Wiltse 入路与后正中入路 TLIF 手术治疗腰椎间盘突出症的比较研究
黄晓川 林斌 刘晖 周亮 何永志 黄砖枝
Wiltse 入路与后正中入路 TLIF 手术治疗腰椎间盘突出症的比较研究
黄晓川 林斌 刘晖 周亮 何永志 黄砖枝
目的探讨 Wiltse 入路与后正中入路 TLIF 手术治疗腰椎间盘突出症临床疗效及术后相邻节段退变是否存在差异。方法2014 年 6 月至 2015 年 6 月,我科对 100 例腰椎间盘突出症患者采用 TLIF 手术治疗,按入院顺序编号利用 SPSS 软件随机采用 Wiltse 入路和后正中手术入路两种方法进行。90 例获随访,其中 Wiltse 入路 46 例,后正中入路 44 例。比较两组术前、术后 1 天肌酸激酶值 ( creatine kinase,CK ),术前、术后 3 个月及终末随访的疼痛视觉模拟评分 ( visual analogue scale,VAS ) 和 Oswestry 功能障碍指数( oswestry disability index,ODI ),术前、终末随访多裂肌脂肪浸润评分和融合节段相邻上位椎间盘修正 MRI指数。结果所有患者均无定位错误、神经损伤、脑脊液漏、椎间隙感染等严重并发症,随访时间 11~23 个月,平均 ( 15.8±3.7 ) 个月,Wiltse 入路组术前、术后 1 天 CK 分别为 ( 83.84±24.79 ) U / L,( 164.26± 23.74 ) U / L;后正中手术入路组术前、术后 1 天 CK 分别为 ( 79.93±23.50 ) U / L,( 419.27±40.94 ) U / L。Wiltse 入路组术前、术后 3 个月和终末随访 VAS 评分分别为 ( 7.00±1.23 ) 分,( 1.52±0.67 ) 分,( 1.48± 0.51 ) 分;后正中手术入路组术前、术后 3 个月和终末随访 VAS 评分分别为 ( 7.27±1.24 ) 分,( 2.09± 0.61 ) 分,( 2.18±0.66 ) 分。Wiltse 入路组术前、术后 3 个月和终末随访 ODI 评分分别为 68.26±8.97,22.78± 4.30,22.96±3.95;后正中手术入路组术前、术后 3 个月和终末随访 ODI 评分分别为 69.18±9.83,27.55± 2.82,27.82±3.54。Wiltse 入路组术前、终末随访多裂肌脂肪浸润评分分别为 ( 1.26±0.45 ) 分,( 1.35± 0.57 ) 分;后正中手术入路术前、终末随访多裂肌脂肪浸润评分分别为 ( 1.36±0.49 ) 分,( 2.05±0.58 ) 分;Wiltse 入路组术前、终末随访融合节段相邻上位椎间盘修正 MRI 指数分别为 69.98±16.68,68.85±12.38;后正中手术入路术前、终末随访融合节段相邻上位椎间盘修正 MRI 指数分别为 67.98±14.84,55.19±11.99。两组术前 CK、VAS、ODI、多裂肌脂肪浸润评分、融合节段相邻上位椎间盘修正 MRI 指数的差异无统计学意义,两组术后 1 天 CK、术后 3 个月 VAS、终末随访 VAS、术后 3 个月 ODI、终末随访 ODI、终末随访多裂肌脂肪浸润评分、终末访融合节段相邻上位椎间盘修正 MRI 指数差异有统计学意义。Wiltse 手入路组在术后疼痛、疗效、多裂肌损伤和融合节段相邻上位椎间盘退变情况比后正中入路组具有优势。结论 在腰椎间盘突出患者行 TLIF 手术的治疗过程中,Wiltse 手术入路比后正中入路具有优势,延缓融合相邻节段退变,提高患者的生活质量。
椎间盘移位;腰椎;最小侵入性外科手术;相邻节段退变
