单核细胞/高密度脂蛋白比值与行急诊PCI的STEMI患者院内主要不良心血管事件的相关分析
于永福,王岚峰
单核细胞/高密度脂蛋白比值与行急诊PCI的STEMI患者院内主要不良心血管事件的相关分析
于永福1,王岚峰1
目的 探讨单核细胞/高密度脂蛋白比值(MHR)与行急诊经皮冠状动脉介入治疗(PCI)的急性ST段抬高型心肌梗死(STEMI)患者院内主要不良心血管事件(MACE)发生风险的关系。方法入选2015年10月~2016年6月于哈尔滨医科大学附属第一医院CCU病房行急诊PCI的286例STEMI患者,其中男性193例,女性93例,年龄40~80岁。根据住院1周内是否发生MACE将患者分为MACE组(131例)和非MACE组(155例)。由心血管介入医师行急诊冠状动脉造影检查,并行PCI。入院时测定总胆固醇、三酰甘油、高密度脂蛋白胆固醇(HDL-C)、低密度脂蛋白胆固醇(LDL-C)、C反应蛋白、肌酸激酶同工酶(CK-MB)、MHR、左室射血分数等。结果 与非MACE组比较,MACE组左室射血分数降低,CK-MB和MHR升高,差异有统计学意义(P均<0.05)。多因素Logistic回归分析,结果显示C反应蛋白(OR=1.009,95%CI:1.001~1.016)、左室射血分数(OR=0.934,95%CI:0.905~0.963)、CK-MB(OR=1.003,95%CI:1.001~1.004)是STEMI患者院内发生MACE的影响因素。MHR升高是STEMI患者院内发生MACE的危险因素。结论 MHR与行急诊PCI的STEMI患者发生主要不良心血管事件有关,MHR越大,主要不良心血管事件发生的风险越高。
单核细胞/高密度脂蛋白比值;STEMI;主要不良心血管事件
我国冠状动脉疾病的发病率逐年上升,北方发病率高于南方,城市发病率高于农村[1]。冠状动脉疾病的主要原因是动脉粥样硬化。已有研究表明炎症过程在动脉粥样硬化血栓形成和斑块破裂中起重要作用。急性ST段抬高型心肌梗死(STEMI)是冠心病的严重类型,虽然急诊经皮冠状动脉介入治疗(PCI)有效挽救了濒死心肌,缩小梗死范围,改善预后,但仍有院内主要不良心血管事件(MACE)发生。本研究旨在探讨单核细胞/高密度脂蛋白比值(MHR)与行急诊PCI的STEMI患者院内MACE发生风险的相关性。
1 资料与方法
1.1 研究对象和分组 入选2015年10月~2016年6
月于哈尔滨医科大学附属第一医院CCU病房行急诊PCI的286例STEMI患者,其中男性193例,女性93例,年龄40~80岁。所有患者均符合急性心肌梗死的诊断标准[2]。排除标准:住院前1个月内服用他汀类及其他调脂药物者;拒绝或无法行冠状动脉造影者;资料不完整者。根据是否发生MACE将患者分为MACE组(131例)和非MACE组(155例)。MACE指住院一周内发生,包括心力衰竭、严重心律失常(室速/室颤、房颤及传导阻滞)、心肌梗死后心绞痛及死亡。
1.2 方法 入院时行二维彩色多普勒心脏超声检查,并记录左室射血分数(LVEF)。随即由心血管介入医师行急诊冠状动脉造影检查,并行PCI。在入院时抽取肘静脉血使用双试剂循环酶法检测血常规、总胆固醇、三酰甘油、高密度脂蛋白胆固醇(HDL-C)、低密度脂蛋白胆固醇(LDL-C)、C反应蛋白、肌酸激酶同工酶(CK-MB)等。
1.3 统计学分析 所有统计学分析使用SPSS 19.0软件,计量资料采用均数±标准差(x±s)表示,两组间均数的比较采用t检验,计数资料采用例数/构成比表示,组间比较采用χ2检验。采用多因素Logistic回归分析MHR和MACE的相关性。P<0.05为差异有统计学意义。
