TI-RADS分级和TSH∶Tg比值鉴别甲状腺结节良恶性的研究
焦妍,赵洪刚,张遵城
TI-RADS分级和TSH∶Tg比值鉴别甲状腺结节良恶性的研究
焦妍,赵洪刚,张遵城△
目的评价B超甲状腺影像报告数据系统(TI-RADS)分级和促甲状腺素(TSH)∶甲状腺球蛋白(Tg)比值对甲状腺结节良恶性的诊断效能。方法选择2015年1月—12月我院甲乳外科甲状腺结节手术患者156例,经手术后病理诊断甲状腺乳头状癌患者50例,良性甲状腺结节患者106例。计算患者TSH∶Tg比值,采用受试者工作特征曲线(ROC)计算诊断切值,检测值<切值积0分,检测值≥切值积1分。对TI-RADS分级进行量化,3级及以下、4a、4b、4c、5级分别积0、1、2、3、4分。联用积分为TSH∶Tg比值积分和TI-RADS分级积分之和。结果TSH∶Tg比值鉴别甲状腺结节良恶性ROC曲线下面积(AUC)为0.736,敏感度、特异度、阳性预测值、阴性预测值、诊断符合率分为64.0%、82.1%、62.7%、82.8%、76.3%。TI-RADS分级积分鉴别甲状腺结节良恶性的AUC为0.753,敏感度、特异度、阳性预测值、阴性预测值、诊断符合率分为84.0%、72.6%、59.2%、90.6%、76.3%。联用积分鉴别甲状腺结节良恶性的AUC为0.839,敏感度、特异度、阳性预测值、阴性预测值、诊断符合率分为74.0%、86.1%、71.1%、87.5%、82.1%。结论联用TI-RADS分级和TSH∶Tg比值鉴别甲状腺结节良恶性诊断效率优于单用一种方法,且简便易行,建议临床医师使用。
甲状腺结节;促甲状腺素;甲状腺球蛋白;甲状腺乳头状癌;促甲状腺素∶甲状腺球蛋白比值;B超甲状腺影像报告数据系统
2010年美国甲状腺协会(ATA)的调查指出,正常人群触诊甲状腺结节检出率为4%~10%,运用超声其检出率提高到19%~67%,甲状腺结节患者大部分为良性病变,约5%的患者会发生恶变[1]。2011年我国《甲状腺结节和分化型甲状腺癌诊治指南》提到,触诊获得的甲状腺结节患病率为3%~7%,高分辨率B超检查获得的甲状腺结节的患病率为20%~76%,甲状腺结节中的甲状腺癌的患病率为5%~15%。良恶性甲状腺结节的临床处理不同,对患者生存质量的影响也存在显著差异。因此,甲状腺结节评估的要点是良恶性鉴别[2]。现阶段鉴别甲状腺结节性质的无创检查手段主要是超声,受结节大小和操作者水平的干扰较大。目前临床还缺少理想的进行甲状腺结节性质鉴别的血液检验指标。本研究联合使用影像和血液2种方法鉴别甲状腺结节的性质,旨在建立一种简便、可量化的方法来提高其检测的准确率。
1 资料与方法
1.1 一般资料选择2015年1月—12月我院甲乳外科甲状腺结节手术患者156例,其中分化型甲状腺癌患者(恶性组)50例,良性甲状腺结节患者(良性组)106例,均经手术后病理诊断。恶性组男28例,女22例,平均年龄(54.1±13.9)岁;良性组男49例,女57例,平均年龄(53.2±11.4)岁。2组性别(χ2=0.323)、年龄(t=1.353)差异均无统计学意义。所有患者甲状腺激素、甲状腺过氧化物酶抗体(TPOAb)、甲状腺球蛋白抗体(TGAb)、促甲状腺素受体抗体(TRAb)均正常,无甲状腺炎和其他甲状腺疾病病史,未服用过影响甲状腺功能的药物,未进行过任何激素治疗,无颈部手术和外伤史,未进行过甲状腺细针穿刺,无自身免疫疾病和除甲状腺外的肿瘤,无慢性肝病、结核等慢性病,无肝肾功能异常。
1.2 检测指标和方法入院第2天清晨空腹抽取肘正中静脉血,3 000 r/min离心10 min,血清4 h内上机检测,促甲状腺素(TSH)使用centaur xp全自动化学发光检测仪及配套试剂进行检测。甲状腺球蛋白(Tg)使用罗氏cobas E411全自动电化学发光检测仪进行检测。甲状腺B超采用飞利浦IE33彩超检测仪。根据B超甲状腺影像报告数据系统(TIRADS)分2、3、4a、4b、4c、5级进行报告,所有报告均由2位中级以上职称医师共同发出。采用积分值对分级进行量化,3级及以下积0分,4a级积1分,4b级积2分,4c级积3分,5级积4分。计算患者TSH∶Tg比值,TSH∶Tg(IU/g)=TSH(mIU/L)/Tg(μg/L)×1 000[3]。采用受试者工作特征曲线(ROC)法计算TSH∶Tg比值的诊断切值,检测值<诊断切值的患者积0分,检测值≥诊断切值的患者积1分,联用积分为TSH∶Tg比值积分和TI-RADS积分之和。