随着老龄化社会的到来,腰椎退变性疾病成为影响人们生活质量的常见病,腰椎后路减压、椎间植骨融合内固定是治疗腰椎间盘突出症的重要手术方式。经椎间孔腰椎椎体间融合术 ( transforaminal lumbar interbody fusion,TLIF ) 可以通过后正中和经 Wiltse 肌间隙两种入路进行。后正中入路将椎旁肌剥离,常导致术后下腰痛的发生,Wiltse 入路从椎旁肌肌间隙进入,不损伤椎旁肌,降低腰椎融合术后下腰痛发生率,是腰椎微创手术入路[1]。TLIF手术椎间融合率高,但国内外文献报道腰椎融合术后导致相邻节段退变[2]。目前,越来越多的学者关注腰椎融合术后相邻节段退变,近年来,笔者采用Wiltse 入路结合 Quandrant 微创通道行 TLIF 手术治疗腰椎间盘突出症取得良好疗效。对 2014 年 6 月至2015 年 6 月,我院收治的 90 例腰椎间盘突出症患者进行前瞻性对比研究,明确 Wiltse 入路和正中入路的 TLIF 手术在治疗腰椎间盘突出症的疗效和术后相邻节段的退变方面的差异。报告如下。
资料与方法
一、纳入与排除标准
1. 纳入标准:( 1 ) 单节段腰椎间盘突出症伴有不稳;( 2 ) 经正规保守治疗半年疗效不佳;( 3 ) 患者知晓并签署知情同意书。
2. 排除标准:( 1 ) 多节段椎间盘突出症;( 2 ) 腰椎滑脱;( 3 ) 腰椎先天性发育异常;( 4 ) 患者不同意纳入此项研究。
二、一般资料
本组共纳入 100 例,行 TLIF 手术治疗,按入院顺序编号利用 SPSS 软件随机采用 Wiltse 入路和后正中入路两种方法治疗,每组各 50 例。90 例获随访,其中 Wiltse 入路 46 例,后正中入路 44 例,随访时间 11~23 个月,平均 ( 15.8±3.7 ) 个月;Wiltse入路组男 32 例,女 14 例,年龄 43~68 岁,平均( 55.9±7.9 ) 岁;后正中入路组男 29 例,女 15 例,平均年龄 41~65 岁,平均 ( 54.1±6.7 ) 岁 ( 表1 )。
三、手术方法
Wiltse 入路组:全身麻醉,俯卧位,常规消毒,根据术前 MRI 多裂肌弧形最凸点到棘突正中线距离测量,并结合术前在 C 型臂机前后位透视下,标记手术节段椎弓根位置,采用 Wiltse 手术切口,棘突正中旁双侧长约 3 cm 的 2 个纵向切口。切开皮肤、皮下组织及腰背筋膜后,将导管从多裂肌与最长肌肌间隙插入,直至骨性结构,逐级扩张导管,选择合适深度的 Quadrant 通道页片,连接固定至自由臂,撑开叶片,并连接光源。钻出椎弓根钉置钉通道,插入导针,定位透视满意,拔出导针,骨蜡封闭针眼,症状重一侧行开窗减压,切除椎间盘,放置椎间融合器,按原先置钉通道置入椎弓根螺钉,透视椎弓根钉位置良好,装上连接杆固定。以同样方式在症状轻一侧安放连接通道,不减压,置入连接椎弓根钉,冲洗后双侧切口,放置引流管,逐层闭合切口。
后正中入路组:传统后正中入路手术,症状重一侧行开窗减压。
四、观察内容及评价指标
( 1 ) 术前、术后 1 天肌酸激酶 ( creatine kinase,CK ) 值;( 2 ) 术前、术后 3 个月和终末随访疼痛视觉模拟评分 ( visual analogue scale,VAS );( 3 ) 术前、术后 3 个月和终末随访 Oswestry 功能障碍指数( oswestry disability index,ODI );( 4 ) 术前和终末随访 MRI 多裂肌内脂肪浸润评分,根据欧阳林等[3]报道,将多裂肌内脂肪浸润分为 3 度:I 度,肌内不显示脂肪信号或单个线状、点状脂肪信号;II 度,肌内显示多发灶性脂肪信号 ( 超过 2 处,但没有形成网格状或羽毛状 );III 度,肌内显示网格状或羽毛状脂肪信号。I 度为 1 分,II 度为 2 分,III 度为3 分;( 5 ) 采用 Sobajima 等[4]报道的方法进行融合节段相邻上位椎间盘信号测量,在影像 PACS 系统勾勒出髓核区域的轮廓线,即能显示其信号强度( signal intensity,SI ) 和面积,计算两者的乘积为MRI 指数。选取同节段脑脊液信号值作为参照值,以消除因磁场场强不均造成的偏差,修正 MRI 指数=髓核 SI×面积÷脑脊液 SI,如图 1 所示。
