Herbst双期拔牙矫治对颞下颌关节位置影响的CBCT研究
陈维维 伍军 桑婷 黄臻
Herbst双期拔牙矫治对颞下颌关节位置影响的CBCT研究
陈维维 伍军 桑婷 黄臻

Herbst双期拔牙矫治; 颞下颌关节(TMJ); CBCT
1 资料与方法
1.1 病例选择

1.2 矫治设计

1.3 研究方法
1.3.1 CBCT扫描 所有研究对象均在Herbst矫治器矫治前2 周(T1期)、Herbst矫治器初戴入矫治时(T2期)、Herbst矫治器拆除时(T3期)及二期固定矫治器拆除时(T4期)分别进行CBCT(KAVO公司生产,扫描范围:直径16 cm×高度13 cm,管电压120 kV, 管电流5 mA,曝光时间14.7 s,扫描层厚0.25 mm)扫描。CBCT的拍摄均由放射科同一名医师按同一标准完成。
1.3.2 关节间隙测量 采用Invivo Dental软件对CBCT图像进行三维重建。作垂直于髁状突最大长轴的层切线,令其层切厚度为1 mm, 重建出垂直于髁状突长轴的一组斜位图像,选择处于中间的斜位图像为矢状位使用层。采用Kamelchuk[5]法在此层面上对关节上、前、后关节间隙进行测量,具体为:作平行于FH平面的直线L与关节窝上缘相切于切点S; 过S作L的垂线L1,位于关节间隙内的连线长度为关节上间隙SS;过S作髁突前缘的切线L2,再过髁突前缘切点作L2的垂线,位于关节间隙内的连线长度为关节前间隙AS;过S作髁突后缘的切线L3,再过髁突后缘切点作L3的垂线,位于关节间隙内的连线长度为关节后间隙SS(图 1)。
1.4 统计学方法
采用SPSS 17.0软件进行配对t检验,检验水准为α=0.05。
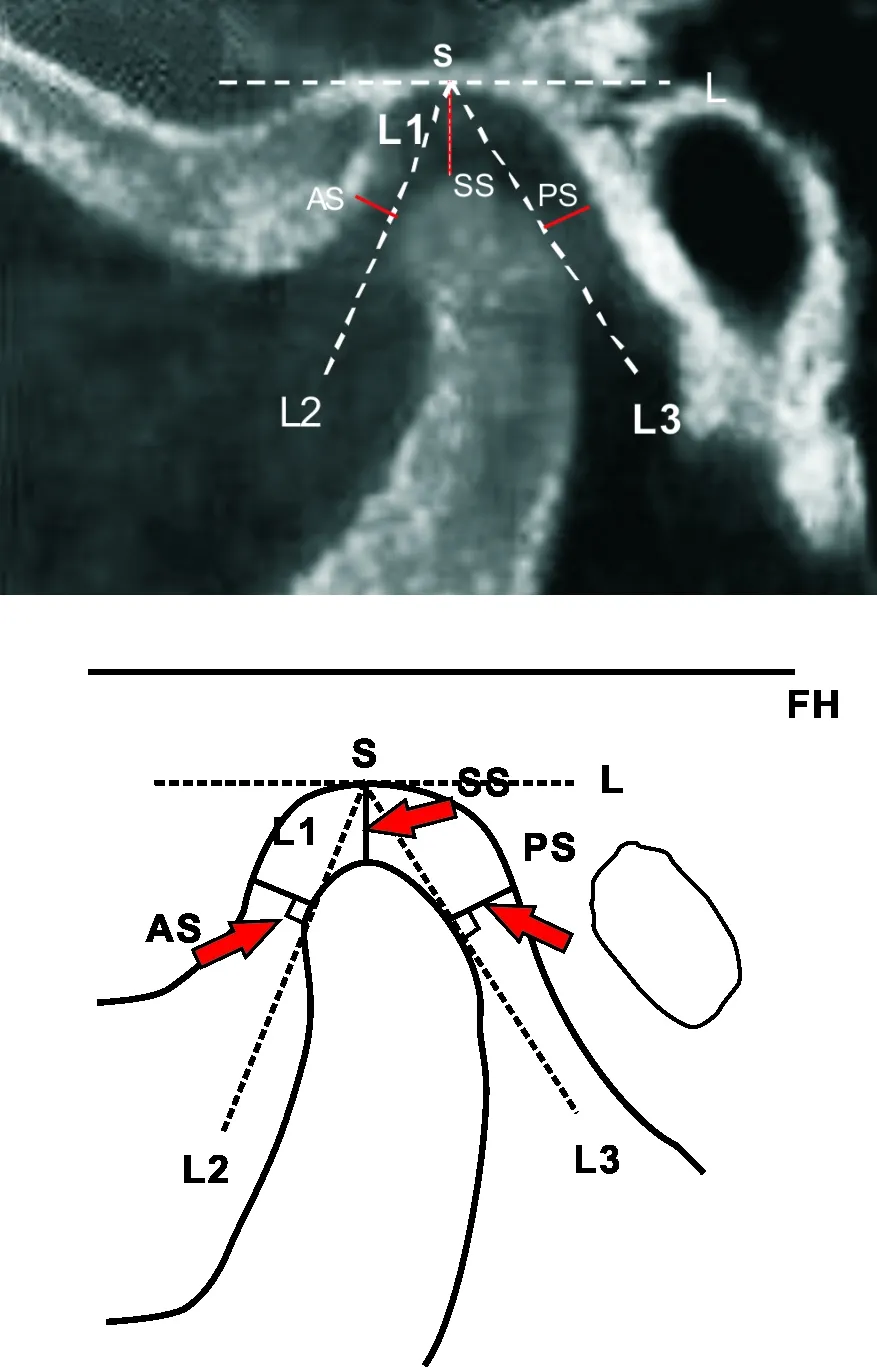
SS: 关节上间隙; AS: 关节前间隙; PS: 关节后间隙
SS: Superior joint space; AS: Anterior joint space; PS: Posterior joint space
Fig 1 Measurements of superior, anterior and posterior joint space
2 结 果
2.1 临床疗效
2.2 测量结果
治疗前左右两侧颞下颌关节间隙、不同时期颞下颌关节间隙及间隙变化量见表 1~3。
由表 1可见,治疗前左、右两侧颞下颌关节间隙无明显差异(P>0.05)。因此,将左、右两侧间隙合并,取其平均值计算。
表 1 治疗前左、右两侧颞下颌关节间隙测量值比较