1.3 统计学方法采用SPSS 19.0软件进行统计学处理,正态性检验采用Shapiro-Wilk法,符合正态分布的计量资料以均数±标准差表示,组间比较采用t检验;不符合正态分布的计量资料以M(P25,P75)表示,组间比较采用Wilcoxon Mann-Whitney秩和检验。计数资料组间比较采用χ2检验。绘制ROC曲线,采用Youden指数最大法确定检测最佳临界值。P<0.05为差异有统计学意义。
2 结果
2.12 组TSH∶Tg比值、TI-RADS分级积分和联用积分比较恶性组TSH∶Tg比值、TI-RADS分级积分和联用积分均高于良性组,差异均有统计学意义(均P<0.05),见表1。
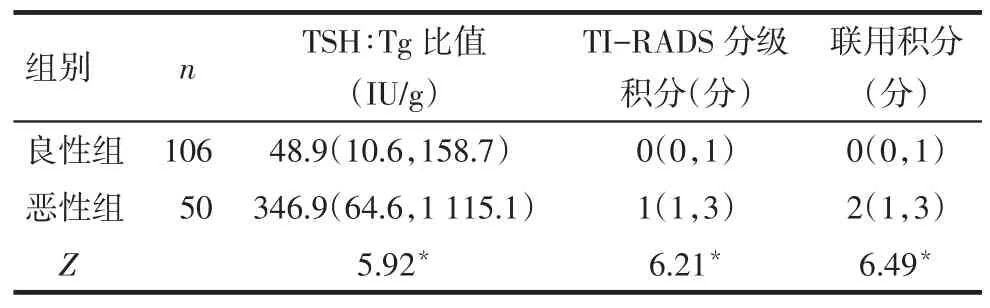
Tab.1Comparison of TSH:Tg ratio,TI-RADS scale and combination scale between two groups表1 2组TSH∶Tg比值、TI-RADS分级积分和联用积分比较[M(P25,P75)]
2.2 不同指标对甲状腺结节良恶性的诊断效能评价联用积分的曲线下面积(AUC)均高于TSH:Tg比值和TI-RADS分级积分(均P<0.05),见图1,表2。联用积分对甲状腺结节良恶性诊断的敏感度高于TSH:Tg比值,低于TI-RADS分级积分;但其特异度和诊断符合率均高于TSH:Tg比值和TI-RADS分级积分,联用积分的诊断效能最优,见表3。
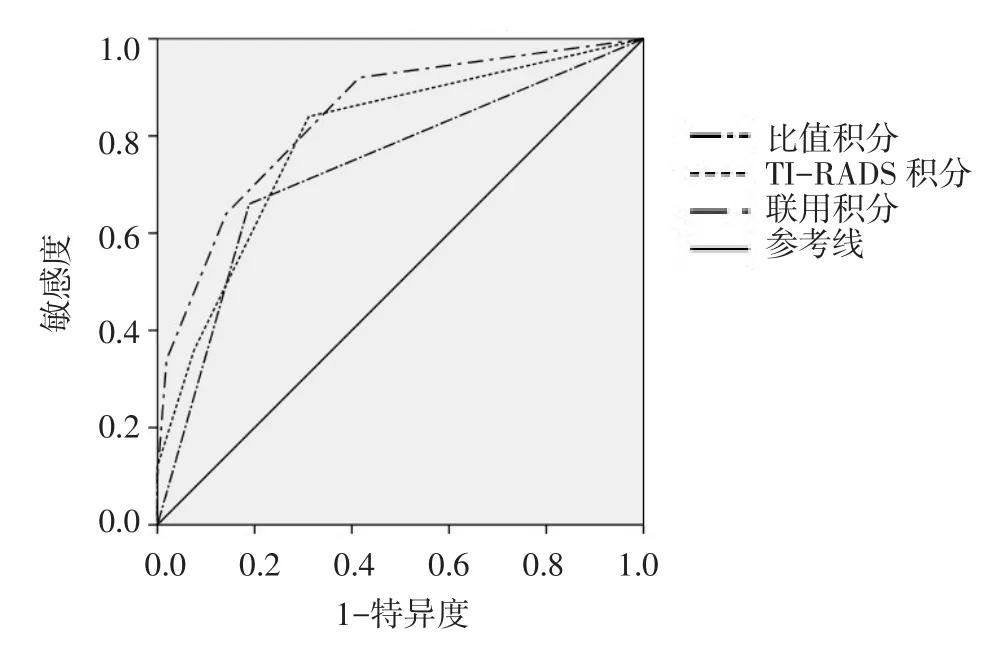
Fig.1ROC analysis for TSH:Tg ratio,TI-RADS scale and combination scale图1 TSH∶Tg比值、TI-RADS分级积分和联用积分的ROC

Tab.2Comparison of area under the roc curve(AUC) between different indicators of benign and malignant thyroid nodules表2 不同指标鉴别甲状腺结节良恶性的AUC比较

Tab.3The diagnostic effective analysis of TSH:Tg ratio, TI-RADS scale and combination scale表3 不同指标对甲状腺结节良恶性的诊断效能评价(%)
3 讨论
现阶段临床术前鉴别甲状腺结节性质的无创检查手段主要是B超。2009年Horvath等[4]借鉴美国放射学会制定的乳腺影像报告和数据系统超声分级诊断标准首次提出TI-RADS分级诊断标准,现今已经成为一种标准化的甲状腺超声术语。章晶等[5]报道,TI-RADS 2、3、4a、4b、4c、5级鉴别出甲状腺结节的实际恶性率分别为0、0.5%、4.6%、25%、73%、 94%,可以达到初步鉴别甲状腺结节良恶性的目的。本研究将患者分级结果采用积分值量化,由于2、3级恶性率极低,分级为2、3级的患者不积分,分级为4a、4b、4c、5级的患者分别积1、2、3、4分。采用TI-RADS分级积分对患者进行诊断,AUC为0.753,诊断符合率为76.3%。使用积分法量化分级结果对患者进行诊断可以达到区别良恶性的目的,但诊断效能不够理想。推测可能由于影像检查手段的结果判断受到结节大小和操作者水平影响造成。因此,本研究拟引入客观性较强的血液检验指标和TI-RADS指标联合使用,以提高检验准确性。
