幽门螺杆菌感染对植入药物洗脱支架急性冠状动脉综合征患者长期预后的影响
王德昭 王 军 李世敬 陈步星*
(1. 首都医科大学附属北京天坛医院心内科, 北京 100050; 北京市门头沟区医院心内科, 北京 102300)
· 心血管疾病的病理生理机制 ·
幽门螺杆菌感染对植入药物洗脱支架急性冠状动脉综合征患者长期预后的影响
王德昭1王 军2李世敬2陈步星1*
(1. 首都医科大学附属北京天坛医院心内科, 北京 100050; 北京市门头沟区医院心内科, 北京 102300)
目的 探讨幽门螺杆菌(Helicobacterpylori, Hp)感染和急性冠状动脉综合征(acute coronary syndrome, ACS)患者植入药物洗脱支架(drug eluting stent, DES)后长期随访心血管不良事件的关系。方法 回顾性选择2010年1月1日至2012年12月31日行DES植入术的326例ACS患者。所有患者均已经进行了13C尿素呼气试验,高敏C反应蛋白(high sensitive C-reactive protein, hsCRP),同型半胱氨酸(homocysteine, HCY)等检查,根据Hp感染情况及是否行Hp根除治疗分为3组:无Hp感染的患者组(Hp- group,n=176),Hp阳性行根治术后转阴患者(Hp+therapy group,n=75),Hp阳性没有根除治疗患者(Hp+no therapy group,n=75)。随访5年内主要心血管不良事件(main adverse cardiovascular event, MACE)和上消化道出血(upper gastrointestinal bleeding, UGIB)发生情况。结果 随访5年,结果发现Hp+no therapy患者较其他2组MACE和UGIB发生率高(P值分别为0.009和0.000)。Hp+no therapy是预测累积MACE事件(HR:2.441, 95%CI:1.354~4.400,P=0.003)和UGIB(HR:5.257, 95%CI:2.572~10.745,P<0.001)的独立危险因素。结论 植入药物洗脱支架合并Hp感染的ACS患者有更多的MACE和UGIB发生, Hp根除治疗可以降低MACE和UGIB的发生率。
幽门螺杆菌;根除治疗; 急性冠状动脉综合征;主要不良心脏事件;远期预后
幽门螺杆菌(Helicobacterpylori, Hp)感染被认为是许多疾病的致病因素,是导致消化不良的常见原因,与食管运动失调、胃食管反流病以及消化性溃疡相关的消化道出血(upper gastrointestinal bleeding, UGIB)关系密切[1-3]。随着越来越多的急性冠状动脉综合征(acute coronary syndrome, ACS)患者使用药物洗脱支架(drug eluting stent, DES),需要进行长期双联抗血小板治疗的患者也越来越多,随之而来,在这些患者中UGIB的发生率也逐年增高。双联抗血小板药物治疗患者UGIB发生率为12.5%,而非双联抗血小板药物治疗的患者上消化道出血发生率为4.0%[4-5]。许多ACS患者在接受双联抗血小板治疗同时也伴随Hp感染,这些都大大增加了UGIB的发生率。
Hp感染可能在冠状动脉粥样硬化性心脏病(coronary artery disease, CAD)发病中发挥某种潜在的作用[6]。有研究[7]表明,血清学阳性的Hp感染与ACS的发生和动脉粥样硬化的进展呈显著正相关。中国2013年消化科指南建议,服用双联抗血小板药物的患者,如果没有消化性溃疡,不需要Hp根除治疗,而日本和韩国的指南则建议采取根除治疗[8]。这些患者是否应该采取根除治疗是有争议的。
本研究目的是探讨Hp感染与服用双联抗血小板治疗的ACS患者长期预后之间的关系,并评价Hp根除疗法对于主要心血管事件(major adverse cardiac events, MACE)和UGIB的意义。
1 材料与方法
1.1 研究对象
本研究入选自2010年1月1日至2012年12月31日在北京市门头沟区医院连续住院的ACS患者。图1是试验的流程图,有365例患者入组,所有患者均签署了知情同意书,并通过北京市门头沟区医院伦理委员会同意。排除7例非药物涂层支架和6例失访患者外,随访期结束后有326例患者资料齐全。记录患者的病史﹑体格检查和实验室检查结果。入选患者分为3组。第1组:Hp阴性组(Hp,n=176),第2组:Hp阳性并进行根除Hp治疗组(Hp+治疗,n=75),和第3组:Hp阳性未根除Hp治疗组(Hp +无治疗,n=75)。Hp阳性组利用数字表法随机决定是否进行根除治疗。

图1 入组患者随访流程图
Fig.1 Flow chart of the patients enrolled into the trial
Hp:Helicobacterpylori; DES: drug eluting stent.