2 结果
2.1 两组基本资料比较 两组年龄、性别比、吸烟比例、高血压比例、糖尿病比例、单核细胞和血脂比较,差异无统计学意义(P均>0.05)。与非MACE组比较,MACE组左室射血分数降低,CK-MB和MHR升高,差异有统计学意义(P均<0.05)(表1)。
2.2 STEMI患者院内发生MACE的影响因素 多因素Logistic回归分析,结果显示C反应蛋白(OR=1.009,95%CI:1.001~1.016)、LVEF(OR=0.934,95%CI:0.905~0.963)、CK-MB(OR=1.003,95%CI:1.001~1.004)是STEMI患者院内发生MACE的影响因素。以Q3为对照,Q1、Q2的OR值均小于1,MHR升高是STEMI患者院内发生MACE的危险因素(表2)。
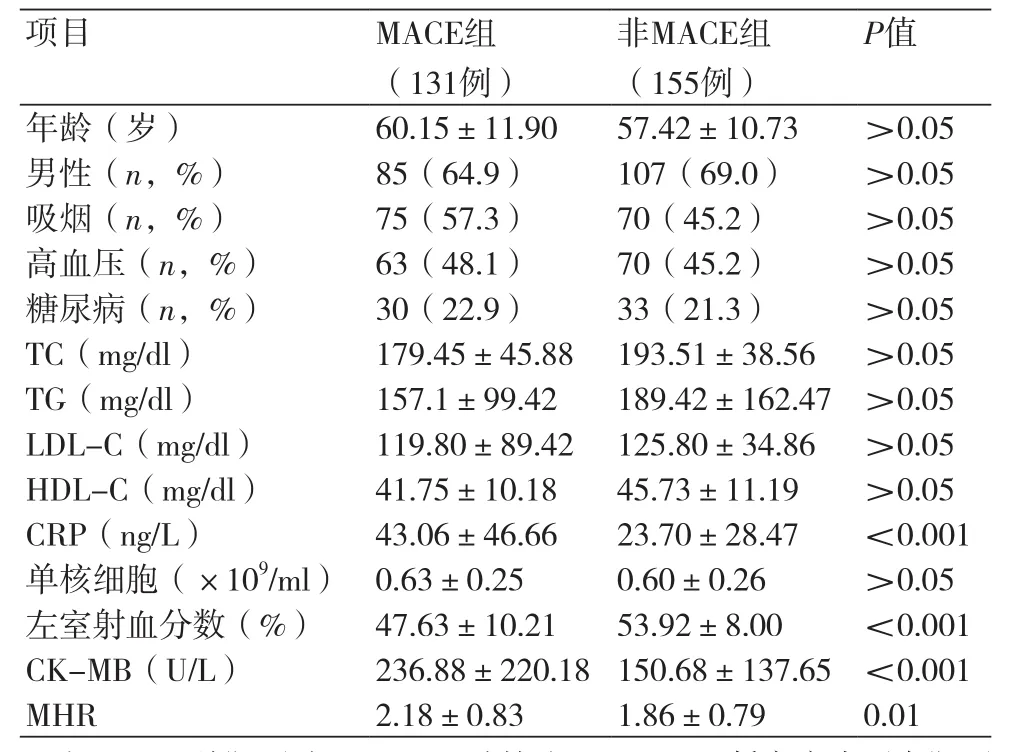
表1 两组患者基本特征比较
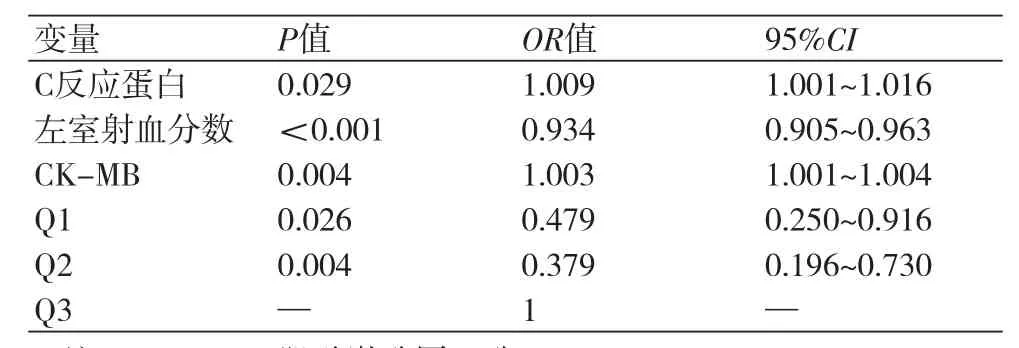
表2 STEMI患者院内发生MACE的影响因素
3 讨论
动脉粥样硬化和斑块破裂是STEMI的主要原因。炎症在动脉粥样硬化中起关键作用。炎症与STEMI的MACE有关[2]。急诊PCI是STEMI的首选治疗方式,可以明显减少患者6个月内死亡和再次心肌梗死的发生。炎症相关指标是患者短期和长期死亡的预测因子[2,3]。白细胞、淋巴细胞、中性粒细胞/淋巴细胞比值、C反应蛋白和血小板/淋巴细胞比值与炎症致动脉粥样硬化有关[4-9]。
单核细胞为巨噬细胞和泡沫细胞的来源,也是斑块进展的预测因子[10]。内皮功能障碍导致单核细胞、淋巴细胞易于粘附,其通过吸收氧化的低密度脂蛋白和其他脂质发展为巨噬细胞和异化为泡沫细胞[11]。泡沫细胞形成脂质条纹,分泌促炎因子,加重局部炎症反应。单核细胞和巨噬细胞在动脉粥样硬化斑块形成和破裂的各个时期均起作用,可导致STEMI[11,12]。
高密度脂蛋白(HDL)已被证实具有抗炎、抗氧化和抗动脉粥样硬化血栓形成作用[13,14]。HDL有效抑制内皮细胞粘附分子的表达,防止单核细胞在动脉壁募集[15]。低水平的HDL和高水平的LDL是急性冠脉综合征的独立预测因子[16,17]。
在慢性肾脏病患者中发现,MHR增加与不良心血管预后有关。有研究发现[18],MHR增高是冰冻球囊导管消融后房颤复发的一个预测因子,围手术期患者MHR>11.48,房颤复发风险增加11.2倍。本研究中,高MHR与低MHR相比,MACE发生风险增高。本研究为单中心研究,并且样本数量少,仅分析了入院MHR的水平,而MHR在心肌梗死急性期后的水平未被考虑。
[1] 陈伟伟,高润霖,刘力生,等. 《中国心血管病报告2015》概要[J].中国循环杂志,2015, 31(7):617-22.
[2] Rasoul S,Ottervanger JP,de Boer MJ,et al. Predictors of 30-day and 1-year mortality after primary percutaneous coronary intervention for ST-elevation myocardial infarction[J]. Coronary Artery Disease,2009,20(6):415.
