穿刺活检未证实为前列腺癌的血清前列腺特异性抗原阳性的原发部位不明的肿瘤一例报道并文献复习
廖义翔,周家杰,刘 涛,曾金敏,杨光华
·临床诊疗提示·
穿刺活检未证实为前列腺癌的血清前列腺特异性抗原阳性的原发部位不明的肿瘤一例报道并文献复习
廖义翔,周家杰*,刘 涛,曾金敏,杨光华
目的 提高对血清前列腺特异性抗原(PSA)显著升高但穿刺活检未证实为前列腺癌的PSA+的原发部位不明的肿瘤(CUP)的认识。方法 报道荆州市中心医院1例血清PSA显著升高但穿刺活检未证实为前列腺癌的PSA+的CUP的诊疗过程,并进行文献复习。在万方数据知识服务平台及PubMed中检索,时间截至2016-10-09,共8篇文献入选,加上本例患者,共10例血清PSA显著升高但穿刺活检未证实为前列腺癌的PSA+患者被报道,对其进行分析总结。结果 10例男性患者中,年龄61~80岁;直肠指诊均为阴性(前列腺中等大小,质软,未扪及明显结节);血清PSA 56.3~4 222.0 μg/L;均发现骨转移灶或盆腔淋巴结转移灶,经反复前列腺穿刺活检未能证实为前列腺癌,而诊断为PSA+的CUP;均采用姑息性内分泌治疗。结论 血清PSA显著升高,但前列腺穿刺活检结果为阴性的PSA+的CUP患者临床上可考虑采取姑息性内分泌治疗策略,以期延缓患者疾病的进展或缓解患者症状,提高生存质量。
前列腺肿瘤;活组织检查,针吸;前列腺特异抗原;肿瘤,未知原发灶
廖义翔,周家杰,刘涛,等.穿刺活检未证实为前列腺癌的血清前列腺特异性抗原阳性的原发部位不明的肿瘤一例报道并文献复习[J].中国全科医学,2017,20(24):3043-3046.[www.chinagp.net]
LIAO Y X,ZHOU J J,LIU T,et al.Carcinoma of unknown primary origin with markedly elevated PSA levels unconfirmed by repeat prostate biopsy:a case report and review of the literature[J].Chinese General Practice,2017,20(24):3043-3046.
目前血清前列腺特异性抗原(PSA)检测在世界范围内已被广泛作为前列腺癌筛查的金标准[1-3]。由于前列腺炎、前列腺增生、发热、直肠指诊等也可引起血清PSA升高,因此确诊前列腺癌必须经过前列腺穿刺活检。临床工作中偶尔也会出现血清PSA显著升高,但前列腺穿刺活检却未能在组织学上证实为前列腺癌,尤其晚期肿瘤,临床称为PSA+的原发部位不明的肿瘤(carcinoma of unknown primary site,CUP)。本文报道1例血清PSA显著升高,但经过3次前列腺穿刺活检均未能找到组织学证据的转移性前列腺癌病例,并回顾性分析国内外文献资料,复习与血清PSA显著升高相关的CUP。
1 病例简介
患者,男,63岁,因“反复腰背部及四肢疼痛1年”于2015年3月入住荆州市中心医院骨科。患者近1年来无明显诱因反复出现腰背部及四肢疼痛,院外多次自行口服布洛芬缓释胶囊等止痛药物,症状有所好转。既往有高血压病史10年,口服硝苯地平缓释片,控制尚可;无创伤及手术史。体格检查:体温36.3 ℃,脉搏80次/min,呼吸频率20次/min,血压135/85 mm Hg(1 mm Hg=0.133 kPa),消瘦体貌,心肺腑未见明显异常,脊柱多处压痛。入院后实验室检查:血红蛋白86 g/L(参考范围:110~150 g/L),血清PSA 2 136.0 μg/L(参考范围:<4.0 μg/L),血清碱性磷酸酶238 μ/L(参考范围:40~150 μ/L)。