五、统计学处理
采用 SPSS 17.0 软件进行统计学分析,采用 χ2检验比较两组性别,采用 t 检验比较两组年龄,术前、术后及随访各观察内容数据,P<0.05 为差异有统计学意义。
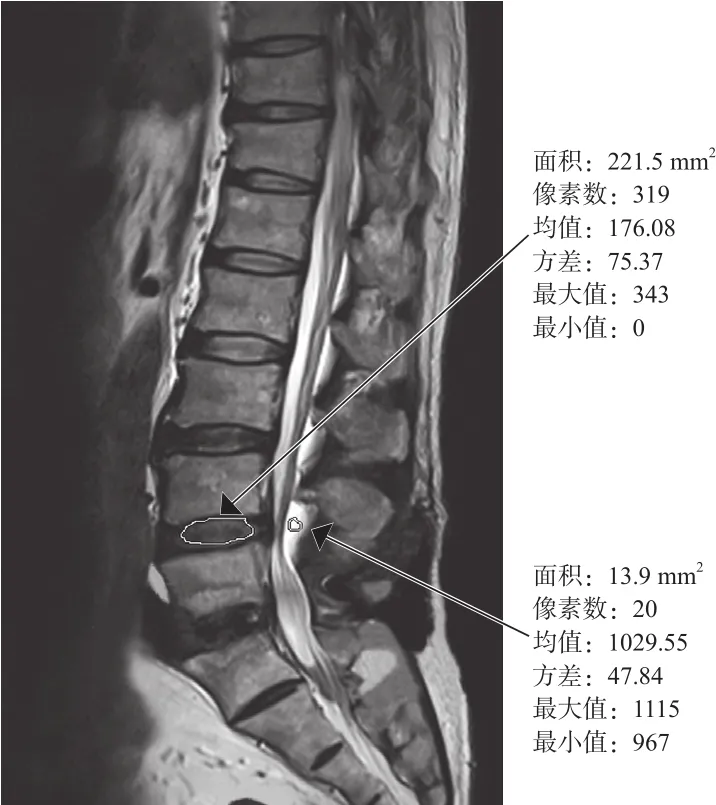
图1 修正 MRI 指数的测量Fig.1 The measurement of modifed MRI index
结 果
所有患者均无定位错误、神经损伤、脑脊液漏、椎间隙感染等严重并发症,Wiltse 入路组随访时间 11~23 个月,平均 ( 16.1±3.9 ) 个月,后正中入路组随访时间 11~23 个月,平均 ( 15.5±3.6 ) 个月。术前两组 CK、VAS、ODI、术前多裂肌脂肪浸润评分、术前融合节段相邻上位椎间盘修正 MRI 指数差异无统计学意义 ( P>0.05 );两组术后 1 天 CK、术后 3 个月和终末随访 VAS、术后 3 个月和终末随访ODI、终末随访多裂肌脂肪浸润评分、终末随访融合节段相邻上位椎间盘修正 MRI 指数的差异有统计学意义 ( P<0.05 ),Wiltse 入路组在术后疼痛、疗效、多裂肌损伤情况 ( 图 2 ) 和融合节段相邻上位椎间盘退变情况比后正中入路组具有优势 ( 表1 )。
讨 论
腰椎多裂肌主要维持脊柱稳定性,Rosatelli 等[5]报道腰椎多裂肌除了 L5包含浅、深 2 层,其余的均包含浅、中、深 3 层。浅层起于腰椎各个棘突,向外下走行,跨过多个节段止于 L5、S1的乳突以及骶骨、髂骨。中层起于腰椎各个棘突,L1、L2、L3分别止于 L4、L5及 S1的乳突,L4中层多裂肌止于 S2背面。深层起源于腰椎各个椎板,跨过 2 个节段后分别止于下 2 个节段的乳突。由于中层多裂肌较薄,和浅层均起于棘突,跨越节段长,浅、中层结构和功能极其相似,因此有学者并不把多裂肌中层独立分出,而把腰椎的多裂肌分为浅、深 2 层[6]。
传统腰椎后正中入路广泛剥离椎旁肌特别是多裂肌,导致其损伤,常导致腰椎术后下腰痛[7]。1968 年,Wiltse 等[8]报道腰椎多裂肌与最长肌之间肌间隙手术入路,该入路对多裂肌干扰极小,降低腰椎术后下腰痛发生率[9]。本研究术后 3 个月及终末随访的 VAS 评分和 ODI 评分 Wiltse 入路组明显低于后正中入路组。

图2 两组术前、终访 MRI 中多裂肌脂肪浸润评分 a:Wiltse 入路术前 MRI 提示多裂肌脂肪浸润为 2 分;b:Wiltse 入路术后 18 个月终访 MRI 提示多裂肌脂肪浸润为 2 分;c:后正中入路术前 MRI 提示多裂肌脂肪浸润为 1 分;d:后正中入路术后 18 个月多裂肌脂肪浸润为 2 分Fig.2 The fatty infltration score of the multifdus muscle in MRI between the 2 groups preoperatively and at the fnal follow up a: Preoperatively the fatty infltration score of the multifdus muscle was 2 in Wiltse approach; b: At 18 months after the operation the fatty