肠腔内、外双套管负压引流在低位直肠癌一期切除吻合术中的应用
闫威,李松明,李瑞,张嘉越,岑延增,冷津立,赖彦华,何红艳,羊涛
肠腔内、外双套管负压引流在低位直肠癌一期切除吻合术中的应用
闫威,李松明,李瑞,张嘉越,岑延增,冷津立,赖彦华,何红艳,羊涛△
目的探讨肠腔内、外双套管负压引流在低位直肠癌一期切除吻合中的可行性与安全性。方法回顾性收集2009年1月—2014年12月期间收治的650例低位直肠癌患者资料,分为对照组(n=220)、造口组(n=205)和引流组(n=225)。对照组采用Dixon术(直肠低位前切除术);造口组行Dixon术加预防性末端回肠造口术,二期手术还纳;引流组行Dixon术,术中放置肠腔内、外双套管持续灌洗负压引流。比较3组患者手术时间、术中出血量、术后排气时间、住院费用的差异。术后进行随访,分析3组术后吻合口漏及术后感染等并发症发生情况。结果3组手术时间、术中出血量以及术后排气时间差异无统计学意义(P>0.05);引流组患者住院时间和住院费用低于造口组(P<0.05)。在并发症方面,3组患者的吻合口漏发生率、切口感染、盆、腹腔感染、肺部感染的发生率差异无统计学意义(P>0.05)。术后随访结果显示,3组患者的复发、转移及死亡比例差异均无统计学意义(P>0.05)。结论肠腔内、外双套管负压引流可缩短低位直肠癌患者Dixon术后的住院时间,减轻患者负担,能否降低术后吻合口漏发生率需进一步证实。
直肠肿瘤;吻合术,外科;引流术;手术后并发症;低位直肠癌;Dixon术;双套管引流;吻合口漏
低位直肠癌是我国较为常见的恶性肿瘤,具有患病率高、患病时间早、肿瘤位置低的特点[1]。目前其手术治疗主要采用吻合器辅助下的Dixon术式,但由于直肠特殊的解剖结构,吻合口张力大,血供不足,术后吻合口漏的发生率较高[2]。笔者近年来在行Dixon术时采用了肠腔内、外双套管持续负压吸引的方案,取得较好的临床效果,现总结如下。
1 对象与方法
1.1 研究对象选取2009年1月—2014年12月间我院收治的650例直肠癌患者,按照手术方式分为对照组(220例)、造口组(205例)和引流组(225例)。纳入标准:(1)入院前有便血、便频、便细、黏液便等直肠癌临床症状,影像学检查提示直肠占位。(2)经肠镜取材,病理学检查确诊为直肠癌。(3)接受一期切除吻合手术。排除标准:(1)全身情况差,恶病质状态,不能耐受手术。(2)直肠癌位置距齿状线<5 cm,肿瘤广泛侵袭周围组织,无法完全切除或已发生远处转移。(3)多发结、直肠肿瘤。所有入选的患者及其家属均知情同意并签署知情同意书。3组患者性别、年龄、肿瘤部位、TNM分期、白蛋白、血红蛋白及白细胞计数差异均无统计学意义(P>0.05),见表1。

Tab.1Comparison of the clinical characteristics between three groups表1 3组患者临床特征比较
1.2 手术方法3组患者的手术均由同一专业组医生施行。围手术期治疗:术前均行肠道准备,抗感染和营养支持治疗,控制内科疾病。手术操作:所有病例均按照直肠全系膜切除(TME)原则进行手术,术中吻合一律应用吻合器或切割吻合器。对照组行传统Dixon手术[3]:常规游离结肠系膜,牢固结扎肠系膜下动脉及伴行静脉,分离并切除乙状结肠和直肠,保证切缘距肿瘤>2 cm,且吻合口无张力。一期吻合,放置传统单腔引流管。