[3] Kushner FG,Hand M,Smith Jr SC,et al. 2009 Focused Updates: ACC/ AHA Guidelines for the Management of Patients With ST Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention(updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines[J]. Circulation,2009,120(22):2271-306.
[4] Nikolsky E,Grines CL,Cox DA,et al. Impact of baseline platelet count in patients undergoing primary percutaneous coronary intervention in acute myocardial infarction (from the CADILLAC trial)[J]. Am J Cardiol,2007,99:1055-61.
[5] Iijima R,Ndrepepa G,Mehilli J,et al. Relationship between platelet count and 30 day clinical outcomes after percutaneous coronary interventions. Pooled analysis of four ISAR trials[J]. Thromb Haemost, 2007,98(4):852-7.
[6] Ommen SR,Gibbons RJ,Hodge DO,et al. Usefulness of the lymphocyte concentration as a prognostic marker in coronary artery disease[J]. Am J Cardiol,1997,79(6):812-4.
[7] Tamhane UU,Aneja S,Montgomery D,et al. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome[J]. Am J Cardiol,2008,102(2):653-7.
[8] Makrygiannis SS,Ampartzidou OS,Zairis MN,et al. Prognostic usefulness of serial C-reactive protein measurements in ST-elevation acute myocardial infarction[J]. Am J Cardiol,2013,111(1):26-30.
[9] Oylumlu M,Yild iz A,Oylumlul M,et al. Platelet-to-lymphocyte ratio is a predictor of in-hospital mortality patients with acute coronary syndrome[J]. Anatol J Cardiol,2015,15(4):277-83.
[10] Kanbay M,Solak Y,Unal HU,et al. Monocyte count/HDL cholesterol ratio and cardiovascular events in patients with chronic kidney disease[J]. Int Urol Nephrol,2014,46(8):1619-25.
