肘关节“恐怖三联征”合并肱骨远端骨折的手术治疗
吴加东 卞化 沈孝天 王超 孙焕建 王友华 刘璠
肘关节“恐怖三联征”合并肱骨远端骨折的手术治疗
吴加东1卞化1沈孝天1王超1孙焕建1王友华2刘璠2
目的探讨手术治疗肘关节“恐怖三联征”合并肱骨远端骨折的临床疗效。方法选择东南大学医学院附属盐城医院2005年1月至2014年6月收治的13例肘关节“恐怖三联征”合并肱骨远端骨折患者,男8例,女5例,年龄24~56岁,平均(31.4±2.1)岁,肱骨远端骨折AO分型:B1型3例,C1型7例,C2型3例。肱骨远端骨折行钢板固定,桡骨头骨折行钢板、螺钉固定或置换,冠突骨折行钢板、螺钉或克氏针固定,修复内外侧副韧带。术后按照Broberg-Morrey评估系统对肘关节功能进行评分。结果11例患者获得随访,随访时间12~22个月,平均(16.2±2.1)个月。骨折愈合时间19~23周,平均(20.2±3.2)周。Broberg-Morrey评分:优2例(18.2%)、良6例(54.5%)、可2例(18.2%)、差1例(9.1%),优良率72.7%。肘关节屈伸范围75~116°,平均(101.2±10.9)°;前臂旋转范围为90~120°,平均(107.7±8.4)°。结论 肘关节“恐怖三联征”合并肱骨远端骨折为高能量损伤,关节严重不稳定,需重建骨关节及软组织的解剖结构,肘关节功能可得到良好恢复。
肘关节; 恐怖三联征; 肱骨远端骨折
随着工业及交通业的迅猛发展,复杂肘关节骨折脱位其发生率在临床上逐年增加,人们对此已倍加关注。Hotchkiss[1]于1996年首次将肘关节后脱位伴桡骨头和冠状突骨折命名为“恐怖三联征”。其合并肱骨远端骨折,继发于肘关节伸直位遭受垂直轴向的巨大暴力,肱骨远端与尺桡骨近端直接撞击所致,因内外侧副韧带起止点的解剖特性,其常常连带着肱骨远端骨块一起牵扯移位,故此类损伤较单纯性“恐怖三联征”相比,往往骨性结构破坏更重。本文采用重建损伤的骨性结构、关节囊及韧带的方法治疗13例患者,其中11例获得随访,疗效满意,报道如下。
资料与方法
一、一般资料