1.2 入选标准
根据2012年欧洲心脏病学会(European Society of Cardiology,ESC)指南[9],入选的ACS患者由不稳定型心绞痛,非ST段抬高心肌梗死和ST段抬高心肌梗死(ST segment elevation myocardial infarction,STEMI)组成。所有患者服用双联抗血小板治疗,住院期间植入药物洗脱支架后,没有消化系统症状及体征。
1.3 排除标准
曾在1月内有胃肠道出血者,有胃切除术、心功能不全、甲状腺功能异常病史,任何部位的现症感染。在1个月内使用抗生素、质子泵抑制剂、H2受体拮抗剂、铋剂或硫糖铝。住院期间未行DES植入术也被排除在外。有反酸、烧心、恶心、呕吐、胃痛、腹泻或已明确存在Hp感染而致的消化性溃疡患者被排除。
1.4 方法
1.4.1 常规检查
所有患者入院后第二天进行下面的检查,受试者抽血化验前至少空腹2 h:血常规、糖化血红蛋白、血清高敏C反应蛋白(high sensitive C-reactive protein, hs-CRP)、血清同型半胱氨酸(homocysteine, HCY)、凝血4项。
1.4.213C尿素呼气试验
13C尿素呼气试验使用HCBT-01呼气试验自动化测试仪(深圳中核海德威生物科技有限公司)。Hp感染由13C/12C同位素比值确定(δ‰)。Hp感染被定义为δ≥(4±0.4)‰[10]。
1.4.3 超声心动图检查
采用GE VIVID超声心动图诊断系统(美国GE公司)进行超声心动图检查。患者被要求在左侧卧位。在胸骨旁长轴、胸骨旁短轴、心尖四腔心切面和心尖两腔图中使用。左室舒张末期内径和左心房内径均采用胸骨旁长轴切面测量。双侧辛普森公式用来量化左室射血分数(left ventricular eject fraction, LVEF)。
1.4.4 冠状动脉血管造影术(coronary angiography, CAG)和经皮冠状动脉介入治疗(percutaneous coronary intervention, PCI)
所有的急性心肌梗死患者接受再灌注治疗为直接PCI。所有患者不稳定型心绞痛患者进行择期PCI。术前签署知情同意书后,立即给予负荷剂量阿司匹林(300 mg)和氯吡格雷(300 mg)服用。抗凝给予普通肝素(100 IU / kg),活化部分凝血活酶时间≥60 s。血栓抽吸、球囊血管成形术和支架植入术采用标准技术。
1.5 Hp根除疗法
根除治疗组给予为期10 d的雷贝拉唑(20 mg,每天2次)、阿莫西林(1 g,每日2次)和左氧氟沙星(250 mg,每天2次)治疗。Hp根除治疗后30 d再进行13C尿素呼气试验为阴性。
1.6 随访
所有患者出院后门诊随访5年。出院后1个月在心内科门诊进行随访,此后每6个月进行随访。监测MACE事件(包括非致死性心梗,非致死性靶血管血运重建以及全因死亡)[11]和UGIB。所有患者完成数据采集后,进行数据录入和分析。
1.7 统计学方法
连续变量采用t检验,非连续变量采用χ2检验。当连续数据不呈正态分布,组间比较采用非参数Wilcoxon秩和检验。采用Kaplan-Meier比较3组间的MACE发生率和UGIB发生率。使用Cox比例风险回归模型对MACE和UGIB的影响因素先进行单因素分析,P<0.1的变量进入多因素回归分析。以P<0.05为差异有统计学意义。
2 结果
2.1 3组患者基线资料比较
3组患者hsCRP和HCY水平比较差异有统计学意义(P<0.001),其余变量差异无统计学意义(表1)。
2.2 Cox回归分析结果
Cox单因素分析显示,Hp+无治疗、年龄和多支病变与MACE事件的发生有关,Cox多因素回归分析显示,Hp+无治疗(RR:2.441,95%CI:1.354~4.400,P=0.003)、年龄(RR:1.022,95%CI:1.001~1.043,P=0.038)、多支病变(RR:1.781,95%CI:1.011~3.138,P=0.046)和HsCRP(RR:0.964,95%CI:0.932~0.997,P=0.035)是MACE事件发生的预测因子(表2)。