造口组[4]:Dixon术完成后行末端回肠造口术,一段末端回肠(3~5 cm)提拉至左下腹部皮肤表面,硬质塑料棒穿行于外置回肠下,防止其回缩。术后第2~ 3天切开外置回肠,引流其内容物。外置回肠回纳的时间取决于患者临床状态,如无吻合口漏等术后并发症,多在术后12 d进行。引流组[5]:Dixon术中放置肠腔内、外双套管持续负压引流。肿瘤所在直肠切除并吻合后,于距吻合口近端约10 cm的肠管处做一浆肌层荷包缝合。切开肠管,将自制的双套引流管置入肠腔内,引流管前端跨过吻合口5 cm,收紧荷包线;引流管另一端引出体外,将引流管出肠壁处的浆膜与腹膜缝合固定,此为肠腔内双套管引流,并在吻合口旁置入另一双套引流管,为肠腔外双套管引流,见图1。双套引流管均于手术完成后从腹壁撤出体外,内套管接负压15~30 kPa持续吸引并间断冲洗,外套管接500 mL生理盐水。结肠外双套管的外套管为普通橡皮引流管(内径1.0 cm,长度30~40 cm),内套管为吸痰管(内径0.7 cm、长度35~50 cm);结肠内双套管的外套管为蕈状导尿管,长度30~40 cm,内套管为吸痰管(内径0.5 cm、长度35~50 cm)。双套管内端均剪成鱼口状,距内管末端3~5 cm处剪3~4个侧孔;内套管插入外套管中,距外套管外端约6 cm处穿出,双套管两管内端平齐,将内套管用丝线与外套管在穿出位置缝合固定。根据术中情况,外管在距内端约5~8 cm处剪数个椭圆形侧孔。双套管内、外套管侧孔直径分别约为1 mm和2 mm。

Fig.1An illustration of the double cavity casing negative pressure drainage by inside and outside of the intestine.图1 肠腔内、外双套管引流示例
1.3 疗效评价分别记录3组的手术时间、术中出血量、排气时间、住院时间、住院费用、术后感染情况、吻合口漏发生率等。术后对所有患者进行随访,随访时间为6~48个月,中位随访时间36个月。随访内容主要包括:患者生存状态、生活品质、肿瘤复发情况等。
1.4 统计学方法采用SPSS 19.0进行统计学分析。计量资料以均数±标准差表示,多组间均数比较采用方差分析,组间多重比较采用SNK-q检验;计数资料组间比较采用χ2检验。以P<0.05为差异有统计学意义。
2 结果
2.1 术后疗效比较3组围手术期均无病例死亡。3组间手术时间、术中出血量以及术后排气时间差异无统计学意义(P>0.05)。引流组的住院时间和住院费用低于造口组(P<0.05),但与对照组相比差异无统计学意义(P>0.05),见表2。

Tab.2Comparison of clinical effects between three groups表2 3组患者的疗效指标比较
2.2 术后并发症及随访结果3组患者术后切口感染,盆、腹腔感染,肺部感染发生率及吻合口漏发生率差异均无统计学意义(P>0.05)。术后感染患者经积极对症治疗后均痊愈。经过加强全身营养支持,继续无渣流质饮食,并保持肠腔内及吻合口旁的双腔负压引流(期间并未使用抗生素及生长抑素)后,造口组和引流组的吻合口漏患者均在4周内愈合并行还纳术或拔出引流管,对照组27例吻合口漏患者中有6例在4周内愈合。随访结果表明,3组的复发、转移及死亡比例差异均无统计学意义(P>0.05),见表3。
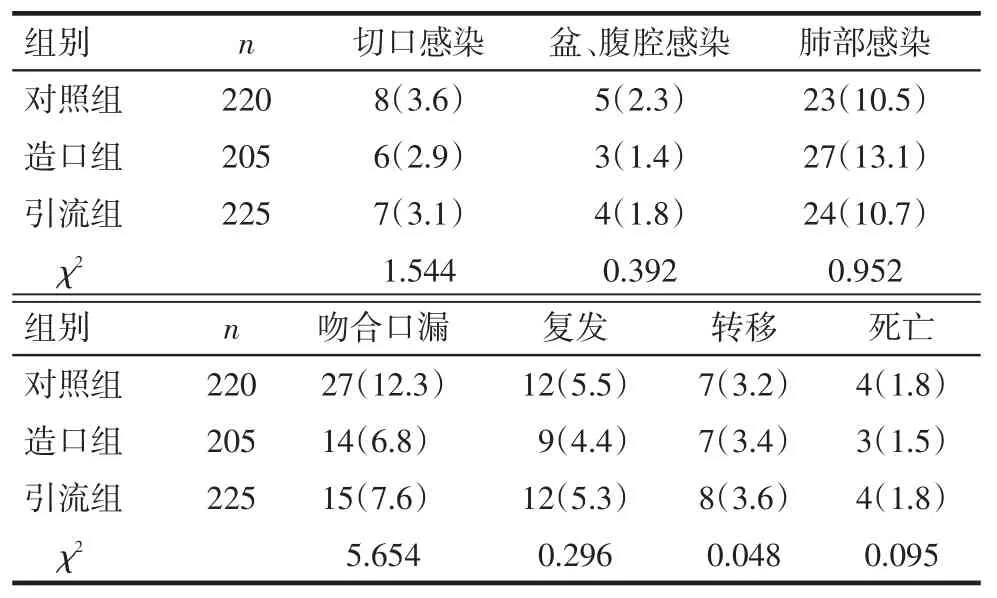