infltration score of the multifdus muscle was 2 in Wiltse approach; c: Preoperatively the fatty infltration score of the multifdus muscle was 1 in posterior midline approach; d: At 18 months after the operation the fatty infltration score of the multifdus muscle was 2 in posterior midline approach
表1 Wiltse 入路组与后正中入路组各项指标的比较 (±s)Tab.1 The comparison of indexs between Wiltse approach group and posterior midline approach group (±s)
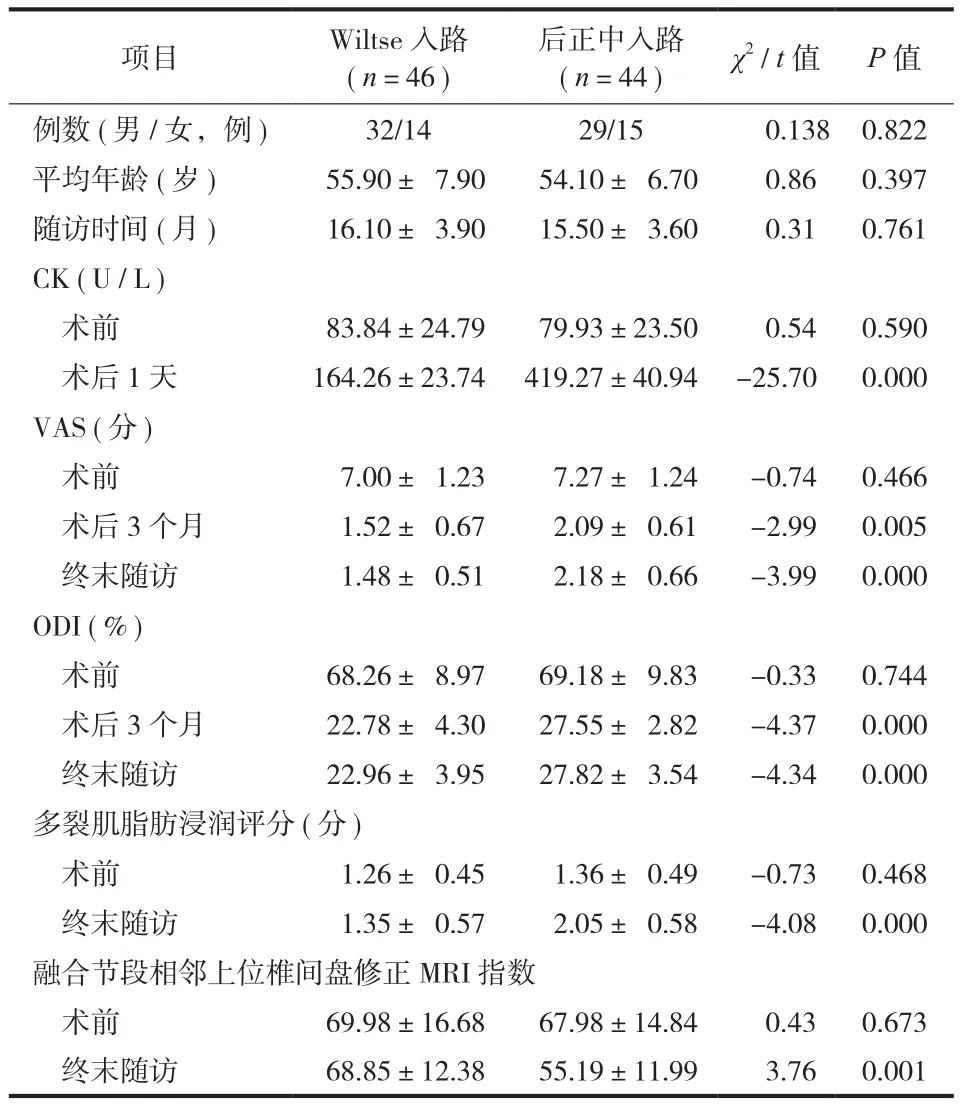
表1 Wiltse 入路组与后正中入路组各项指标的比较 (±s)Tab.1 The comparison of indexs between Wiltse approach group and posterior midline approach group (±s)
项目 Wiltse 入路( n=46 )后正中入路( n=44 ) χ2/ t 值 P 值例数 ( 男 / 女,例 ) 32/14 29/15 0.138 0.822平均年龄 ( 岁 ) 55.90± 7.90 54.10± 6.70 0.86 0.397随访时间 ( 月 ) 16.10± 3.90 15.50± 3.60 0.31 0.761 CK ( U / L )术前 83.84±24.79 79.93±23.50 0.54 0.590术后 1 天 164.26±23.74 419.27±40.94 -25.70 0.000 VAS ( 分 )术前 7.00± 1.23 7.27± 1.24 -0.74 0.466术后 3 个月 1.52± 0.67 2.09± 0.61 -2.99 0.005终末随访 1.48± 0.51 2.18± 0.66 -3.99 0.000 ODI ( % )术前 68.26± 8.97 69.18± 9.83 -0.33 0.744术后 3 个月 22.78± 4.30 27.55± 2.82 -4.37 0.000终末随访 22.96± 3.95 27.82± 3.54 -4.34 0.000多裂肌脂肪浸润评分 ( 分 )术前 1.26± 0.45 1.36± 0.49 -0.73 0.468终末随访 1.35± 0.57 2.05± 0.58 -4.08 0.000融合节段相邻上位椎间盘修正 MRI 指数术前 69.98±16.68 67.98±14.84 0.43 0.673终末随访 68.85±12.38 55.19±11.99 3.76 0.001
肌酸激酶有 3 种同工酶,主要存在于骨骼肌、脑和心肌中。存在骨骼肌的肌酸激酶同工酶的升高主要与肌肉的损伤过程相关,一般术后第 1 天最高,术后 1 周基本恢复正常[10]。Kawaguchi 等[11]报道,腰椎传统后路手术后肌酸激酶明显高于前路手术,其认为后路比前路对肌肉损伤更为严重,可能是由于后路手术广泛剥离椎旁肌导致损伤。由于血浆中骨骼肌同工酶含量占 96% 以上,因此,在对脑及心肌无影响手术中可以用肌酸激酶值反映骨骼肌的损伤情况。本研究术后 1 天 CK 值 Wiltse 入路组明显低于后正中入路组,提示 Wiltse 入路组对于椎旁肌损伤低于后正中入路组;终访 MRI 多裂肌脂肪浸润评分 Wiltse 入路组明显低于后正中入路组,进一步证实 Wiltse 入路组对于椎旁肌损伤低于后正中入路组;结合术后 VAS 评分及 ODI 评分 Wiltse 入路组明显低于后正中入路组,证明多裂肌在维持腰椎稳定起着重要作用,降低术后下腰痛的发生率。