Cox单因素分析显示,Hp+无治疗和年龄与UGIB事件的发生有关,Cox多因素回归分析显示,Hp+无治疗(RR:5.257,95%CI:2.572~10.745,P<0.001)、年龄(RR:1.037,95%CI:1.011~1.063,P=0.004)、糖尿病(RR:0.287,95%CI:0.112~0.735,P=0.009)和HsCRP(RR:0.940,95%CI:0.893~0.989,P=0.017)是UGIB事件发生的预测因子(表3)。
表1 3组患者基线资料
Tab.1 Baseline data of the three groups
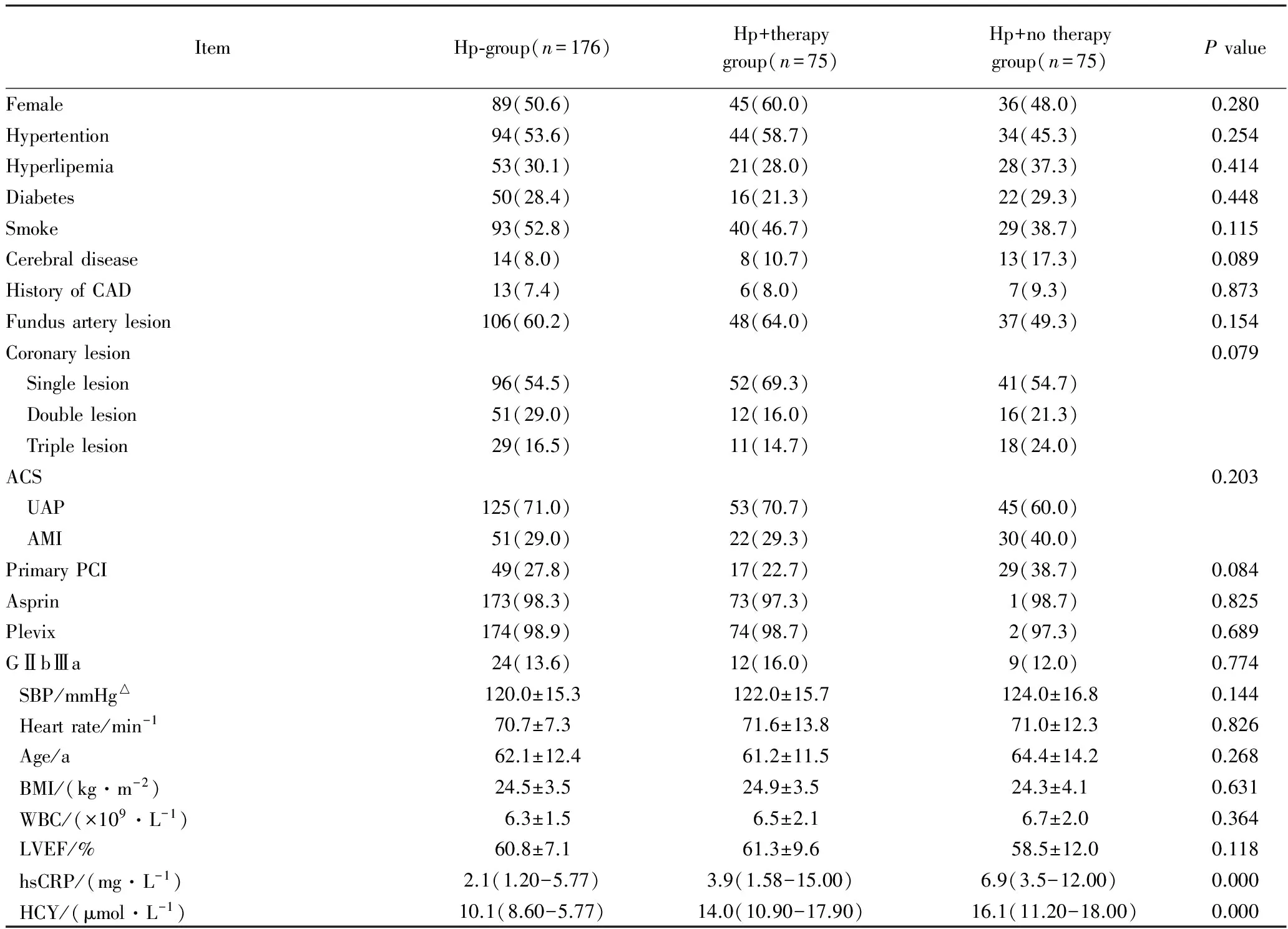
ItemHp⁃group(n=176)Hp+therapygroup(n=75)Hp+notherapygroup(n=75)PvalueFemale89(50.6)45(60.0)36(48.0)0.280Hypertention94(53.6)44(58.7)34(45.3)0.254Hyperlipemia53(30.1)21(28.0)28(37.3)0.414Diabetes50(28.4)16(21.3)22(29.3)0.448Smoke93(52.8)40(46.7)29(38.7)0.115Cerebraldisease14(8.0)8(10.7)13(17.3)0.089HistoryofCAD13(7.4)6(8.0)7(9.3)0.873Fundusarterylesion106(60.2)48(64.0)37(49.3)0.154Coronarylesion0.079 Singlelesion96(54.5)52(69.3)41(54.7) Doublelesion51(29.0)12(16.0)16(21.3) Triplelesion29(16.5)11(14.7)18(24.0)ACS0.203 UAP125(71.0)53(70.7)45(60.0) AMI51(29.0)22(29.3)30(40.0)PrimaryPCI49(27.8)17(22.7)29(38.7)0.084Asprin173(98.3)73(97.3)1(98.7)0.825Plevix174(98.9)74(98.7)2(97.3)0.689GⅡbⅢa24(13.6)12(16.0)9(12.0)0.774SBP/mmHg△120.0±15.3122.0±15.7124.0±16.80.144Heartrate/min-170.7±7.371.6±13.871.0±12.30.826Age/a62.1±12.461.2±11.564.4±14.20.268BMI/(kg·m-2)24.5±3.524.9±3.524.3±4.10.631WBC/(×109·L-1)6.3±1.56.5±2.16.7±2.00.364LVEF/%60.8±7.161.3±9.658.5±12.00.118hsCRP/(mg·L-1)2.1(1.20-5.77)3.9(1.58-15.00)6.9(3.5-12.00)0.000HCY/(μmol·L-1)10.1(8.60-5.77)14.0(10.90-17.90)16.1(11.20-18.00)0.000
△1mmHg=0.133kPa;Hp:Helicobacterpylori;CAD: coronary artery disease; ACS: acute coronary syndrome; UAP: unstable angina pectoris; AMI: acute myocardial infarction; PCI:percutaneous coronary intervention; SBP: systolic blood pressure; BMI: body mass index; WBC: white blood-cell count; LVEF: left ventricular ejection fraction; hsCRP: high sensitive C-reactive protein; HCY: homocysteine.