Tab 1 Comparison of TMJ joint space measurements before treatment between left and right side

(mm, ±s)
表 2 不同治疗时期颞下颌关节间隙测量值

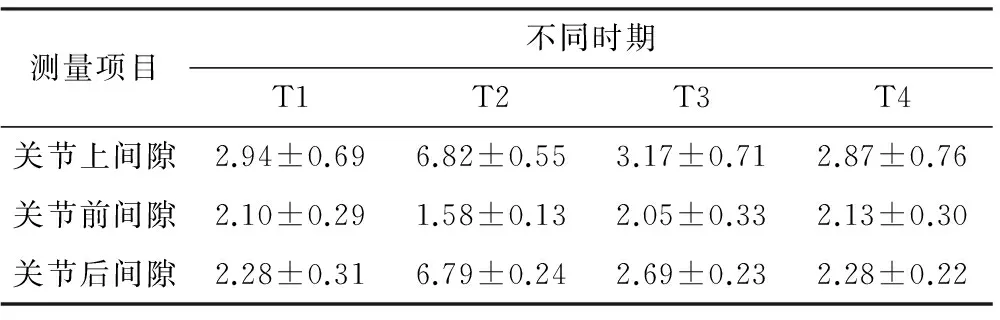
由表2~3及图 2可见, T1-T2-T3期,关节前间隙先减小后增大,关节上间隙、关节后间隙先增大后减小,T3期髁突几乎回复至T1期位置; 与T3期比,T4关节上、后间隙进一步减小,关节前间隙无明显变化,髁突进一步向T1期位置回复;与T1期比,T4各关节间隙的变化均无明显差异,说明双期矫治结束后髁突相对于关节窝回到了治疗前的位置。
表 3 不同治疗时期颞下颌关节间隙变化测量值比较
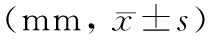

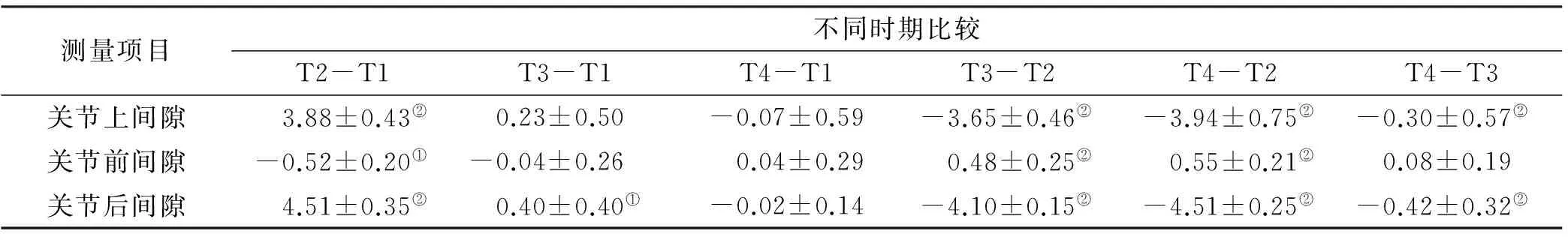
注:①P<0.05; ②P<0.01
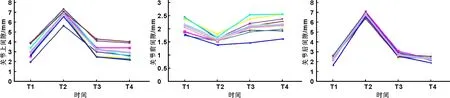
图 2 不同治疗时期关节上、前、后间隙变化趋势
3 讨 论
髁突在关节窝中的位置可以通过三维的关节间隙来确定[6]。 目前常用的关节间隙测量方法主要包括Madsen[7]、Kamelchuk[5]和张震康等[8]的线距定量测量方法以及Pullinger[9]和Rammelsberg等[10]的面积定量测量方法。王瑞永等[11]在CBCT图像上通过以上5 种测量方法测量关节间隙来分析正常成年人髁突在关节窝中的位置,结果发现5 种测量方法均显示髁突基本位于关节窝的中央位置,且5 种测量方法测量关节间隙差异均无显著性, 但是认为面积测量方法相对复杂,不便于临床应用。Ikeda[12]和Leonardi[13]等在CBCT图像上均采用Kamelchuk[5]测量方法来评价髁突的位置,所以本文也选用了Kamelchuk[5]线性测量方法来研究颞下颌关节间隙的改变情况。
目前,功能矫形治疗前移下颌后是否会改变髁突在关节窝中的位置,国内外学者研究结果不尽相同。Arat等[14]应用MRI研究Activator功能矫治器矫治安氏Ⅱ类1分类患者颞下颌关节髁突与关节窝的相对位置,发现矫治结束后关节前间隙明显减小,关节后间隙增加,髁突位置偏前。同样,Chintakanon等[15]在对Twin-block矫治器矫治患者的MRI研究中发现,功能矫治器矫治后大多数下颌后缩患者髁突位置比未治疗者更偏前位,且髁突相对关节窝有不同程度的前移,因此,认为髁突在矫治力的作用下,发生进行性软骨增生的同时还伴随位置的前移。