MRI提示成骨性骨转移瘤可能。追问病史,患者平常有排尿不畅病史,无血尿及尿痛病史。转科后CT提示纵隔、腹主动脉及髂血管旁淋巴结转移(见图1);全身骨扫描提示多发骨转移(见图2);MRI未提示前列腺癌可能。直肠指诊提示前列腺4.0 cm×3.0 cm×3.5 cm,质软,未扪及明显结节。由于血清PSA显著升高,给予经直肠前列腺穿刺活检,穿刺10针均为阴性。成骨性骨转移瘤合并有显著的血清PSA升高,提示转移性PSA+肿瘤,推荐使用激素相关的内分泌治疗[4]。临床未发现组织学证据证实为前列腺癌,但是患者疼痛症状明显,且血清PSA显著升高,认为治疗疾病的临床优先级应该高于组织学证据,因此诊断为“前列腺癌(TxN1M1)”,给予黄体生成素释放激素类似物去势+非类固醇类抗雄激素治疗,并加用唑来膦酸治疗骨转移,5%葡萄糖注射液100 ml+唑来膦酸4 mg静脉滴注,1次/月,共3个月。为获得病理组织学证据,分别在3个月后和6个月后再次行前列腺穿刺活检,仍然未能获得前列腺癌的组织学证据。由于患者在治疗后3个月腰痛症状明显缓解,而且血清PSA下降至7 μg/L,拒绝行经尿道前列腺电切术(TURP)取活检的建议,要求继续去势+抗雄激素治疗,10个月后患者发展为难治性激素抵抗性前列腺癌(CRPC),血清PSA开始反弹,进行性增加,经多西他赛化疗,患者最终在诊断后24个月死亡,患者家属拒绝尸检,直至最后仍然未找到病理组织学证据。

图2 全身骨扫描提示多发骨转移
Figure 2 Multiple bone metastases assessed by whole-body bone scanning
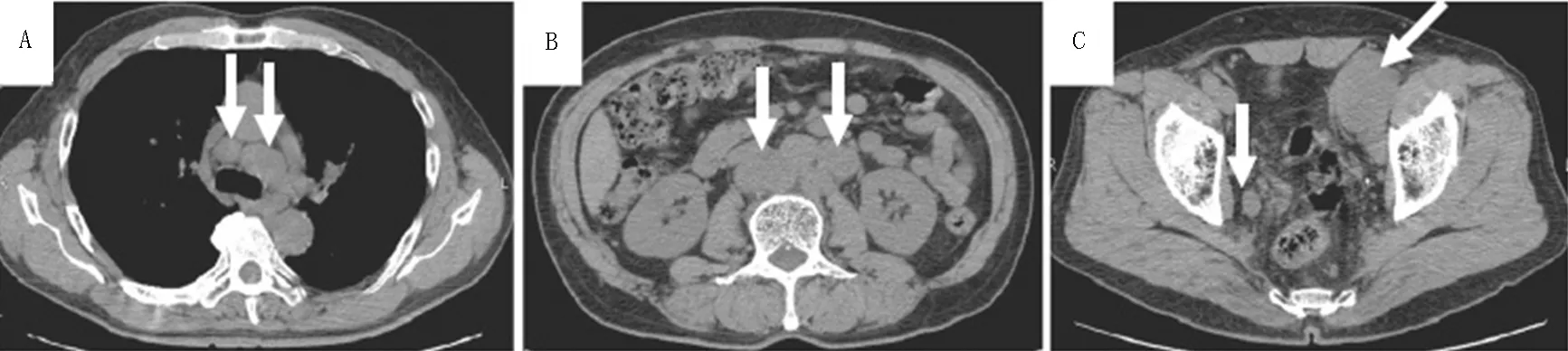
注:A为纵隔,B为腹主动脉,C为髂血管旁
图1 CT提示纵隔、腹主动脉及髂血管旁淋巴结转移
Figure 1 Mediastinal lymph node metastasis,abdominal para-aortic lymph node metastasis,and metastasis to the lymph nodes around the iliac vessels assessed by CT
2 文献复习
2.1 资料来源 以“(前列腺癌)OR(未知原发部位的肿瘤)AND(前列腺穿刺)”为检索词检索万方数据知识服务平台,未发现符合条件的文献。以“prostate cancer”OR“carcinoma of unknown primary site”AND“prostate biopsy”为检索词检索PubMed,时间截至2016-10-09,共检索2 992篇文献,经阅读摘要后剔除与本研究目的无关以及重复发表的文献后,最后纳入8篇文献[5-12],加上本例患者,共10例穿刺活检未证实为前列腺癌的PSA+的CUP患者。
2.2 基本特征 9例患者年龄61~80岁,平均71.4岁;直肠指诊均为阴性(前列腺中等大小,质软,未扪及明显结节);血清PSA 56.3~4 222.0 μg/L,平均855.2 μg/L;7例发现骨转移灶或盆腔淋巴结转移灶,经反复前列腺穿刺活检未能证实为前列腺癌,而诊断为PSA+的CUP;采用姑息性内分泌治疗,平均生存期13个月(见表1)。

表1 9例患者血清PSA和前列腺穿刺活检结果
注:-为未进行检查;PSA=前列腺特异性抗原,TURP=经尿道前列腺电切术
3 讨论