Tab.3Comparison of postoperative complications and outcomes between three groups表3 3组术后并发症及远期疗效比较例(%)
3 讨论
直肠癌是临床上常见的消化道恶性肿瘤之一,其发病率有逐年上升的趋势[6]。肠镜技术和直肠癌根治手术的快速普及使得直肠癌能够及早被发现并治疗。在吻合器的辅助下,低位直肠癌患者实现了保肛治疗。但Dixon术后吻合口漏的发生率居高不下,不仅增加患者痛苦,延长住院时间,部分患者需再次手术进行肠道转流粪便才能治愈[7-8]。资料显示按照TME原则手术治疗直肠癌,吻合口漏的发生率为3%~19%[9]。目前认为吻合口张力过大引起的血运障碍是发生吻合口漏的主要因素,而盆、腹腔感染及引流不畅可加重血运障碍,影响吻合口的愈合[10]。针对吻合口漏发生的原因,临床多采用如下措施:(1)加强围手术期管理,营养支持,纠正贫血、低蛋白血症,糖尿病患者控制血糖,术后早期予以肠内或静脉营养,减轻肠道负荷。(2)术前肠道准备,彻底清洁肠道,减少手术污染。(3)手术时止血确切,充分游离肠管,行结直肠无张力吻合。(4)预防性末端回肠造口,防止小肠内容物过早进入结肠,使结肠处于空虚状态,减少内容物对吻合口的刺激,促进吻合口的愈合。(5)充分引流,促进吻合口的愈合[11]。
为了降低术后吻合口漏的发生率,临床部分采用了预防性的末端回肠造口术,将结直肠空置,促进吻合口的愈合[8,12]。但该方法需要行二期手术还纳,住院时间长,费用高,增加患者痛苦[13]。本研究对比发现,传统Dixon术(对照组)、Dixon术加预防性回肠末端造口术(造口组)和Dixon术加肠腔内、外双套管负压引流(引流组)3种手术方法治疗直肠癌的疗效相似,均未发生围手术期死亡,且术后吻合口漏发生率、并发症发生率及患者的复发、转移和死亡比例无明显差异。但与造口组相比,引流组无需行二次手术,缩短了住院时间,降低了住院费用,减轻了患者负担。再者负压引流可将术后肠腔内产生的气体、消化液及术中残留的粪渣及时排出体外,使肠腔始终保持清洁和空虚状态。同时可充分引流腹腔渗出液,减少盆腔感染的发生,保持肠腔内空虚状态有助于吻合口处肠管血运的改善及水肿消退。负压主动吸引可使引流更有效,并可抵消术后因肛门收缩或结肠逆蠕动导致的肠腔内压力增高[14],且双套引流管的内套管可进气进液,能防止组织吸附于引流管壁,既保证了引流的通畅,又避免了肠黏膜损伤。此外,一旦发生吻合口漏,肠腔内、外双套管持续负压引流能及时有效引流,防止漏出液扩散,促进吻合口漏的愈合[15]。由于样本量有限,吻合口漏发生率总体不高,此次研究尚未得到回肠末端造口和双套管负压引流能够显著降低吻合口漏发生率的结论。为此,笔者将纳入更多的直肠癌患者,以明确双套管负压引流对吻合口漏发生的防治作用。
参考文献
[1]Jiang XH,Zeng BC,Liu GZ.Perioperative nursing of laparoscopic anus-saving operation in treatment of low rectal cancer[J].Clinical Medical&Engineering,2015,22(6):795-796.[江小好,曾冰川,刘国珍.腹腔镜保肛术治疗低位直肠癌的围手术期护理观察[J].临床医学工程,2015,22(6):795-796].doi:10.3969/j. issn.1674-4659.2015.06.0795.