然而,大多数的学者通过研究后,认为功能矫治器矫治安氏Ⅱ类下颌后缩患者,髁突在关节窝中的位置有回复至矫治前的位置的趋势,功能矫治结束后并不会改变髁突在关节窝中的位置[4,16]。Ruf 等[4]采用MRI研究Herbst矫治器矫治安氏Ⅱ类患者,发现Herbst功能矫治器矫治结束时髁突向前移位,但是功能矫治结束1 年后,髁突位置与治疗前无显著差异。Croft等[16]采用Herbst矫治器矫治40 例处于混合牙列时期的安氏Ⅱ类下颌后缩患者,评估Herbst矫治前(T1期),Herbst矫治器拆除前(T2期)及保持后(T3期,在治疗2.7 年后)颞下颌关节髁突的位置,发现治疗阶段(T1-T2)髁突位置处于前移位状态,但是保持阶段(T2-T3)关节后间隙显著减小了0.7 mm,总的阶段(T1-T3)关节后间隙减小了0.4 mm,认为Herbst矫治器在治疗阶段虽使髁突前移,但治疗2.7 年后髁突位置回复,甚至相对于治疗前关节后间隙反而略有减小。
本研究发现下颌后缩患者在Herbst矫治器初戴时(T2期),髁突相对于关节窝的位置与Herbst矫治器治疗前(T1期)明显不同,其关节前间隙明显减小,关节后、上间隙明显增大,说明髁突向前下方移位。但是在Herbst矫治器拆除时(T3期)髁突位置几乎回复至治疗前的位置,与Herbst矫治器初戴时(T2期)比较,关节前间隙明显增大,关节后、上间隙明显减小;与Herbst矫治器矫治前(T1期)比较,虽然关节后间隙略有增加,但是关节前间隙、关节上间隙都没有明显变化。固定矫治器拆除时(T4期)髁突回复至初始位置,与Herbst矫治器治疗前(T1期)比较没有明显的差异。
因此,本研究结果提示,对于安氏Ⅱ类下颌后缩患者采用Herbst双期拔牙矫治后并不会改变颞下颌关节髁突位置,这与Ruf 等[4]和Croft等[16]的研究结论相似,即Herbst功能矫治过程中的髁突移位只是暂时性的,最终会回复至初始位置。但本研究仅观察到固定矫治结束时,今后有望对患者进行进一步的回访跟踪研究,或将更有实际意义。
[1] Franchi L, Alvetro L, Giuntini V, et al. Effectiveness of comprehensive fixed appliance treatment used with the forsus fatigue resistant device in class II patients[J]. Angle Orthod, 2011, 81(4): 678-683.