2005年1月至2014年6月收治的13例肘关节“恐怖三联征”合并肱骨远端骨折患者,男8例、女5例,均为闭合性损伤,其中合并尺神经损伤2例。年龄24~56岁,平均(31.4±2.1)岁,致伤原因:交通伤7例(53.8%)、坠落伤4例(30.8%)、其他伤2例(15.4%)。肱骨远端骨折AO分型:B1型3例,C1型7例,C2型3例。桡骨头骨折分型按Mason分型[2]:Ⅱ型8例,Ⅲ型5例。因合并肘关节脱位,按照Johnston-Mason分型[3]均为Ⅳ型。尺骨冠突骨折按照Regan-Morrey分型[4]:Ⅰ型2例,Ⅱ型4例,Ⅲ型7例。急诊闭合复位,长臂石膏托临时固定。受伤至手术时间3~10 d,平均5.2 d。
二、术前准备与手术方法
术前常规行X线、CT检查以明确骨折分型。使用甘露醇、七叶皂苷等消肿,待局部软组织条件允许后行手术治疗,术中预防使用抗生素。
臂丛麻醉或全麻下,取侧卧位,患肢置于侧胸壁,取肘后“S”型切口,潜行分离皮下,解剖保护尺神经,先用2枚克氏针或电钻自尺骨鹰嘴尖向尺骨远端钻通骨隧道备用,距尺骨近端约2cm处做“V”形截骨,向近端翻转附带肱三头肌肌腱的鹰嘴骨块,将髁间骨折转变为髁上骨折, 解剖型钢板固定于肱骨远端后外侧及(或)内上髁嵴上,将鹰嘴截骨块复位, 行张力带内固定。从肘肌和尺侧腕伸肌间隙进入显露桡骨头骨折,安全区内置放钢板螺钉或桡骨头置换。取肘前内侧切口,自尺侧腕屈肌的两头之间进入,自前向后或自后向前双头加压螺钉固定冠突骨块,若骨块较小,自前向后克氏针固定,从鹰嘴背侧引出,折弯剪短预置于尺骨背面。肘关节后脱位常伴有不同程度内外侧副韧带损伤,若起止点撕脱,用锚钉固定骨面,若体部断裂,用不可吸收缝线编织缝合,对尺神经有原发性损伤或术中发现内固定物与尺神经毗邻时,需将尺神经前置于皮下筋膜。检查肘关节在屈伸30~130°范围内未发生脱位,提示关节相对稳定,C型臂X线机透视再次确认关节在位,骨折复位良好,内固定位置满意。所有患者具体骨折类型和治疗方式见表1。
三、术后处理及评估
常规口服吲哚美辛12.5 mg/d,1次/d,预防骨化性肌炎的发生。术后以可屈性支具固定,3 d后即指导肘关节康复锻炼,包括肘关节屈伸及前臂旋转功能,逐步加大主动训练。患者均于术后第1、3、6及12个月定期随访。评估项目包括:肘关节屈伸和前臂旋转范围。功能评估采用Broberg和Morrey评估系统[5]:满分100分,包括运动40分、力量20分、疼痛35分、稳定性5分等4方面。