[11] Steinberg D,Witztum JL. Is the oxidative modi fication hypothesis relevant to human atherosclerosis? Do the antioxidant trials conducted to date refute the hypothesis?[J]. Circulation,2002,105:2107-11.
[12] Moreno PR,Purushothaman KR,Fuster V,et al. Intimomedial interface damage and adventitial inflammation is increased beneath disrupted atherosclerosis in the aorta: implications for plaque vulnerability[J]. Circulation,2002,105(21):2504-11.
[13] Karabacak M,Kahraman F,Sert M,et al. Increased plasma monocyte chemoattractant protein-1 levels in patients with isolated low highdensity lipoprotein cholesterol[J]. Scand J Clin Lab Inves,2015,75(4):327-32.
[14] Barter PJ,Nicholls S,Rye KA,et al. Antiin flammatory properties of HDL[J]. Circ Res,2004,95:764-72.
[15] Cockerill GW,Rye KA,Gamble JR,et al. High-density lipoproteins inhibit cytokine-induced expression of endothelial, cell adhesion molecules[J]. Arterioscler Thromb Vasc Biol,1995,15:1987-94.
[16] Kahveci G,Bayrak F,Mutlu B,et al. Clinical signi ficance of highdensity lipoprotein cholesterol in left-sided infective endocarditis[J]. Am J Cardiol,2008,101(8):1170-3.
[17] Reddy VS,Bui QT,Jacobs JR,et al. Relationship between serum lowdensity lipoprotein cholesterol and in-hospital mortality following acute myocardial infarction[J]. Am J Cardiol,2015,115(5):557-62.
[18] Canpolat U,Aytemir K,Yorgun H,et al. The role of preprocedual monocyteto-high-density lipoprotein ratio in prediction of atrial fibrillation recurrence after cryoballoon-based catheter ablation[J]. Europace,2015,17 (12):1807-15.
本文编辑:姚雪莉
Correlation between monocyte-high-density lipoprotein ratio and major adverse cardiovascular events in patients with STEMI undergone emergency PCI
Yu Yongfu*, Wang Lanfeng.
*Department of Cardiovascular Diseases, First Affiliated Hospital of Harbin Medical University, Harbin 150001, China.
Corresponding author: Wang Lanfeng, E-mail: 1014377650@qq.com
Objective To discuss the relationship between monocyte-high-density lipoprotein ratio (MHR) and in-hospital major adverse cardiovascular events (MACE) in patients with ST-segment elevation myocardial infarction (STEMI) undergone emergency percutaneous coronary intervention (PCI). Methods STEMI patients undergone emergency PCI (n=286, male 193, female 93 and aged from 40 to 80) were chosen from the CCU of the First Affiliated Hospital of Harbin Medical University from Oct. 2015 to June 2016. All patients were divided, according to onset of MACAE within one week after hospitalization, into MACE group (n=131) and non-MACE group (n=155). The levels of total cholesterol (TC), triglyceride (TG), high-density lipoprotein-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C), C-reactive protein (CRP), creatine kinase-MB isoenzyme (CK-MB), MHR and left ventricular ejection fraction (LVEF) were detected when patients were hospitalized. Results LVEF decreased, and CK-MB and MHR increased in MACE group compared with non-MACE group (all P<0.05). The results of multi-factor Logistic regression analysis showed that CRP (OR=1.009, 95%CI: 1.001~1.016), LVEF (OR=0.934, 95%CI: 0.905~0.963) and CK-MB (OR=1.003, 95%CI: 1.001~1.004) were influence factors of inhospital MACE in STEMI patients. The increase of MHR was a risk factor of in-hospital MACE in STEMI patients. Conclusion MHR is correlated to MACE in STEMI patients undergone PCI, and the more the MHR is, the higher the risk of MACE is.
Monocyte-high-density lipoprotein ratio; ST-segment elevation myocardial infarction; Major adverse cardiovascular events
R541.4
A
1674-4055(2017)08-0963-03
1150001 哈尔滨,哈尔滨医科大学附属第一医院心血管内科
王岚峰,E-mail:1014377650@qq.com
10.3969/j.issn.1674-4055.2017.08.19