Ozgur 等[12]首次报道腰椎融合术后相邻节段退变,这引起脊柱外科医生广泛关注。随着对脊柱研究的不断深入,有些学者认为,腰椎融合术后相邻节段应力增加,小关节负荷增加,椎间盘压力增大,以上因素加速相邻节段退变[13]。学者对腰椎退变常常采用椎间隙高度下降、小关节关节炎等定性指标或半定量指标进行评价,这些指标并不能反映腰椎早期退变情况[14]。如何才能早期反映腰椎退变成为学者关注问题。椎间盘退变早期变化为髓核含水量下降,Benneker 等[15]研究表明,椎间盘 T2加权像上的信号强度和其内部含水量相关,即可通过 T2加权像上的信号强度来反映椎间盘退变早期变化。Sobajima 等[4]报道,MRI 指数 ( 即椎间盘髓核的信号强度与面积乘积 ) 与退变腰椎间盘组织学检查相符,其反映了椎间盘早期退变。本研究通过PACS 影像数据系统选取同节段脑脊液信号值作为参照值,以消除因磁场场强不均造成的偏差。本研究终末随访融合节段相邻上位椎间盘修正 MRI 指数 Wiltse 入路组明显高于后正中入路组,考虑多裂肌延迟腰椎融合术后相邻节段退变。后正中入路造成多裂肌的损伤,导致腰椎稳定性的下降,随后带来的生物力学变化加速退变,使术后下腰痛发生率增加。
本研究表明,对于腰椎间盘突出症的 TLIF 手术治疗,Wiltse 入路与后正中入路相比,具有减小椎旁肌损伤、临床疗效好、较好延缓融合相邻节段退变等特点。由于本研究病例数较少,随访时间较短,有待于进一步大样本、多中心及长期随访研究,进一步证实 Wiltse 入路 TLIF 手术治疗腰椎间盘突出症的优势。
[1] Wiltse LL, Spencer CW. New uses and refinements of the paraspinal approach to the lumbar spine[J]. J Spine, 1988, 13(6):696-706.
[2] Zencica P, Chaloupka R, Hladíková J, et al. Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis:a retrospective radiological and clinical analysis[J]. J Acta Chir Orthop Traumatol Cech, 2010, 77(2):124-130.
[3] 欧阳林, 何平, 肖玉辉, 等. 磁共振成像对腰肌劳损的诊断价值[J]. 中国临床医师杂志, 2011, 5(4):92-96.
[4] Sobajima S, Kompel JF, Kim JS, et al. A slowly progressive and reproducible animal model of intervetebral disc degeneration characterized by MRI, X-ray, and histology[J]. J Spine, 2005, 30(1):15-24.
[5] Rosatelli AL, Ravichandiran K, Agur AM. Three-dimensional study of the musculotendinous architecture of lumbar multifdus and its functional implications[J]. J Clin Anat, 2008, 21(6): 539-546.