表2 Cox回归分析MACE的影响因素(进入法)
Tab.2 Predictors of presence of MACE in Cox proportional hazards regression model (enter)
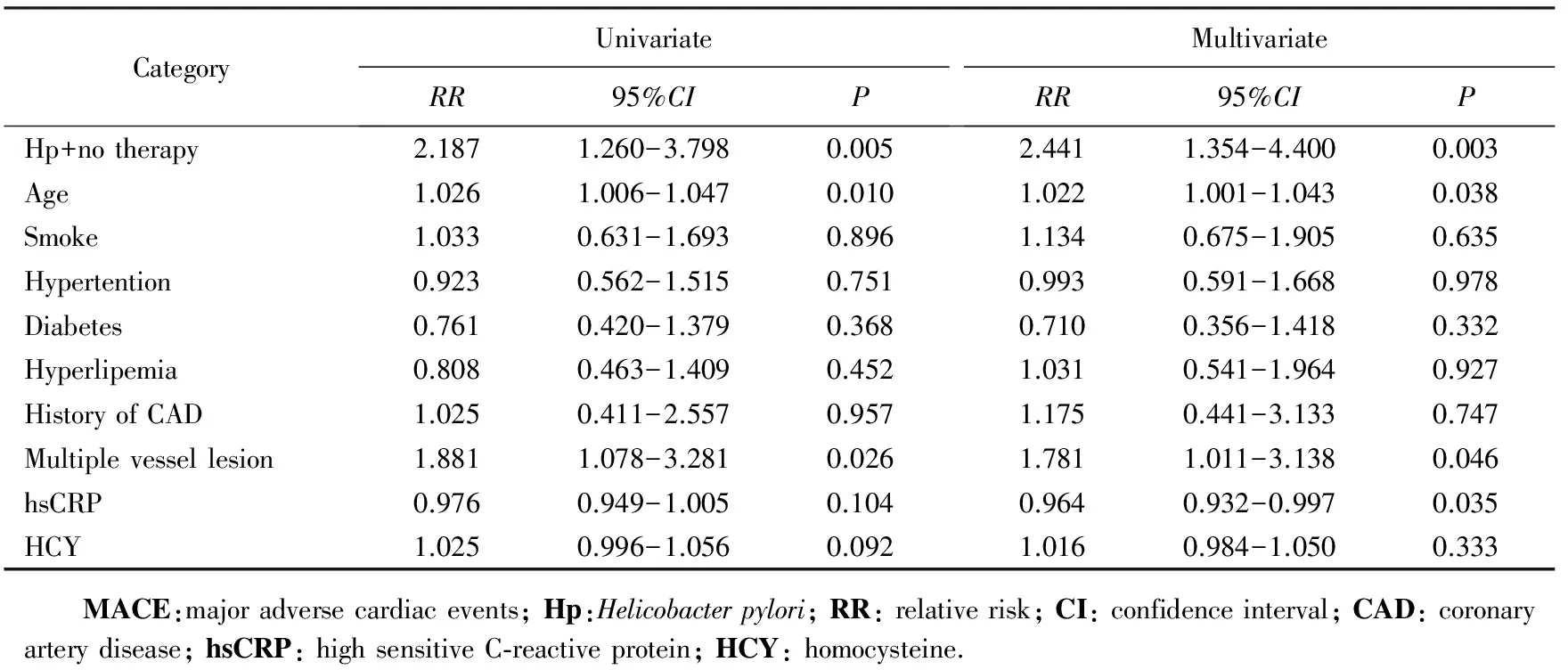
CategoryUnivariateRR95%CIPMultivariateRR95%CIPHp+notherapy2.1871.260-3.7980.0052.4411.354-4.4000.003Age1.0261.006-1.0470.0101.0221.001-1.0430.038Smoke1.0330.631-1.6930.8961.1340.675-1.9050.635Hypertention0.9230.562-1.5150.7510.9930.591-1.6680.978Diabetes0.7610.420-1.3790.3680.7100.356-1.4180.332Hyperlipemia0.8080.463-1.4090.4521.0310.541-1.9640.927HistoryofCAD1.0250.411-2.5570.9571.1750.441-3.1330.747Multiplevessellesion1.8811.078-3.2810.0261.7811.011-3.1380.046hsCRP0.9760.949-1.0050.1040.9640.932-0.9970.035HCY1.0250.996-1.0560.0921.0160.984-1.0500.333 MACE:majoradversecardiacevents;Hp:Helicobacterpylori;RR:relativerisk;CI:confidenceinterval;CAD:coronaryarterydisease;hsCRP:highsensitiveC⁃reactiveprotein;HCY:homocysteine.