[2] Pancherz H. The Herbst appliance—Its biologic effects and clinical use[J]. Am J Orthod, 1985, 87(1): 1-20.
[3] Aidar LA, Dominguez GC, Yamashita HK, et al. Changes in temporomandibular joint disc position and form following Herbst and fixed orthodontic treatment[J]. Angle Orthod, 2010, 80(5): 843-852.
[4] Ruf S, Pancherz H. Does bite-jumping damage the TMJ? A prospective longitudinal clinical and MRI study of Herbst patients[J]. Angle Orthod, 2000, 70(3): 183-199.
[5] Kamelchuk LS, Grace MG, Major PW. Post-imaging temporomandibular joint space analysis[J]. Cranio, 1996, 14(1): 23-29.

[7] Madsen B. Normal variations in anatomy, condylar movements, and arthrosis frequency of the temporomandibular joints[J]. Acta Radiol Diagn(Stockh), 1966, 4(3): 273-288.
[8] 张震康, 赵福运, 孙广熙, 等. 正常成年人颞颌关节100侧X线分析[J]. 中华医学杂志, 1975, 55(3): 130-132.
[9] Pullinger A, Hollender L. Variation in condyle-fossa relationships according to different methods of evaluation in tomograms[J]. Oral Surg Oral Med Oral Pathol, 1986, 62(6): 719-727.