CUP是一种不常见的恶性肿瘤[13],其特点是确切的影像学证据提示转移性肿瘤,但是经过多项检查,如CT、MRI甚至正电子发射计算机断层显像(PET-CT)等高端精密设备检查或者免疫组化、电子显微镜或分子生物学检查、穿刺活检等,始终无法找到原发病灶的证据,是一种通过转移而诊断的绝症[14]。CUP占肿瘤3%~5%[4],恶性程度高,被认为是第7或第8常见恶性肿瘤类型,其肿瘤相关病死率位列第4[15],预后极差。一项Meta分析纳入12篇尸检文献,结果显示:884例患者中644例尸检证实了原发肿瘤部位,其中多见部位为肺部(27%)、胰腺(24%)、肝脏或胆管(8%)、肾脏和肾上腺(8%)、结肠和直肠(7%)、生殖道(7%)和胃(6%)[16]。而以骨转移为主要表现的CUP中,尸检确认前列腺为原发部位位居第2。有文献综述表明,与泌尿系统相关的CUP中,尸检确认原发部位为前列腺癌的发生率约为4%[17]。
CUP不易被发现的主要原因目前尚不十分清楚,主要假设包括自然退化、免疫介导的消亡和先天的微小肿瘤[13,18-19]。一般的CT平扫+增强或MRI常难以发现病灶,因此PET-CT被推荐用作CUP的诊疗。HAN等[20]在120例CUP患者中应用PET-CT进行全身检测,成功找出原发肿瘤部位54例,检出率为42.5%,灵敏度、特异度和准确率分别达91.5%、85.2%和88.3%。
临床上对于CUP的处理策略一般有两种,一是“shotgun modality”,译为“精准模式”,是指通过多种方式务求找到原发病灶,然后进行治疗,精准打击;二是“nihilistic modality”,译为“模糊模式”,是指针对转移灶进行姑息性对症治疗。这是两种截然相反的治疗策略,当通过多种检查均未找到原发病灶时,同时考虑到CUP患者的总生存期非常差,中位生存时间为6~14个月[20],临床只能采取中间策略,采用相对经济实惠的姑息性治疗方式,以期延缓患者疾病的进展或缓解症状,提高生存质量。
本研究患者,成骨性骨转移瘤合并显著的血清PSA升高,提示转移性PSA+肿瘤,通过多方面检查未能发现原发病灶,反复穿刺活检均未得到有力的组织学证据。但是患者疼痛症状明显,且PSA为参考范围的500倍以上,临床认为治疗疾病的优先级应该高于组织学证据,因此诊断患者为“前列腺癌(TxN1M1)”,推荐使用激素相关的内分泌治疗[4]。患者在接受黄体生成素释放激素类似物去势+非类固醇类抗雄激素治疗以及唑来膦酸的治疗后,临床症状得到缓解,且血清PSA明显下降,病情得到控制。遗憾的是10个月后患者发展为难治性CRPC,血清PSA开始反弹,进行性增加,经过多西他赛化疗,最终在诊断后24个月死亡,直至最后仍然未能找到病理组织学证据。搜索PubMed上发表的前列腺穿刺活检结果,提示仅有9例血清PSA明显升高患者,前列腺穿刺活检结果均为阴性[5-12]。尽管血清PSA已被广泛应用于前列腺癌的筛查,但其在结肠、肝、胰腺、肾脏、肾上腺、皮肤、乳腺、卵巢和唾液腺中亦有分泌[20]。因此若反复前列腺穿刺活检阴性,须考虑上述部位恶性肿瘤的可能,因此多种方式、不同时间的反复检查对原发病灶的检出非常有必要。
综上所述,尽管目前大型检查仪器不断进步,但PSA+的CUP的诊断和治疗不论对于医生还是患者均是一个难题,对现代医疗仍是一个挑战。反复的穿刺活检及不同检查方式、不同时间反复检查对CUP的诊断会有一定的帮助,尤其是PET-CT。
作者贡献:廖义翔进行文章的构思与设计、文章的可行性分析、文献/资料收集、文献/资料整理、撰写论文;廖义翔、刘涛、曾金敏、杨光华进行论文修订;周家杰负责文章的质量控制及审校、对文章整体负责,监督管理。
本文无利益冲突。
[1]EGGENER S E,CIFU A S,NABHAN C.Prostate cancer screening[J].JAMA,2015,314(8):825-826.DOI:10.1001/jamaH2015.8033.
