置管方式及时间对肾盂输尿管成形术后患儿尿路感染的影响
谢起根 李作青 徐哲 孙俊杰 周李 苏诚
·临床研究论著·
置管方式及时间对肾盂输尿管成形术后患儿尿路感染的影响
谢起根 李作青 徐哲 孙俊杰 周李 苏诚
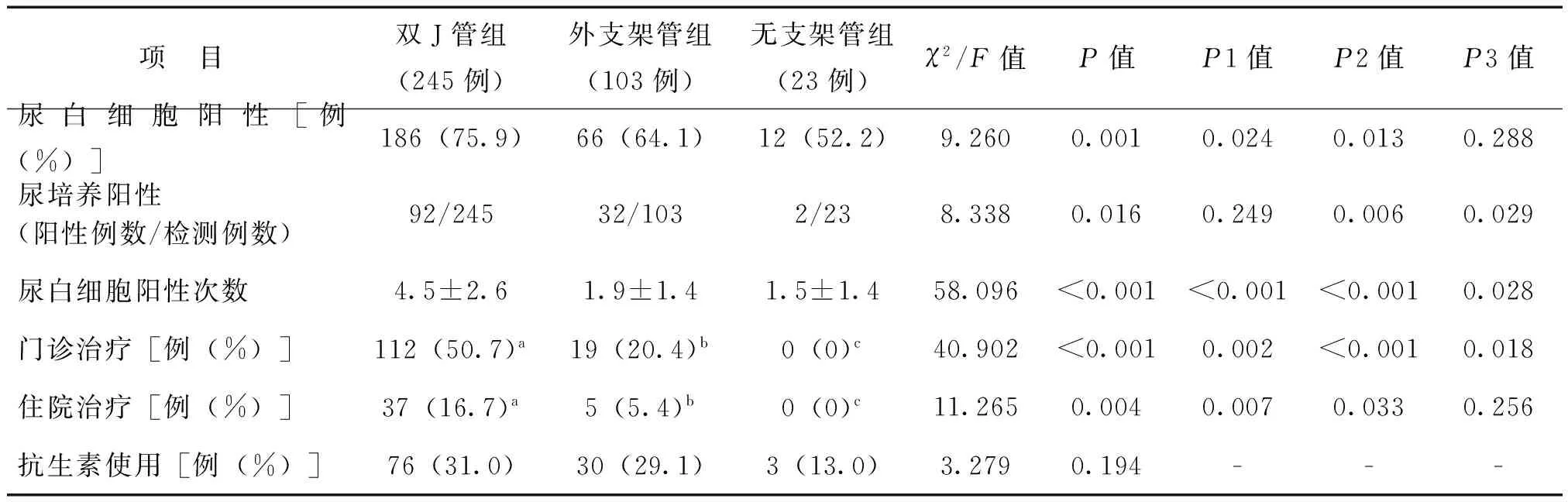
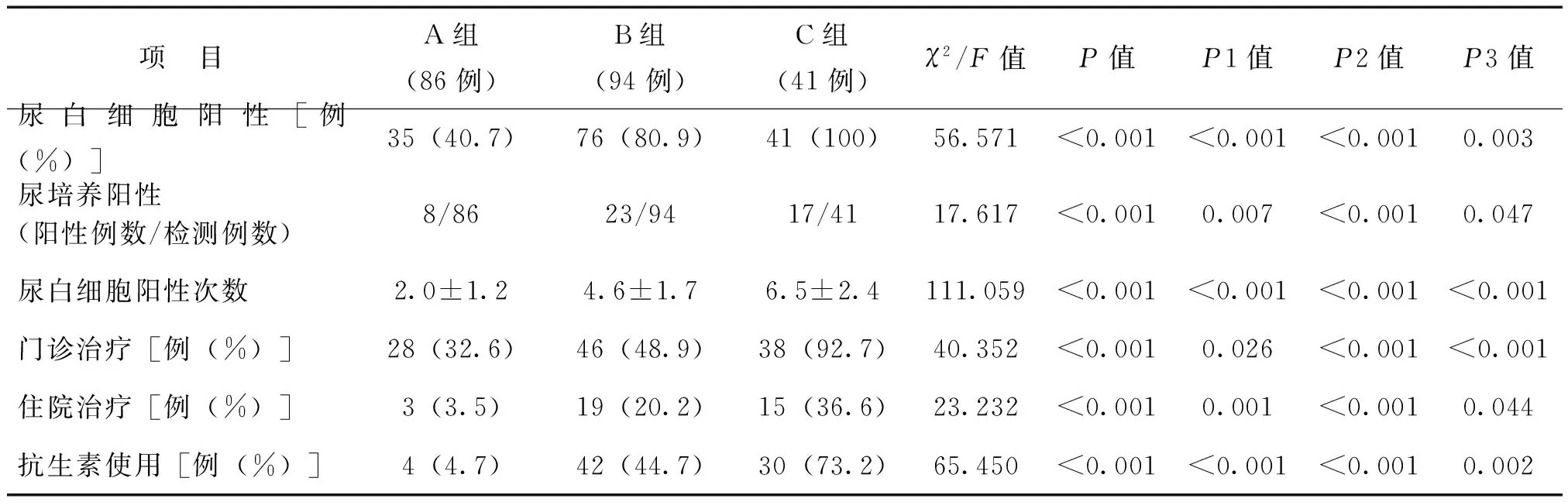
目的 探讨置管方式及时间对肾盂输尿管(UPJ)成形术后患儿尿路感染发生的影响。方法 收集371例UPJ成形术患儿的临床资料。根据置管方式不同,分为双J管组(245例)、外支架管组(103例)和无支架管组(23例)。双J管组中根据术后双J管留置时间长短分为≤45 d组(A组)、46~105 d组(B组)和>105 d组(C组)。所有患儿根据有无尿路感染分为尿路感染组(126例)和无尿路感染组(245例)。分别收集各组患儿的术前临床资料及定期复查的尿常规、尿培养结果,比较各组尿白细胞阳性率、尿白细胞阳性次数、尿培养阳性率、住院治疗率、门诊治疗率、抗生素使用情况、远期手术成功率间的差异。结果 双J管组、外支架管组、无支架管组患儿在术前或术后早期的尿路感染率组间比较差异均无统计学意义(P均>0.05);出院后双J管组尿路感染发生率高达21.7%,高于外支架管组(2.1%,P<0.01)及无支架管组(0%,P<0.017)。术后双J管组尿白细胞阳性次数多于外支架管组,其门诊治疗率和住院治疗率均高于外支架管组(P均<0.017)。与无支架管组比较,双J管组尿白细胞阳性次数较多,尿白细胞阳性率、尿培养阳性率和门诊治疗率较高(P均<0.017)。双J管组各亚组尿白细胞阳性率、尿常规阳性次数、出院后抗生素使用率的比较中,均为A组 肾盂输尿管成形术;置管;尿路感染 离断式肾盂输尿管(UPJ)成形术是治疗梗阻性肾积水的标准术式,术后输尿管的置管方式有内置双J管、输尿管外支架管、无支架管等方式。因护理方便、创伤小、术后恢复快,内置双J管是目前最常用的置管方式。外支架管术式无需二次入院麻醉拔管,但留置管道多,护理困难。随着腹腔镜及机器人辅助手术的应用,近年无支架管术式应用报道越来越多。尿路感染是UPJ成形术后最常见的并发症[1-3]。双J管留置期间形成膀胱-输尿管尿液反流,外支架管容易造成逆行感染,无支架术式如出现引流不畅势必增加感染风险,各引流方式均存在尿路感染的易感因素。双J管留置时间仍有较大的随意性。目前对置管方式及时间对尿路感染发生影响的研究较少,本研究通过对2010至2015年期间我科收治的371例UPJ成形术患儿进行回顾性分析,探讨不同引流方式和时间对尿路感染发生的影响以及双J管的拔管时机。 一、研究对象 本研究共纳入了2010年1月至2015年12月我科连续收治的371例行单侧开放离断式UPJ成形术治疗梗阻性肾积水患儿,排除双侧、有肾输尿管合并症、其他手术方式、随访资料不全者。