表3 Cox回归分析上消化道出血的影响因素(进入法)
Tab.3 Predictors of presence of UGIB in Cox proportional hazards regression model (enter)
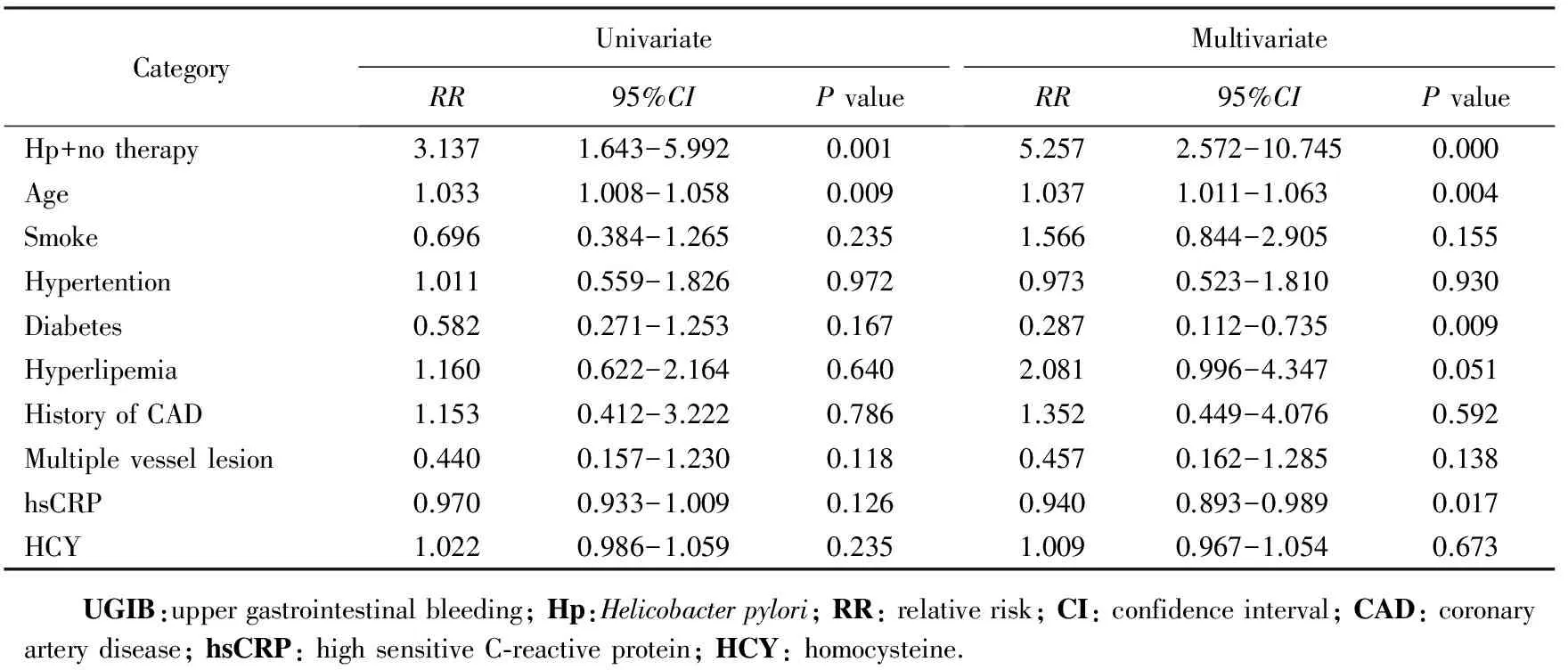
CategoryUnivariateRR95%CIPvalueMultivariateRR95%CIPvalueHp+notherapy3.1371.643-5.9920.0015.2572.572-10.7450.000Age1.0331.008-1.0580.0091.0371.011-1.0630.004Smoke0.6960.384-1.2650.2351.5660.844-2.9050.155Hypertention1.0110.559-1.8260.9720.9730.523-1.8100.930Diabetes0.5820.271-1.2530.1670.2870.112-0.7350.009Hyperlipemia1.1600.622-2.1640.6402.0810.996-4.3470.051HistoryofCAD1.1530.412-3.2220.7861.3520.449-4.0760.592Multiplevessellesion0.4400.157-1.2300.1180.4570.162-1.2850.138hsCRP0.9700.933-1.0090.1260.9400.893-0.9890.017HCY1.0220.986-1.0590.2351.0090.967-1.0540.673 UGIB:uppergastrointestinalbleeding;Hp:Helicobacterpylori;RR:relativerisk;CI:confidenceinterval;CAD:coronaryarterydisease;hsCRP:highsensitiveC⁃reactiveprotein;HCY:homocysteine.
2.3 比较3组 MACE和UGIB的发生率
随访60个月,3组患者MACE 的发生率分别为15.9%,16.0%和30.7%,差异有统计学意义(Log rank testF=9.462,P=0.009),详见图2。3组UGIB 的发生率分别为9.7%,9.3%和26.7%,差异有统计学意义(Log rank testF=16.188,P<0.001),详见 图3。
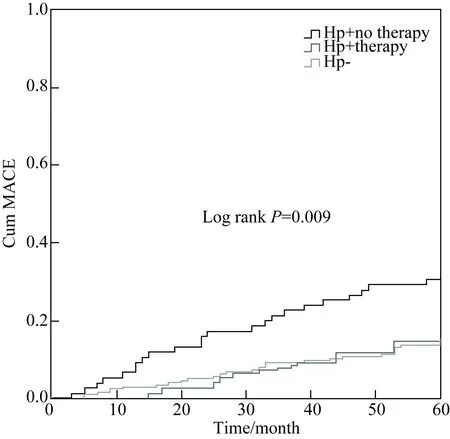
图2 3组患者累积MACE事件的Kaplan Meier曲线
Fig.2 Kaplan-Meier curves of MACE among three groups
MACE:main adverse cardiovascular event; Hp:Helicobacterpylori.