[2]BRAWLEY O W,THOMPSON I M Jr,GRÖNBERG H.Evolving recommendations on prostate cancer screening[J].Am Soc Clin Oncol Educ Book,2016,35:e80-87.DOI:10.14694/EDBK_157413.
[3]双卫兵,邓欣.前列腺癌骨转移的治疗[J].现代泌尿生殖肿瘤杂志,2015,7(6):373-377.DOI:10.3870/j.issn.1674-4624.2015.06.018. SHUANG W B,DENG X.Treatment of bone metastases in prostate cancer[J].Journal of Contemporary Urologic and Reproductive Oncology,2015,7(6):373-377.DOI:10.3870/j.issnH1674-4624.2015.06.018.
[4]ETTINGER D S,ARNOLETTI J P,GOCKERMAN J P,et al.Occult primary cancer clinical practice guidelines[J].J Natl Compr Canc Netw,2005,3(2):214-233.
[5]SATO D,MIYASHITA Y,HIMURA I,et al.A suspected case of occult prostatic carcinoma in a patient presenting with gastrointestinal symptoms[J].J Med Soc Toho,1999,46(2):163-168.
[6]NAKATA S,NAKANO K,TAKAHASHI H,et al.A case of prostate cancer diagnosed pathologically by bone metastatic site biopsy[J].Nihon Hinyokika Gakkai Zasshi,2005,96(4):507-510.
[7]UEDA Y,HIGUCHII Y,HASHIMOTO T,et al.Prostate cancer diagnosed through the biopsy of the bone metastatic lesion;a case report[J].Hinyokika Kiyo,2007,53(5):327-330.
[8]WAKATABE Y,OHKUSA H,TABATA K,et al.Two cases of prostate cancer patients with a multifocal bone tumor it was difficult to diagnose in spite of elevated PSA[J].J Kanagawa Med Assoc,2009,36:202-203.
[9]MAKINO T,KUROKAWA K,NEGISHI I,et al.A case of prostate cancer diagnosed by bone biopsy of metastasis lesion[J].Nippon Hinyokika Gakkai Zasshi,2009,100:417-420.
[10]SHIN T K Y,OBINATA D,TAKATAMA K,et al.A case of prostatic cancer which we can diagnosed by the ureteral metastatic carcinoma[J].Japan J Urol Surg,2011,24:65-68.
[11]FUKUMOTO R,SODA T,UEHARA M,et al.A case of prostate cancer diagnosed by lymphadenectomy[J].Hinyokika Kiyo,2012,58(10):557-560.
[12]IWAMURA H,HATAKEYAMA S,TANAKA Y,et al.A case of metastatic cancer with markedly elevated PSA level that was not detected by repeat prostate biopsy[J].BMC Research Notes,2014,7:64-68.DOI:10.1186/1756-0500-7-64.
[13]PAVLIDIS N,PENTHEROUDAKIS G.Cancer of unknown primary site:20 questions to be answered[J].Ann Oncol,2010,21(Suppl 7):vii303-307.DOI:10.1093/annonc/mdq278.