[2]Xu CL,Wang FQ,Wang QY.Effect of double cavity drainage in preventionandtreatmentofcolorectalcancerpostoperative anastomotic fistula[J].Chinese Journal of Misdiagnostics,2012,12(17):4548.[许长录,王富强,王庆玉.双套管引流防治直肠癌Dixon术后吻合口瘘疗效分析[J].中国误诊学杂志,2012,12(17):4548].
[3]Sverrisson I,Nikberg M,Chabok A,et al.Hartmann’s procedure in rectalcancer:apopulation-basedstudyofpostoperative complications[J].Int J Colorectal Dis,2015,30(2):181-186.doi:10.1007/s00384-014-2069-6.
[4]Steinemann DC,Stierle T,Zerz A,et al.Hartmann’s procedure and laparoscopic reversal versus primary anastomosis and ileostomy closure for left colonic perforation[J].Langenbecks Arch Surg,2015,400(5):609-616.doi:10.1007/s00423-015-1319-6.
[5]Zhang JY,Huang YH,Pang FX,et al.Application of the double cavity casing negative pressure drainage by inside and outside of the intestine in the primary resection and anastomosis of left colon cancer combined with acute obstruction[J].Chin J Bases Clin General Surg,2015,22(3):307-311.[张嘉越,黄永鸿,庞飞雄,等.肠腔内外双套管负压引流在左半结肠癌并急性梗阻一期切除吻合中的应用[J].中国普外基础与临床杂志,2015,22(3):307-311].
[6]Li WD,Jia L.Community screening,early diagnose and treatment for colorectal cancer[J].Chin J Clinicians(Electronic Edition),2015,9(5):724-726.[李伟冬,贾林.结直肠癌的社区筛查及早期诊治[J].中华临床医师杂志(电子版),2015,9(5):724-726]. doi:10.3877/cma.j.issn.1674-0785.2015.05.004.
[7]Matsuda M,Tsuruta M,Hasegawa H,et al.Transanal drainage tube placement to prevent anastomotic leakage following colorectal cancer surgery with double stapling reconstruction[J].Surg Today,2016,46(5):613-620.doi:10.1007/s00595-015-1230-3.
[8]Jiménez Fuertes M,Costa Navarro D.Resection and primary anastomosis without diverting ileostomy for left colon emergencies: is it a safe procedure?[J].World J Surg,2012,36(5):1148-1153. doi:10.1007/s00268-012-1513-4.
[9]Lim SB,Yu CS,Kim CW,et al.The types of anastomotic leakage thatdevelopfollowinganteriorresectionforrectalcancer demonstrate distinct characteristics and oncologic outcomes[J].Int J Colorectal Dis,2015,30(11):1533-1540.doi:10.1007/s00384-015-2359-7.
[10]Xia KZ,Zhang J.Application of self-made double cannula combined with continuous negative pressure suction for rectal cancer during operation[J].Chin J Bases Clin General Surg,2014,21(3):367-369.[夏扣柱,张健.自制双套管持续负压吸引在直肠癌术中的应用[J].中国普外基础与临床杂志,2014,21(3):367-369].