结 果
13例患者中11例获得随访,随访时间12~22个月,平均(16.2±2.1)个月。骨折愈合时间19~23周,平均(20.2±3.2)周。肘关节屈伸范围 75~116°,平均(101.2±10.9)°;前臂旋转范围为 90~120°,平均(107.7±8.4)°。术后 3例出现肘关节僵硬,骨化性肌炎1例,创伤性关节炎1例,无深部感染、内固定物松动断裂的发生,2例合并尺神经损伤患者术后经神经营养等治疗后逐步好转。Broberg-Morrey评分:优2例(18.2%)、良6例(54.5%)、可 2例(18.2%)、差1例(9.1%),优良率72.7%。典型病例见图1~3。
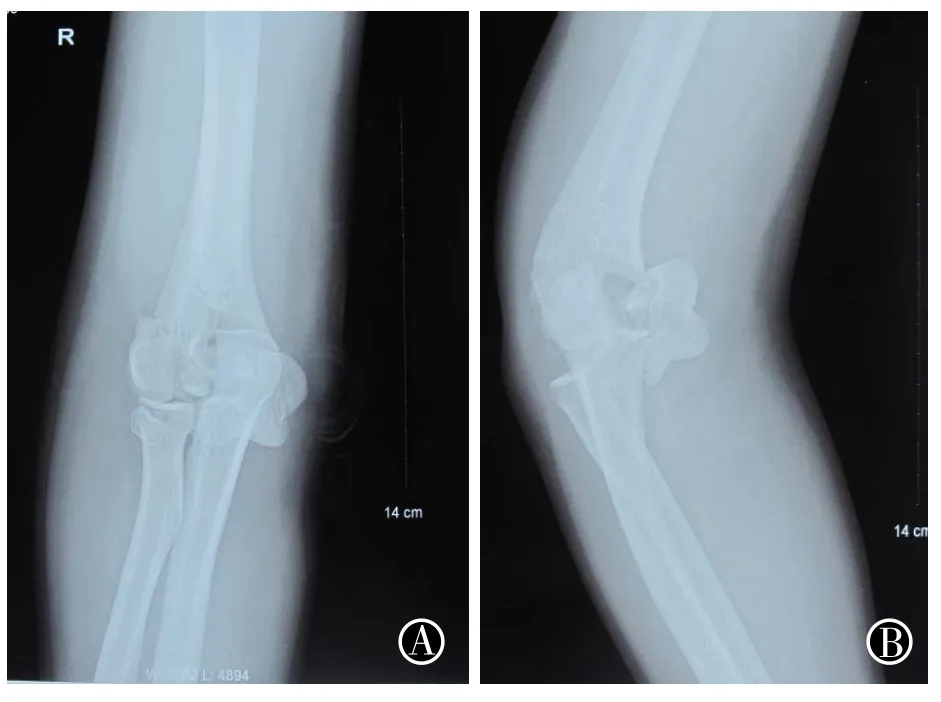
图1 肘关节“恐怖三联征”合并肱骨远端骨折术前正(A)、侧(B)位X线片
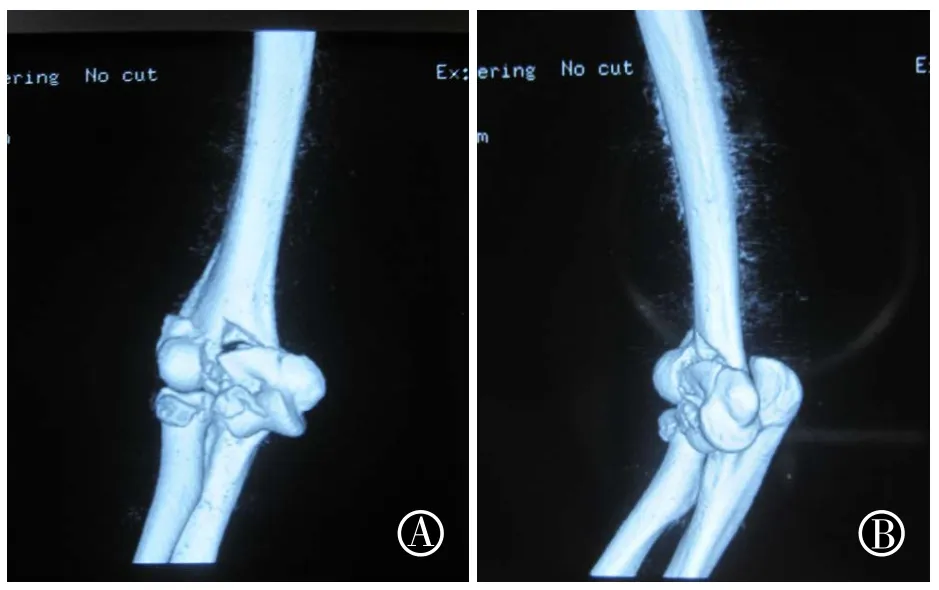
图2 肘关节“恐怖三联征”合并肱骨远端骨折术前正(A)、侧(B)位CT片

图3 肘关节“恐怖三联征”合并肱骨远端骨折术后正(A)、侧(B)位X线片
讨 论
肘关节稳定环分为内、外、前、后4柱。前柱包括冠状突、肱肌、前关节囊,后柱包括鹰嘴突、三头肌、后关节囊,内侧柱由尺侧副韧带、冠状突、内髁或内上髁组成,外侧柱由桡骨头、肱骨小头和桡侧副韧带组成。在成年桡骨头的生理作用包括两部分,即维持肘关节外侧的稳定性和传导应力。冠突系内侧副韧带前束附着部,和鹰嘴形成半月(滑车)切迹,与肱骨滑车构成肱尺关节。冠突骨折将致半月弧形关系不连续,肱尺关节紊乱。Hammacher等[6]把肘关节比喻成“希腊的庙宇”,桡骨和尺骨是两个“柱子”,支撑着“屋顶”—肱骨远端,屋顶与柱子间的连接在尺侧由韧带构成,在桡侧由肌肉的张力及韧带维系。肘关节“恐怖三联征”表现为桡骨头骨折、冠突骨折及肘关节脱位,其稳定环中的一柱或多柱受累,或“希腊”柱子中的任一支撑柱破坏,肘关节必将失稳。若前臂轴向暴力过大,同时合并肱骨远端骨折,骨性结构损伤较单纯“恐怖三联征”更为严重,肘关节稳定性彻底丧失,治疗相当棘手。