3 讨论
Hp是一种强制性的细胞内病原体,可导致持久性感染,在某些患者中可能终生存在,并可以产生永久的抗体[3]。有研究[12-13]报道Hp阳性和心脏X综合征的患者有较大相关性,Hp感染与ACS之间亦关系密切[7,14],但是也有研究[15-17]显示二者并无明确相关性。本研究评估了326例行DES植入的ACS患者未来5年内Hp感染与MACE和UGIB的关系,结果发现Hp感染是预测MACE和UGIB的独立危险因素。Hp阳性未根除治疗的患者相对风险是Hp阴性组的2.441倍。Hp阳性患者如果给予根除Hp治疗则与Hp阴性的患者的MACE和UGIB发生率差异无统计学意义,这也从侧面证实Hp根除治疗可以降低MACE和UGIB的发生率。
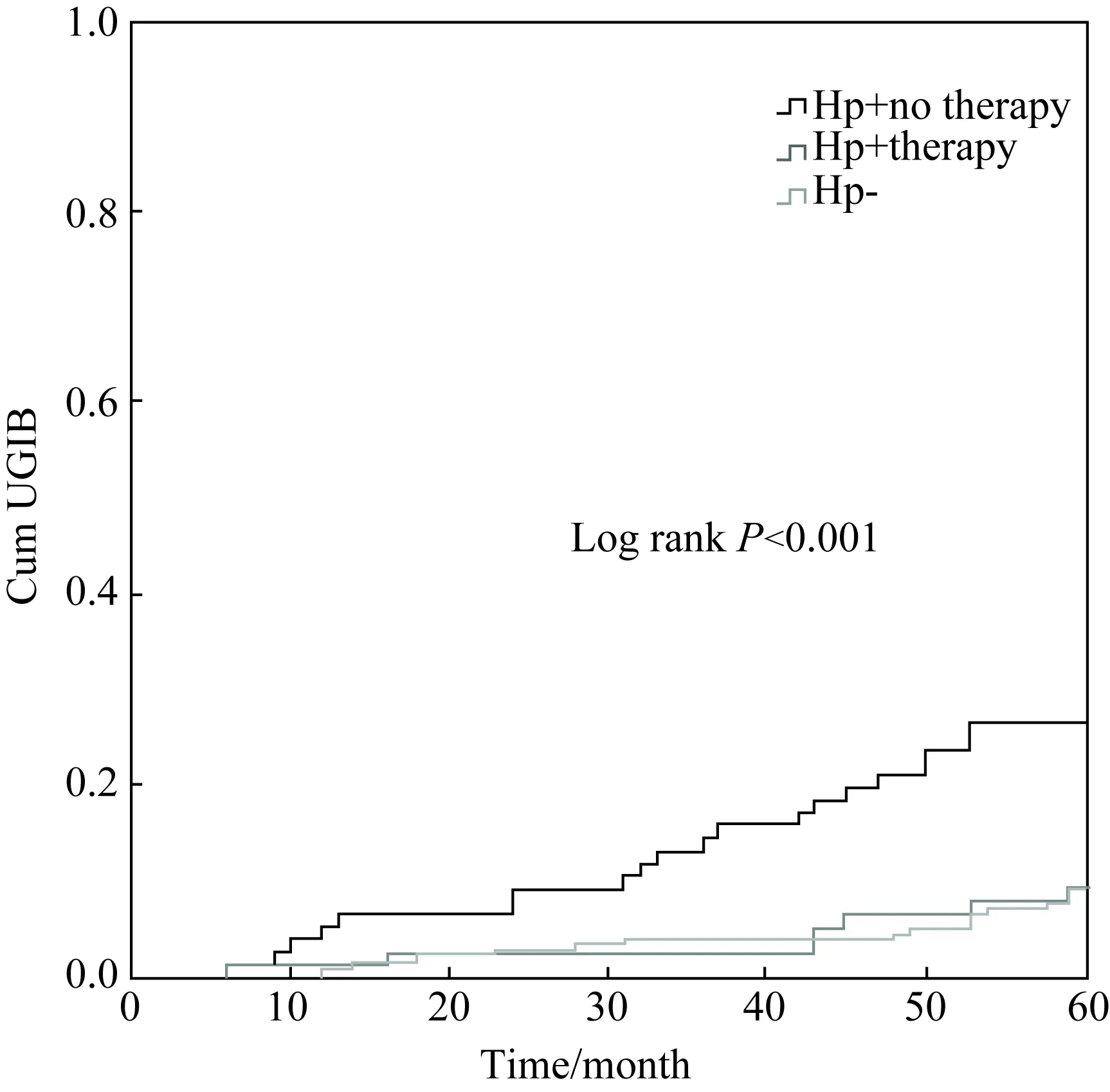
图3 3组患者UGIB事件的Kaplan Meier曲线
Fig.3 Comparison of Kaplan-Meier curves as a function of time to the UGIB among three groups
UGIB:upper gastrointestinal bleeding; Hp:Helicobacterpylori.