[6] Hoh DJ, Wang MY, Ritland SL. Anatomic features of the paramedian muscle-splitting approaches to the lumbar spine[J]. Neurosurgery, 2010, 66(3):13-25.
[7] Schwender JD, Holly LT, Rouben DP, et al.Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results[J]. J Spinal Disord Tech, 2005, 18(Suppl 2):S1-6.
[8] Wiltse LL, Bateman JG, Hutchinson RH, et a1. The paraspinal sacrospinalis-splitting approach to the lumbar spine[J]. J Bone Joint Surg (Am), 1968, 50(5):919-926.
[9] Kuriyama N, Ito H. Electromyographic functional analysis of the lumbar spinal muscles with low back pain[J]. J Nippon Med Sch, 2005, 72(3):165-173.
[10] 胡志军, 范顺武, 赵兴, 等. 微创后路腰椎椎体间融合术椎旁软组织解剖评估[J]. 国际骨科学杂志, 2007, 28(5):295-297.
[11] Kawaguchi Y, Matsui H, Tsuji H. Changes in serum creatine phosphokinase MM isoenzyme after lumbar spine surgery[J]. J Spine, 1997, 22(9):1018-1023.
[12] Ozgur BM, Yoo K, Rodriguez G, et al. Minimally invasive technique for transforaminal lumbar interbody fusion[J]. J Eur Spine, 2005, 14(9):887-894.
[13] Hee HT, Castro FP, Majd ME, et al. Anterior/posterior lumbar fusion versus transforaminal lumbar interbody fusion: analysis of complications and predictive factors[J]. J Spinal Disord, 2001, 14(6):533-540.
[14] GhiselliG, Wang JC, Hsu WK, et al. L5S1segment survivorship and clinical outcome analysis after L4-5 isolated fusion[J]. J Spine, 2003, 28(15):1275-1280.
[15] Benneker LM, Heini PF, Anderson SE, et al. Correlation of radiographic and MRI parameters to morphological and biochemical assessment of intervertebral disc degeneration[J]. J Eur Spine, 2005, 14(1):27-35.