[11]Tan TH.Experience of prevention and cure of postoperative anastomotic fistula after low rectal cancer[J].Journal of Hubei University of Science and Technology(Medical Sciences),2014,28(1):41-42.[覃团宏.低位直肠癌保肛根治术后吻合口瘘防治体会[J].湖北科技学院学报(医学版),2014,28(1):41-42].
[12]Park UC,Chung SS,Kim KR,et al.Single-stage procedure with intraoperative colonoscopy and colonic irrigation in patients with obstructing left-sided colonic cancer[J].Int J Colorectal Dis,2004,19(5):487-492.doi:10.1007/s00384-004-0584-6.
[13]Gao F,Xu M,Song F,et al.Prevention of anastomotic fistula formation after low-position Dixon operation[J].Pak J Med Sci,2014,30(5):1007-1010.doi:10.12669/pjms.305.4453.
[14]Li SM,Yang T,Zhang JY,et al.Application of the double cavity casing negative pressure drainage by inside and outside of the intestine in the primary anastomosis of perforation in left hemicolon[J].Chin J Cen Surg,2014,29(11):887-888.[李松明,羊涛,张嘉越,等.肠腔内外双套管负压引流在左半结肠穿孔行一期修补术中的应用[J].中华普通外科杂志,2014,29(11):887-888]. doi:10.3760/cma.j.issn.1007-631X.2014.11.018.
[15]Wang WX,Cheng DW,Qi WD.Clinical research of preset improved double casing in treatment of postoperative anastomotic leakage[J].J Med Theor Prac,2013,26(24):3270-3271.[王维新,成德文,祁卫东.预置改良双套管治疗贲门癌、直肠癌术后吻合口漏的临床研究[J].医学理论与实践,2013,26(24):3270-3271].
(2016-03-23收稿2016-07-22修回)
(本文编辑胡小宁)
Application of the double cavity casing negative pressure drainage by inside and outside of the intestine in the primary resection and anastomosis of low rectal cancer
YAN Wei,LI Songming,LI Rui,ZHANG Jiayue,CEN Yanzeng,LENG Jinli,LAI Yanhua,HE Hongyan,YANG Tao△
Department of General Surgery,NO.303 Hospital of PLA,Nanning 530021,China△
ObjectiveTo investigate the feasibility and safety of the double cavity casing negative pressure drainage by inside and outside of the intestine in the primary resection and anastomosis of low rectal cancer.MethodsA total of 650 cases with low rectal cancer treated in our hospital from January 2009 to December 2014 were retrospectively collected and divided into control group(n=220),stoma group(n=205)and drainage group(n=225).The control group was received Dixon (low rectal anterior resection),the stoma group was treated with Dixon and ileostomy,while the drainage group was underwent double cavity casing negative pressure drainage by inside and outside of the intestine in the primary resection and anastomosis.The operation time,bleeding volume,the period of anal exhaust after operation and hospital expenses were compared between three groups.Postoperative follow-up was performed,and anastomotic leakage,postoperative infection and other complications were analyzed.ResultsThere were no significant differences in the operation time,bleeding volume and the period of anal exhaust after operation between three groups(P>0.05).The hospital stay and expenses were shorter and lower in drainage group than those in stoma group(P<0.05).In addition,there were no significant differences in wound infection,pelvic infection,and pulmonary infection between three groups(P>0.05).All patients were followed up, and the mortality,the recurrence rate and metastasis rate were not significantly different between three groups(P>0.05). ConclusionThe application of double cavity casing negative pressure drainage is likely to reduce the incidence of anastomotic leakage in Dixon,while the effect needs to be confirmed by large clinical trial,at the same time,patients enjoy shorter hospital stay,fewer suffering and lower expense of hospitalization.
rectal neoplasms;anastomosis,surgical;drainage;postoperative complications;low rectal cancer;Dixon operation;double cavity casing;anastomotic leakage
R657.1
A
10.11958/20160087
中国人民解放军第三〇三医院普通外科(邮编530021)
闫威(1981),男,硕士研究生,主治医师,主要从事结、直肠肛门外科临床研究
△通讯作者E-mail:154869200@qq.com