研究[18-19]指出Hp感染对动脉粥样硬化有促进作用:首先,Hp感染启动一种急性期反应,并激活肿瘤坏死因子-1、白细胞介素-6和纤维蛋白原,这些炎性细胞因子可以直接或间接地参与动脉壁的炎性反应。其次,Hp也可以导致血小板聚集,并通过引起内皮损伤来激活自身免疫反应[20-21],由于抗原模仿,细菌和热休克蛋白之间产生交叉免疫反应[22],这个过程可能导致冠状动脉钙化和动脉粥样硬化[23]。此外,Hp可以直接定植于动脉血管壁[18],有研究者[24]利用聚合酶链反应技术在动脉粥样斑块处发现了Hp。在ACS和斑块破裂的急性期,Hp可能导致局部炎性反应,加重血小板聚集,导致急性心肌缺血的发生[22],这可以解释Hp感染与长期不良事件相关。
以往对于Hp感染与未来心血管不良事件发生率之间关系是有争议的,这种差异可能是由于研究人群不同所致。例如,有研究[18]入选的是健康成年人,而还有研究[25]则入选了冠状动脉粥样硬化性心脏病患者。此外,以前的研究[26]只是检测Hp IgG和IgA抗体,二者对评估Hp感染的敏感性和特异性均较差。本研究采用13C尿素呼气试验检测是否存在Hp感染,该检测技术是目前国内外认可的金标准[26-27]。在本研究中,传统的心血管危险因素包括高血压、糖尿病、高脂血症、吸烟、家族史和MACE的发生率无显著相关,可能是因为本研究入选的患者均为ACS患者,绝大多数患者均存在若干上述危险因素,而且在随访期间对上述传统危险因素已给予了积极的治疗。另外,也可能存在选择偏倚、单中心研究和样本量偏小的问题,尚期待大规模的随机对照研究。
综上,本研究表明,在植入DES的ACS患者中,Hp感染患者在长期随访中有更多的MACE和UGIB发生,Hp根除治疗可以降低MACE和UGIB的发生率。
[1] Budzyński J, Kopocka M, Bujak R, et al. Autonomic nervousfunction in Helicobacter pylori-infected patients with atypical chest pain studied by analysis of heart rate variability[J]. Eur J Gastroenterol Hepatol, 2004,16(5): 451-457.
[2] Fashner J,Gitu A C. Common gastrointestinal symtoms: dyspepsia and Helicobacter pylori[J]. FP Essent, 2013,413(10): 24-28.
[3] Roesler B M, Rabelo-Gonçalves E M, Zeitune J M.Virulence factors of Helicobacter pylori: a review[J].Clin Med Insights Gastroenterol, 2014,7(3): 9-17.
[4] Ng F H, Wong S Y, Chang C M, et al. Gastrointestinal bleeding in patients receiving a combination of aspirin, clopidogrel, and enoxaparin in acute coronary syndrome[J]. Am J Gastroenterol, 2008, 103(4): 865-871.
[5] Huang K W, Luo J C, Huang C C, et al. Risk factors for upper gastrointestinal bleeding in coronary artery disease patients receiving both aspirin and clopidogrel[J]. J Chin Med Assoc, 2013,76(1):9-14.
[6] Rogha M, Nikvarz M, Pourmoghaddas Z, et al. Is Helicobacter pylori infection a risk factor for coronary heart disease? [J]. ARYA Atheroscler,2012,8(1):5-8.
[7] Vafaeimanesh J, Hejazi S F, Damanpak V, et al. Association of Helicobacter pylori infection with coronary artery disease: is Helicobacter pylori a risk factor?[J].Scientific World Journal,2014,2014:516354.
[8] Lee S Y.Current progress toward eradicating Helicobacter pylori in East Asian countries:differences in the 2013 revised guidelines between China, Japan, and South Korea[J].World J Gastroenterol,2014,20(6):1493-1502.
[9] Hamm C W, Bassand J P, Agewall S, et al. ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the task force for the management of aute coronary syndromes (ACS) in patients presenting without persistent ST-segement elevation of the European Society of Cardiology (ESC) [J]. Eur Heart J,2011,32(23): 2999-3054.
[10]邸岩, 高炳霞, 齐颖, 等. 门诊患者13C-呼气试验检测幽门螺杆菌的调查分析[J]. 中华医院感染学杂志, 2013, 23(24): 5960-5962.
[11]Cutlip D E, Windecker S, Mehran R, et al. Clincal end points in coronary stent trials: a case for standardized definitions[J]. Circulation,2007,115(17): 2344-2351.
[12]Celik T, Iyisoy A, Yuksel U C. Possible pathogenetic role of Helicobacter pylori infection in cardiac syndrome X[J]. Int J Cardiol,2010,142(2):193-194.
[13]Assadi M, Saghari M, Ebrahimi A, et al. The relation between Helicobacter pylori infection and cardiac syndrome X: apreliminary study[J].Int J Cardiol,2009,134(3):e124-e125.
[14]Franceschi F, Niccoli G, Ferrante G, et al. CagA antigen of Helicobacter pylori and coronary instability: insight from aclinico-pathological study and a meta-analysis of 4241 cases[J]. Atherosclerosis, 2009,202(2):535-542.