[14]HEMMINKI K,SUNDQUIST K,SUNDQUIST J,et al.Location of metastases in cancer of unknown primary are not random and signal familial clustering[J].Sci Rep,2016,6:22891.DOI:10.1038/srep22891.
[15]ECONOMOPOULOU P,PENTHEROUDAKIS G.Cancer of unknown primary:time to put the pieces of the puzzle together?[J].Lancet Oncol,2016,17(10):1339-1340.DOI:10.1016/S1470-2045(16)30377-1.
[16]PENTHEROUDAKIS G,GOLFINOPOULOS V,PAVLIDIS N.Switching benchmarks in cancer of unknown primary:from autopsy to microarray[J].Eur J Cancer,2007,43(14):2026-2036.DOI:10.1016/j.ejca.2007.06.023.
[17]ALBERTI C.Carcinoma of unknown primary(CUP);some considerations about pathogenesis and diagnostic strategy,particularly focusing on CUPS pertaining to the Urology[J].G Chir,2012,33(1/2):41-46.
[18]RUHLMANN V,RUHLMANN M,BELLENDORF A,et al.Hybrid imaging for detection of carcinoma of unknown primary:a preliminary comparison trial of whole-body PET/MRI versus PET/CT[J].Eur J Radiol,2016,85(11):1941-1947.DOI:10.1016/j.ejrad.2016.08.020.
[19]CRAWFORD S M,SKINNER J,COOMBES E,et al.Cancer of unknown primary:a cancer registry study of factors affecting access to diagnosis[J].Clin Oncol(R Coll Radiol),2017,29(1):e39-46.DOI:10.1016/j.clon.2016.09.011.
[20]HAN A,XUE J,HU M,et al.Clinical value of18F-FDG PET-CT in detecting primary tumor for patients with carcinoma of unknown primary[J].Cancer Epidemiol,2012,36(5):470-475.DOI:10.1016/j.canep.2012.03.002.
(本文编辑:贾萌萌)
Carcinoma of Unknown Primary Origin with Markedly Elevated PSA Levels Unconfirmed by Repeat Prostate Biopsy:a Case Report and Review of the Literature
LIAOYi-xiang,ZHOUJia-jie*,LIUTao,ZENGJin-min,YANGGuang-hua
DepartmentofUrology,JingzhouCentralHospital;theSecondClinicalMedicalCollege,YangtzeUniversity;JingzhouHospital,TongjiMedicalCollege,HuazhongUniversityofScienceandTechnology,Jingzhou434020,China*Correspondingauthor:ZHOUJia-jie,Chiefphysician;E-mail:871315639@qq.com
Objective To improve the awareness level of the cancer of unknown primary origin (CUP) with markedly elevated PSA levels unconfirmed by repeat prostate biopsy.Methods We reported the diagnosis and treatment of one case of CUP with markedly elevated PSA levels but was not confirmed by repeat prostate biopsy form Jingzhou Central Hospital,and reviewed the corresponding literature.We searched and included 8 articles in which totaled 9 such patients were reported from Wanfang data and PubMed as of 2016-10-09.We analyzed and summarized the clinical data of the above 9 cases and one case
by Jingzhou Central Hospital.Results The data of the 10 cases:male aged 61-80;negative results of digital rectal examination (the prostate was soft,medium-sized without obvious nodules );serum PSA levels were 56.3-4 222.0 μg/L;bone metastases or pelvic lymph node metastases were found;negative results of repeat prostate biopsy;diagnostic result was CUP with markedly elevated PSA levels;therapeutic regimen was palliative endocrine therapy.Conclusion For patients with CUP,markedly elevated PSA levels and negative results of repeat prostate biopsy,palliative endocrine therapy is suggested to use in order to delay the progress of the disease or relieve the symptoms and improve the quality of life.
Prostatic neoplasms;Biopsy,aspiration;Prostate-specific antigen;Neoplasms,unknown primary origin
R 737.25
D
10.3969/j.issn.1007-9572.2017.06.y52
2016-11-11;
2017-04-06)
434020湖北省荆州市,荆州市中心医院 长江大学第二临床医学院 华中科技大学同济医学院附属荆州医院泌尿外科
*通信作者:周家杰,主任医师;E-mail:871315639@qq.com