复杂肘关节骨折脱位,累及多柱,很难在单一切口内完成。肘后“S”形入路,可兼顾肱骨远端骨折及桡骨头骨折,筋膜皮瓣掀起后,鹰嘴“V”形截骨,可充分显露肱骨远端,单钢板或双钢板固定[7]。沿Kocher间隙(肘后肌及尺侧腕伸肌间隙)显露桡骨头,安全区内置放螺钉或钢板[8],通常桡骨头粉碎,内固定困难或无法实现坚强固定,推荐桡骨头置换,以利外侧柱可靠支撑。自肘关节尺侧腕屈肌的两头之间进入显露冠突,自前向后或自后向前双头加压螺钉固定冠突骨块,若骨块较小,自前向后克氏针固定,从鹰嘴背侧引出,折弯剪短预置于尺骨背面,操作简便可行,有报道用“套索”缝合固定或锚钉固定,其可行性及稳定性有待进一步验证。内侧副韧带损伤常见于体部或冠突附着部,外侧副韧带损伤常见于肱骨外髁附着部,若起止点撕脱,用锚钉固定骨面,若体部断裂,用不可吸收缝线编织缝合。
术后以可屈性支具固定,3 d后即指导肘关节康复锻炼,包括肘关节屈伸及前臂旋转功能,逐步加大主动训练。肘关节僵硬是复杂肘关节骨折脱位术后常见并发症,大部分患者伴有不同程度活动范围丧失。一般不推荐术后石膏固定,强调镇痛状态下(围手术期服用吲哚美辛、塞来昔布等)或配用铰链式外固定支架下早期功能锻炼[9-10],防止关节粘连。
作者发现,肘关节“恐怖三联征”合并肱骨远端骨折为高能量损伤,但内外侧副韧带常因关节上下附着骨结构同时骨折而分散受力,其损伤往往较单纯“恐怖三联征”脱位时的强行拽扯较轻,因此重建骨结构是关键,修复软组织损伤可最大程度的恢复其原有解剖形态及生理功能,临床随访,效果满意。
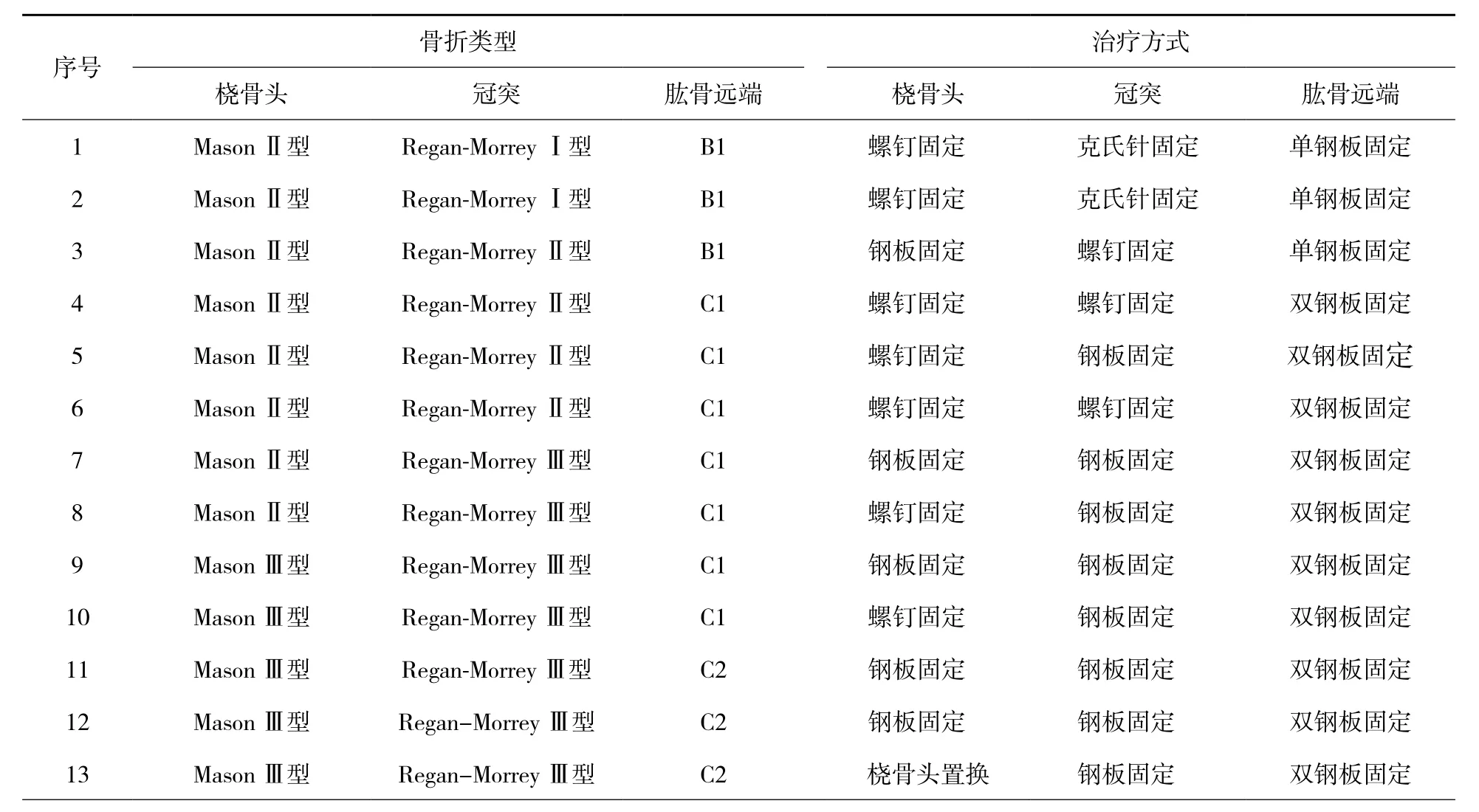
表1 13例患者的骨折类型和治疗方式
本文的局限性:(1)该类损伤是一个涉及多个骨折、多发韧带损伤的模型,其受伤机制复杂,因样本量小,未能将其软组织损伤情况与单纯“恐怖三联征”详细对比研究,这在今后的研究中值得进一步深入。(2)临床疗效随访仍需大样本、大数据支持。
[1]Hotchkiss RN. Fractures and dislocations of the elbow[M]//Rockwood CA, Green DP, Bucholz RW, et al. Rockwood and Green, s fractures in adults. 4th ed. Philadelphia: Lippincott-Raven, 1996:929-1024.