[15]Ozdogru I, Kalay N, Dogan A, et al. The relationship between Helicobacter pylori IgG titre and coronary atherosclerosis[J]. Acta Cardiol, 2007,62(5):501-505.
[16]Saleh N, Svane B, Jensen J, et al. Stent implantation, but not pathogen burden, is associated with plasma C-reactive protein and interleukin-6 levels after percutaneous coronary intervention in patients with stable angina pectoris[J]. Am Heart J, 2005, 149(5):876-882.
[17]Delaney B C, Hobbs F D, Holder R. Association of Helicobacter pylori infection with coronary heart disease. Eradication of the infection on grounds of cardiovascular risk is not supported by current evidence[J]. BMJ,1996,312(7025):251-252.
[18]Sessa R, Pietro M D, Filardo S, et al. Infectious burden and atherosclerosis: a clinical issue[J].World J Clin Cases,2014,2(7):240-249.
[19]Tamer G S, Tengiz I, Ercan E, et al. Helicobacter pylori seropositivity in patients with acute coronary syndromes[J]. Dig Dis Sci,2009, 54(6):1253-1256.
[20]Fagoonee S, De Angelis C, Elia C, et al. Potential link betweenHelicobacter pylori and ischemic heart disease: does the bacterium elicit thrombosis?[J]. Minerva Med,2010,101(2):121-125.
[21]Rechciński T, Kasprzak J D, Chmiela M, et al. Patients with unstable angina pectoris present increased humoral response againstHelicobacter pylori in comparison with patients with aggravated dyspepsia[J]. Acta Microbiol Pol,2002,51(4):339-344.
[22]Strachan D P. Non-gastrointestinal consequences of Helicobacter pylori infection[J]. Br Med Bull,1998,54(1):87-93.
[23]Zhu J, Katz R J, Quyyumi A A, et al. Association of serum antibodies to heat-shock protein 65 with coronary calcification levels: suggestion of pathogen-triggered autoimmunity in early atherosclerosis[J]. Circulation,2004,109(1):36-41.
[24]Izadi M, Fazel M, Sharubandi S H, et al. Helicobacter species in the atherosclerotic plaques of patients with coronaryartery disease[J].Cardiovasc Pathol,2012,21(4):307-311.
[25]Smieja M, Gnarpe J, Lonn E, et al. Multiple infections and subsequent cardiovascular events in the Heart Outcomes Prevention Evaluation (HOPE) Study[J]. Circulation,2003,107(2):251-257.
[26]Eskandarian R, Ghorbani R, Shiyasi M, et al. Prognostic role of Helicobacter pylori infection in acute coronary syndrome: aprospective cohort study[J].Cardiovasc J Afr, 2012,23(3):131-135.
[27]李玲, 姜树强,龙丽娟,等. 健康人群幽门螺杆菌感染情况调查分析[J]. 解放军医药杂志,2013,25(10):98-99.
编辑 孙超渊
Helicobacterpyloriinfection impact on long-term prognosis in patients implanted with drug-eluting stent with acute coronary syndrome
Wang Dezhao1, Wang Jun2, Li Shijing2, Chen Buxing1*
(1.DepartmentofCardiology,BeijingTiantanHospital,CapitalMedicalUniversity,Beijing100050,China; 2.DepartmentofCardiology,BeijingMentougouDistrictHospital,Beijing102300,China)
Objective To explore the relationship betweenHelicobacterpylori(Hp) infection and the long-term outcome in patients with acute coronary syndrome (ACS) treated with drug-eluting stent (DES) implantation. Methods We retrospectively analyzed consecutive 326 patients who were treated with DES implantation from January 1, 2010 to December 31, 2012. Demographic data were collected and all patients underwent examination of high sensitivity C-reactive protein (hsCRP), homocysteine (HCY) and other biochemical indicators. All the patients were divided into three groups according to the result of13C urea breath test. Group 1 had 176 patients without Hp infection; Group 2 had 75 patients with Hp infection with eradication therapy; and group 3, 75 patients with Hp infection without eradication therapy. We explored the correlations of Hp infection with major adverse cardiovascular event (MACE) and upper gastrointestinal bleeding (UGIB) after 5 years of follow-up using survival analysis. Results After 5 years of follow-up, we found that patients with Hp infection without therapy had more MACE and UGIB than the other two groups (Pvalue is 0.009 and 0.000, respectively). Survival analysis showed that Hp infection was a predictor of MACE with a hazard ratio (HR) of 2.441, with 95% confidence interval (CI): 1.354-4.400,P=0.003 and UGIB with HR of 5.257, with 95%CI: 2.572-10.745,P<0.001. Conclusion Patients after DES implantation with Hp infection had more MACE and UGIB after 5 years of follow-up. Hp eradication therapy maybe able to lower the rate of MACE and UGIB.
Helicobacterpylori; eradication therapy; acute coronary syndrome; major adverse cardiac events; long-term outcome
北京市优秀青年基金项目(2011D008017000002)。This study was supported by Outstanding Youth Fund Project the of Beijing(2011D008017000002).
时间:2016-12-15 09∶52
http://www.cnki.net/kcms/detail/11.3662.R.20161215.0952.002.html
10.3969/j.issn.1006-7795.2016.06.006]
R 54
2016-10-03)
*Corresponding author, E-mail:chbux@126.com