( 本文编辑:王萌 )
A comparative study of transforaminal lumbar interbody fusion between Wiltse approach and posterior midline approach in the treatment of lumbar disc herniation
HUANG Xiao-chuan, LIN Bin, LIU Hui, ZHOU Liang,HE Yong-zhi, HUANG Zhuan-zhi. Center of Orthopaedics, the 175th Hospital of Chinese PLA, Zhangzhou, Fujian, 363000, China
ObjectiveTo investigate the clinical effects and the differences of adjacent segment degeneration between Wiltse approach and posterior midline approach in the treatment of lumbar disc herniation by transforaminal lumbar interbody fusion ( TLIF ).MethodsA total of 100 patients with lumbar disc herniation were treated with TLIF between June 2014 and June 2015. Each patient had a serial number according to admission order and were treated by Wiltse approach or posterior midline approach at random by the SPSS software. Ninety patients were followed up, including 46 patients treated by Wiltse approach and 44 patients treated by posterior midline approach. The 2 groups were compared in creatine kinase ( CK ) value, visual analogue scale ( VAS ) score, Oswestry disability index( ODI ) score, fatty infltration score of the multifdus muscle and modifed MRI index of the upper adjacent segment preoperatively, postoperatively and at the fnal follow-up.ResultsAll the patients had no positioning errors, nerve injury, cerebrospinal fuid leak, disc space infection or other serious complications. The average time of follow-up was ( 15.8 ± 3.7 ) months ( range: 11 - 23 months ). The CK values preoperatively and at 1 day after the operation were ( 83.84 ± 24.79 ) U / L and ( 164.26 ± 23.74 ) U / L respectively in Wiltse approach group, which were ( 79.93 ± 23.50 ) U / L and ( 419.27 ± 40.94 ) U / L respectively in posterior midline approach group. The VAS scores preoperatively, at 3 months after the operation and at the fnal follow-up were 7.00 ± 1.23, 1.52 ± 0.67 and 1.48 ± 0.51 respectively in Wiltse approach group, which were 7.27 ± 1.24, 2.09 ± 0.61 and 2.18 ± 0.66 in posterior midline approach group. The ODI scores preoperatively, at 3 months after the operation and at the fnal follow-up were 68.26 ± 8.97, 22.78 ± 4.30 and 22.96 ± 3.95 respectively in Wiltse approach group, which were 69.18 ± 9.83, 27.55 ± 2.82 and 27.82 ± 3.54 respectively in posterior midline approach group. The fatty infltration scores of the multifdus muscle preoperatively and at the fnal follow-up were 1.26 ± 0.45 and 1.35 ± 0.57 respectively in Wiltse approach group, which were 1.36 ± 0.49 and 2.05 ± 0.58 respectively in posterior midline approach group. The modifed MRI index of the upper adjacent segment preoperatively and at the fnal follow-up were 69.98 ± 16.68 and 68.85 ± 12.38 respectively in Wiltse approach group, which were 67.98 ± 14.84 and 55.19 ± 11.99 respectively in posterior midline approach group. No statistically significant differences were found between the 2 groups in CK value, VAS, ODI, fatty infiltration score of the multifdus muscle and modifed MRI index of the upper adjacent segment preoperatively, but there were statistically signifcant differences between the 2 groups in CK value at 1 day after the operation, VAS and ODI at 3 months after the operation and at the fnal follow-up and fatty infltration score of the multifdus muscle and modifed MRI index of the upper adjacent segment at the fnal follow-up. Wiltse approach was superior to posterior midline approach in postoperative pain, curative effects, multifidus muscle injury and degeneration of the upper adjacent segment.ConclusionsCompared with posterior midline approach, the treatment of lumbar disc herniation by TLIF through Wiltse approach has more advantages, which can delay adjacent segment degeneration and promote the quality of patients’ life.
Intervertebral disc displacement; Lumbar vertebrae; Minimally invasive surgical procedures; Adjacent segment degeneration
10.3969/j.issn.2095-252X.2017.01.008
R681.5, R687.3
漳州市自然科学基金 ( ZZ2014J33 )
363000 漳州,中国人民解放军第 175 医院 ( 厦门大学附属东南医院 ) 全军骨科中心
2016-08-12 )