目前对于甲状腺结节性质鉴别的血液检验指标的研究主要集中于TSH和Tg两方面。分化型甲状腺癌细胞膜表面可表达促甲状腺素受体,TSH通过表达多种特异蛋白和增加细胞生长速率途径来刺激癌细胞[6]。多项研究表明,TSH水平较高的患者其甲状腺结节的恶性概率可能较高[7-8],由此可以推断,TSH很可能在甲状腺癌的发生发展过程中起促进作用[9-10]。Tg是参与甲状腺激素合成的一种糖蛋白,是甲状腺激素合成的副产物,正常甲状腺组织和甲状腺癌细胞都可以产生。目前研究普遍认为术前检测Tg水平对于评估甲状腺结节意义不大[2,11-13]。血清Tg水平取决于TSH受体的刺激程度,所以应同时检测Tg和TSH,在解释Tg水平时一定要充分考虑TSH水平对其的影响[14]。
中山大学肿瘤防治中心研究显示,术前应用TSH∶Tg比值评估甲状腺肿瘤的良恶性,其AUC为0.713,敏感度与特异度分别为55.47%和70.8%,阳性预测值为70.8%,该研究认为术前血清TSH∶Tg比值可以作为细针穿刺细胞病理学(FNA)及甲状腺彩超的有效补充[3]。本文应用TSH∶Tg比值鉴别甲状腺结节良恶性的AUC为0.736,敏感度与特异度分别为64.0%和82.1%,阳性预测值为62.7%。敏感度与特异度之和最大时,TSH∶Tg比值的切点值为188.44 IU/g,远高于文献的24.22 IU/g,推测是由于方法学不同造成检测数值的差异,本文采用的是化学发光法,文献使用的是放射免疫法,这一点与文献提示各实验室建立自身参考值的观点相符。与中山大学研究中综合考虑纳入了TGAb正常与异常的患者不同,本文参考目前多项研究的观点,认为患者体内存在的TGAb会干扰Tg的检测[14-16],故在选择病例时排除了TGAb阳性的患者,减少了可能存在的干扰。
本研究应用TSH∶Tg比值鉴别甲状腺结节良恶性的诊断符合率为76.3%,具有一定的鉴别诊断价值,但仍不够理想。为了提高诊断准确率,本研究联合使用两种量化后的指标,将TSH∶Tg比值以188.44 IU/g作为切值区别积分,小于该切值的患者积0分,大于等于该切值的患者积1分。以TSH∶Tg比值积分和TI-RADS分级积分之和作为联用积分,绘制ROC曲线。联用积分的AUC为0.839,诊断符合率为82.1%,诊断效率优于单用一种方法。且该方法简便易行,不增加患者负担,计算简单,可操作性强,建议临床医师使用。
[1]Gharib H,Papini E,Paschke R,et al.American Association of Clinical Endocrinologists,Associazione Medici Endocrinologi,and European Thyroid Association Medical guidelines for clinical practice for the diagnosis and management of thyroid nodules: executive summary of recommendations[J].Endocr Pract,2010,16(3):468-475.
[2]Chinese Society of Endocrinology.Management guidelines for patients with thyroid nodules and differentiated thyroid cancer[J]. Chin J Nucl Med Mol Imaging,2013,33(2):1249-1272.[中华医学会内分泌学分会.甲状腺结节和分化型甲状腺癌诊治指南[J].中华核医学与分子影像杂志,2013,33(2):1249-1272]. doi:10.3760/cma.j.issn.2095-2848.2013.02.003.
