ 197) in Asian patients with previously treated stage IIIb/IV nonsquamous nonsmall-cell lung cancer harboring wild-type epidermal growth factor receptor (ATTENTION study)[J]. Ann Oncol, 2015,26(10):2066-2072.
[22] Rybkin II, Smit E, Kopp HG, et al. PS01.60: Ph Ib/II, Trial of INC280 ± Erlotinib vs Platinum + Pemetrexed in Adult pts with EGFR-Mutated, cMET amplified, EGFR TKI Resistant, Advanced NSCLC: Topic: Medical Oncology[J]. J Thorac Oncol, 2016,11(11):S307-S308.
[23] Rosen LS, Goldman JW, Algazi AP, et al. A First-in-Human Phase I Study of a Bivalent MET Antibody, Emibetuzumab (LY2875358), as Monotherapy and in Combination with Erlotinib in Advanced Cancer[J]. Clin Cancer Res, 2017,23(8):1910-1919.
Effectsofc-METinhibitorcombinedwithEGFR-TKIonproliferationandapoptosisofdrug-resistantlungcancercells
XUANXianglan,ANChangshan
(TheAffiliatedHospitalofYanbianUniversity,Yanji133000,China)
ObjectiveTo observe the effects of c-MET inhibitor SU11274 combined with the epidermal growth factor receptor-tyrosine kinase inhibitor (EGFR-TKI) gefitinib or erlotinib on the proliferation and apoptosis of human lung cancer cell line PC9/R (acquired gefitinib EGFR-TKI-resistance cell line PC9 cells) and to investigate the mechanism.MethodsWe cultured the human lung cancer cell line PC9/R and divided them into six groups: the control group (group C) , SU11274 group (group S), gefitinib group (group G), erlotinib group (group E), gefitinib combined with SU11274 group (group GS), and erlotinib combined with SU11274 group (group ES). The groups S, G, E, GS, and ES were added with 5 umol/L SU11274, 1 umol/L gefitinib, 1 umol/L erlotinib, 1 μmol/L gefitinib+5 μmol/L SU11274, and 1 μmol/L erlotinib+5 μmol/L SU11274; group C was not added any drugs. At 72 h after administration, the cell proliferation was detected by using MTT method, and the apoptosis was detected by using flow cytometry. The protein expression of p-EGFR, p-STAT3, and p-AKT was detected by Western blotting.ResultsThe cell survival rates were lower in the groups GS and ES than in the groups G and E, and the cell survival rates of the combination groups were lower than that of group S (allP<0.05). The cell survival rates of groups G, E, GS, and ES were lower than that of group C (allP<0.05), The early apoptosis rates of the groups GS and ES were higher than those of the groups G and E respectively, and both groups were lower than group S (allP<0.05). The early apoptosis rates of groups GS, ES, and S were higher than that of the group C (allP<0.05). The protein expression of p-EGFR, p-STAT3, and p-AKT of the groups GS and ES were lower than those of the groups G and E, respectively (allP<0.05). The protein expression of p-EGFR, p-STAT3, and p-AKT of the combination group was lower than that of the group S, and the protein expression of p-EGFR, p-STAT3, and p-AKT of the groups G, E, GS, and ES was lower than that of the group C (allP<0.05).ConclusionsSU11274 combined with gefitinib or erlotinib can inhibit the proliferation and promote apoptosis of the EGFR-TKI resistance lung cancer cells by inhibiting the function of EGFR pathway.
non-small-lung cancer; lung cancer cells; drug resistance; epidermal growth factor receptor-tyrosine kinase inhibitor; c-MET inhibitor; cell proliferation; apoptosis
10.3969/j.issn.1002-266X.2017.39.004
R734.2
A
1002-266X(2017)39-0015-04
玄香兰(1983-),女,硕士,主要研究方向为肺癌的基础与临床。E-mail: xuanxianglan101@hotmail.com
2017-08-25)