[10]Rammelsberg P, Jäger L, Duc JM. Magnetic resonance imaging-based joint space measurements in temporomandibular joints with disk displacements and in controls[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2000, 90(2): 240-248.
[11]王瑞永,马绪臣,张万林,等. 健康成年人颞下颌关节间隙锥形束计算机体层摄影术测量分析[J]. 北京大学学报(医学版), 2007, 39(5): 503-506.
[12]Ikeda K, Kawamura A. Assessment of optimal condylar position with limited cone-beam computed tomography[J]. Am J Orthod Dentofacial Orthop, 2009, 135(4): 495-501.
[13]Leonardi R, Caltabiano M, Cavallini C, et al. Condyle fossa relationship associated with functional posterior crossbite, before and after rapid maxillary expansion[J]. Angle Orthod, 2012, 82(6): 1040-1046.
[14]Arat ZM, Gökalp H, Erdem D, et al. Changes in the TMJ disc-condyle-fossa relationship following functional treatment of skeletal Class II Division 1 malocclusion: a magnetic resonance imaging study[J]. Am J Orthod Dentofacial Orthop, 2001, 119(3): 316-319.
[15]Chhintakanon k, Sampson W, Wilkinson T, et al. A prospective study of Twin-block appliance therapy assessed by magnetic resonance imaging[J]. Am J Orthod Dentofacial Orthop, 2000, 118(5): 494-504.
[16]Croft RS, Buschang PH, English JD, et al. A cephalometric and tomographic evaluation of Herbst treatment in the mixed dentition[J]. Am J Orthod Dentofacial Orthop, 1999, 116(4): 435-443.
TheeffectsofHerbsttwophasetreatmentontemporomandibularjointpositionanalyzedbyCBCT
CHENWeiwei1,WUJun2,SANGTing2,HUANGZhen2.
1. 330006,DepartmentofStomatology,ThetraditionalChineseMedicineandWesternMedicineCombinationHospitalofNanchangCity,China; 2.DepartmentofOrthodontics,TheaffiliatedStomatologicalHospitalofNanchangUniversity
Objective: To assess the effects of Herbst two phase treatment on temporomandibular joint(TMJ) position analyzed by CBCT.Methods15 patients of permanent dentition with classⅡ malocclusion combined with mandibular retrusion were treated by Herbst appliance as the 1st phase, then the 4 1st premolars of each patient were extracted, the fixed appliance of edgewise was applied as the 2nd phase of treatment. CBCT examination was carried out at the following stages: 2 weeks before Herbst treatment(T1), at the start of the treatment when Herbst appliance was placed(T2), immediately after Herbst appliance was removed(T3) and immediately after the edgewise appliance was removed(T4). The InvivoDental software was used to calculate the joint space of TMJ from the three-dimensional CBCT images. The acquired data were then statistically analyzed.ResultsDuring T1-T2-T3 stages, the anterior joint space was decreased and then increased, superior joint space and posterior joint space were increased and then decreased. During T3-T4 stages, the superior joint space and posterior joint space decreased further, but anterior joint space did not change. No significant difference was found in the anterior joint space, superior joint space and posterior joint space between T1 and T4 stage.ConclusionAt the start of treatment with Herbst appliance,the condyle is displaced in an anterior and inferior direction. At the end of functional treatment, especially the end of two phase treatment, the condyle is drawed back nearly to the original position.
Herbsttwophasetreatment;Temporomandibularjoint(TMJ);CBCT
江西省卫生厅科技计划(编号: 20133080)
330006, 南昌市中西医结合医院口腔科(陈维维); 南昌大学附属口腔医院正畸科(伍军 桑婷 黄臻)
伍军 0791-86236950 E-mail: wujundent@163.com
R783.5
A
10.3969/j.issn.1001-3733.2017.04.014
(收稿: 2016-11-25 修回: 2017-01-13)