[3]Wang L,Li H,Yang Z,et al.Preoperative serum thyrotropin to thyroglobulin ratio is effective for thyroid nodule evaluation in euthyroid patients[J].Otolaryngol Head Neck Surg,2015,153(1):15-19.doi:10.1177/0194599815579877.
[4]Horvath E,Majlis S,Rossi R,et al.An ultrasonogram reporting system for thyroid nodules stratifying cancer risk for clinical management[J].J Clin Endocrinol Metab,2009,94(5):1748-1751.doi:10.1210/jc.2008-1724.
[5]Zhang J,Xu HX,Zhang YF,et al.Prospective validation of the thyroid imaging reporting and data system on thyroid nodules[J]. Clin J Med Ultrasound(Electronic Edition),2014,11(2):62-65.[章晶,徐辉雄,张一峰,等.甲状腺影像报告和数据系统在甲状腺结节分类中的前瞻性验证[J].中华医学超声杂志:电子版,2014,11(2):62-65].doi:10.3877/cma.j.issn.1672-6448.2014.02.015.
[6]D’Agostino M,Sponziello M,Puppin C,et al.Different expression of TSH receptor and NIS genes in thyroid cancer:role of epigenetics.[J].J Mol Endocrinol,2013,52(2):121-131.doi:10.1530/JME-13-0160.
[7]Moon SS,Lee YS,Lee IK,et al.Serum thyrotropin as a risk factor forthyroidmalignancyineuthyroidsubjectswiththyroid micronodule[J].Head Neck,2012,34(7):949-952.doi:10.1002/ hed.21828.
[8]Mussa A,Salerno MC,Bona G,et al.Serum thyrotropin concentration in children with isolated thyroid nodules[J].J Pediatr,2013,163(5):1465-1470.doi:10.1016/j.jpeds.2013.07.003.
[9]He H,Li W,Liyanarachchi S.Genetic predisposition to papillary thyroid carcinoma:involvement of FOXE1,TSHR,and a novel lincRNA gene,PTCSC2[J].J Clin Endocrinol Metab,2015,100(1):E164-172.doi:10.1210/jc.2014-2147.
[10]Khan MS,Pandith AA,Masoodi SR,et al.Epigenetic silencing of TSHR gene in thyroid cancer patients in relation to their BRAF V600E mutation status[J].Endocrine,2014,47(2):449-455.doi:10.1007/s12020-014-0319-6.