[2]Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases [J]. Br J Surg,1954, 42(172):123-132.
[3]Johnston GW. A follow-up of one hundred cases of fracture of the head of the radius with a review of the literature [J].Ulster Med J, 1962, 31(1): 51-56.
[4]Regan W,Morrey B. Fractures of the coronoid process of the ulna [J]. J Bone Joint Surg(Am),1989,71(9):1348-1354.
[5]Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture [J]. J Bone Joint Surg (Am),1986,68(5):669-674.
[6]Hammacher ER, van der Werken C. Radial head fractures:operative or conservative treatment? The Greek temple model[J]. Acta Orthop Belg, 1996, 62 (S 1): 112-115.
[7]吴加东, 许步伟, 周敦, 等. 肱骨远端解剖特点及双钢板治疗粉碎性骨折临床分析[J]. 中华手外科杂志, 2013, 29(2):104-106.
[8]吴加东, 孙焕建, 陆汉琴, 等. 桡骨近端“安全区”内微型钢板治疗桡骨头骨折的临床疗效[J]. 江苏医药, 2016, 42(8):949-950.
[9]吴加东, 刘国华, 陈海娟, 等.围手术期使用塞来昔布对肘关节僵硬松解术后疗效的评价[J]. 苏州大学学报(医学版),2011, 31(1):131-133.
[10]吴加东, 吕成堂, 周敦, 等. 铰链式外固定支架在桡骨头骨折伴肘关节不稳定治疗中的应用[J]. 中国骨与关节损伤杂志 , 2015, 30(1):98-99.
Shen Xiaotian, Email: sxt20101@163.com
Surgical treatment of terrible triad of the elbow combined with distal humeral fracture
Wu Jiadong1,Bian Hua1, Shen Xiaotian1, Wang Chao1, Sun Huanjian1, Wang Youhua2, Liu Pan2.1Department of Orthopaedics, The Affiliated Yancheng Hospital of Southeast University Medical College, Yancheng 224005, China;2Department of Orthopaedics, The Affiliated Hospital of Nantong University,Nantong 226001, China
BackgroundWith the rapid development of industry and transportation, the occurrence of complex elbow fractures and dislocations is increasing by years, to which people have paid more attention on. In 1996, the posterior elbow dislocation combined with radial head and coronoid process fractures was named as “terrible triad of elbow” by Hotchkiss. It is combined with distal humeral fractures, secondary to the great violence perpendicular to the long axis in elbow extension and the direct impact of distal humerus and proximal ulna. Due to the anatomical features of medial and lateral collateral ligaments attach points, it is often associated with distal humeral fragment. Therefore, compared with simple“terrible triad”, bone structure damage is often more severe in this type of injury.Methord(1)General information.From January 2005 to June 2014, 13 cases (8 males and 5 females) with terror triad of elbow combined with distal humerus fractures were treated, all of which were closed injuries, including 2 cases of ulnar nerve injuries. The ages were 24-56 years with an average of (31.4 ±2.1) years. Causes of injuries included 7 cases of traffic injuries (53.8%), 4 cases of falling injuries (30.8%) and 2 cases of other injuries (15.4%). AO classification of distal humeral fractures: 3 cases of type B1, 7 cases of type C1 and 3 cases of type C2. Radial head fractures were classified according to Mason classification, including 8 cases of type Ⅱ and 5 cases of type Ⅲ . According to Johnston-Mason classification, all the cases were type IV fractures because of the combined elbow dislocations. Coronoid process fractures of ulna were classified according to Regan-Morrey classification, including 2 cases of type I, 4 cases of type Ⅱ and 7 cases of type Ⅲ. Closed reduction was conducted in the emergency department with long arm plaster for temporary immobilization. The time from injury to surgery was 3-10 days with an average of 5.2 days. (2)Preoperative preparation and operative methods.X-ray and CT examinations were performed routinely to define the fracture patterns. Mannitol and aescinate were used to reduce swelling. Operation was conducted as the local soft tissue condition permitted, and antibiotics were given to prevent infection intraoperatively.Under brachial plexus block or general anesthesia, the patient was in lateral position with the affected limb on the ipsilateral chest. An “S” shape incision was made to separate subcutaneous tissue and then anatomize and protect ulnar nerve. Firstly, a bone tunnel was prepared with two Kirschner wires or electric drill from the tip of olecranon to the distal ulna. A "V" shaped osteotomy was conducted approximately 2 cm from the proximal ulna. The olecranon fragment with triceps tendon was inverted proximally, and the intercondylar fracture was transformed to supracondylar fracture. The anatomical plates were fixed on the posterolateral site of distal humerus and (or) the epicondylic ridge, and the olecranon fragment was fixed by using tension band after reduction. The radial head fracture was exposed through the gap between anconeus and cubitalis posterior. Then the plate and screws were placed in the safe area or the radial head replacement was performed instead. Through the anteromedial incision of elbow and the gap between two heads of cubitalis anterior, the coronoid process fragment was fixed with double-head compression screw from anterior to posterior or from posterior to anterior. If the fragment was small, it could be fixed from anterior to posterior with Kirschner wire that came out from the back of olecranon, bended and clipped and placed on the back of ulna. Posterior dislocation of elbow joint was often combined with various degrees of medial and lateral collateral ligaments. The bone surface should be fixed with anchor if the attachment point was avulsed, and the ligament body, if ruptured, should be knitted with non-absorbable sutures. The ulnar nerve should be placed in the subcutaneous fascia if it had primary injury or was adjacent to internal fixators. If the elbow joint was not dislocated with in 30-130° of flexion and extension during examination, it was relatively stable.With the further confirmation under fluoroscopy, the fracture was well restored and the location of internal fixation was satisfactory. (3)Postoperative management and evaluation.Oral indomethacin was taken routinely with 12.5 mg one day at a time to prevent the occurrence of heterotopic ossificans. The flexible brace could be used for fixation after operation, and the elbow rehabilitation exercises were guided 3 days later, including elbow flexion and extension and forearm rotation with gradual increase of active training. All patients were followed up regularly in the 1st, 3rd, 6th and 12th month after operation. Assessment projects included the range of elbow flexion and extension and forearm rotation. Broberg and Morrey evaluation system was used for functional evaluation. The total score was 100 points in 4 aspects, including 40 points of motion, 20 points of strength, 35 points of pain and 5 points of stability.ResultsOf the 13 patients, 11 cases were followed up for 12-22 months with an average of (16.2±2.1) months. The fracture healing time was 19-23 weeks with an average of (20.2±3.2) weeks. The range of elbow flexion and extension was 75-116° with an average of (101.2±10.9)°; the range of forearm rotation was 90-120° with an average of (107.7±8.4)°. After operation, 3 cases had elbow stiffness, 1 case had heterotopic ossificans and 1 case had traumatic arthritis. No deep infection, internal fixator loosening or breakage occurred. Two cases combined with ulnar nerve injuries had gradually improved after neurotrophic therapy. Broberg-Morrey score: 2 excellent cases (18.2%), 6 good cases (54.5%), 2 moderate cases (18.2%) and 1 poor case(9.1%). The good and excellent rate was 72.7%.ConclusionThe terrorist triad of elbow combined with distal humeral fracture is an high energy injury. However, as fractures occur at both proximal and distal bone structures attached by elbow joint, the injuries to medial and lateral collateral ligaments are less severe compared to that of forced pulling during joint dislocations in the terrible triad. Therefore, the reconstruction of bone structures is the key. Soft tissue repair can maximize the restoration of its original anatomy and physiological function, and the outcomes of clinical follow ups are satisfactory.
Elbow joint; Terrible triad of the elbow; Distal humeral fracture
10.3877/cma.j.issn.2095-5790.2017.03.007
盐城市医学科技发展计划项目(YK2013068)
224005 东南大学医学院附属盐城医院(盐城市第三人民医院)骨科1;226001 南通大学附属医院骨科2
沈孝天,Email: sxt20101@163.com
2017-02-08)
(本文编辑:李静;英文编辑:陈建海、张晓萌、张立佳)
吴加东, 卞化,沈孝天,等. 肘关节“恐怖三联征”合并肱骨远端骨折的手术治疗[J/CD].中华肩肘外科电子杂志,2017,5(3):194-198.