[11]Suh I,Vriens MR,Guerrero MA,et al.Serum thyroglobulin is a poor diagnostic biomarker of malignancy in follicular and Hurthlecell neoplasms of the thyroid[J].Am J Surg,2010,200(1):41-46. doi:10.1016/j.amjsurg.2009.08.030.
[12]Lee EK,Chung KW,Min HS,et al.Preoperative serum thyroglobulin as a useful predictive marker to differentiate follicular thyroid cancer from benign nodules in indeterminate nodules[J].J Korean MedSci,2012,27(9):1014-1018.doi:10.3346/jkms.2012.27.9.1014.
[13]Schneider DF,Chen H.New developments in the diagnosis and treatment of thyroid cancer[J].CA Cancer J Clin,2013,63(6):373-394.doi:10.3322/caac.21195.
[14]Perros P,Boelaert K,Colley S,et al.British Thyroid Association Guidelines for the Management of Thyroid Cancer[J].Clin Endocrinol(Oxf),2014,81(Suppl1):1-122.doi:10.1111/ cen.12515.
[15]Spencer CA.Clinical review:Clinical utility of thyroglobulin antibody(TgAb)measurements for patients with differentiated thyroid cancers(DTC)[J].J Clin Endocrinol Metab,2011,96(12):3615-3627.doi:10.1210/jc.2011-1740.
[16]Spencer CA,Bergoglio LM,Kazarosyan M,et al.Clinical impact of thyroglobulin(Tg)and Tg autoantibody method differences on the management of patients with differentiated thyroid carcinomas[J].J Clin Endocrinol Metab,2005,90(10):5566-5575.
(2016-03-01收稿2016-08-27修回)
(本文编辑陈丽洁)
The combination of the TSH∶Tg ratio and TI-RADS for identification of benign and malignant thyroid nodules
JIAO Yan,ZHAO Honggang,ZHANG Zuncheng△
Department of Nuclear Medicine,The Second Hospital,Tianjin Medical University,Tianjin 300211,China△
ObjectiveTo assess the efficiency of thyroid stimulating hormone(TSH):thyroid globulin(Tg)ratio and ultrasound thyroid imaging reporting data system(TI-RADS)for thyroid nodule evaluation in euthyroid patients.Methods A total of 156 patients with thyroid nodules hospitalized in the department of thyroid breast surgery from January to December 2015 were included in this study.There were 50 patients were diagnosed as papillary thyroid carcinoma,and 106 patients were benign thyroid nodules confirmed by pathological diagnosis after operation.The ratio of TSH:Tg was calculatedin patients.The cut-off point was calculated using the receiver operating characteristic(ROC)curve analysis.The measurement value<tangent was 0 point,and the measurement value≥tangent was 1 point.TI-RADS diagnostic criteria was evaluated and calculated.The nodule in TI-RADS categories 1,2 and 3 was 0 points,The nodule in TI-RADS categories 4a,4b,4c,5 was 1,2,3,4 points,respectively.The combination score was the sum of the TSH:Tg ratio score and TI-RADS score.ResultsThe area under the receiver operating characteristic curves of the TSH:Tg ratio was 0.736.The sensitivity,specificity,positive predictive value,negative predictive value,diagnose accordance rate were 64.0%,82.1%, 62.7%,82.8%,76.3%,respectively.The AUC of TI-RADS was 0.753,the sensitivity,specificity,positive predictive value, negative predictive value,diagnose accordance rate were 84.0%,72.6%,59.2%,90.6%,76.3%,respectively.The AUC of the combination of the TSH:Tg ratio and TI-RADS was 0.839,the sensitivity,specificity,positive predictive value,negative predictive value,diagnose accordance rate were 74.0%,86.1%,71.1%,87.5%,82.1%,respectively.ConclusionThe combination diagnosis of the TSH:Tg ratio and TI-RADS for thyroid nodule evaluation in euthyroid patients is better than that of only one method,which is worth clinical popularizing and application.
thyroid nodule;thyrotropin;thyroglobulin;papillary thyroid carcinoma;TSH∶Tg ratio;TI-RADS
R653.2
A
10.11958/20160091
天津医科大学第二医院核医学科(邮编300211)
焦妍(1983),女,硕士在读,主管技师,主要从事内分泌疾病和肿瘤的实验室诊断研究
△通讯作者E-mail:zhangzuncheng@sina.com