其中男300例、女71例,年龄5 d~13岁、中位年龄47个月,左侧248例、右侧123例,中度肾积水169例、重度肾积水202例。根据置管方式不同,分为双J管组(245例)、外支架管组(103例)和无支架管组(23例)。3组患儿的性别构成比、年龄、梗阻侧构成比、肾积水程度比较差异均无统计学意义(P均>0.05),见表1。本研究经中山大学附属第一医院医学伦理委员会审批通过,所有患者均已签署知情同意书。 表1 3组梗阻性肾积水患儿的术前一般资料比较 二、 置管方式及术后复查 双J管组术中留置双J管(无抗反流装置)1条,放或不放置肾周引流管,嘱术后1~6个月拔除双J管。外支架管组留置外支架管、肾造瘘管各1条,放或不放置肾周引流管,术后7~12 d注射亚甲蓝观察输尿管排尿通畅后,拔除外支架管及肾造瘘管,如不通畅则延期拔管。无支架管组术后不放置支架管引流,放置肾周引流管1条。分别于术后住院期间(术后早期)、1、3、6、12个月定期复查尿常规及尿培养(细菌和真菌);随访期间如有尿路感染症状时,加做尿常规和尿培养。尿路感染的诊断采用2015中国专家共识版标准。 三、观察内容 观察并比较双J管组、外支架管组和无支架管组患儿的尿白细胞阳性率、尿白细胞阳性次数、尿培养阳性率、住院和门诊治疗(尿路感染)率、限制及特殊使用级(三代及三代以上头孢、碳青霉烯类、万古霉素、抗真菌类等)抗生素使用率。双J管组再根据术后双J管留置时间长短分为≤45 d组(A组)、46~105 d组(B组)和>105 d组(C组),比较前述指标在A、B、C组间的差异。双J管组、外支架管组和无支架管组再根据有无尿路感染分为尿路感染组和无尿路感染组,比较其远期手术成功率。 四、统计学处理 一、双J管组、外支架管组、无支架管组患儿尿路感染发生率的比较 双J管组221例患儿获得随访,随访成功率90.4%,外支架管组93例患儿获得随访,随访成功率90.2%,无支架管组全部患儿获得随访,3组随访率比较差异无统计学意义(P>0.05)。3组患儿的术前尿路感染发生率比较差异无统计学意义(P>0.05);双J管及外支架管组术后早期尿路感染率高达32.7%及30.1%,略高于无支架管组(8.7%),但比较差异无统计学意义(P>0.05)。出院后3组患儿的尿路感染率比较差异有统计学意义(P<0.001),其中双J管组尿路感染发生率高达21.7%,高于外支架管组(2.1%,P<0.001)及无支架管组(0%,P<0.017);外支架管组和无支架管组尿路感染发生率极低,2组比较差异无统计学意义(P>0.05),见表2。 表2 UPJ手术前后3组梗阻性肾积水 患儿的尿路感染率比较 例(%) 注:出院后获随访例数,a221例、b93例、c23例 二、 双J管组、外支架管组、无支架管组患儿UPJ术后尿路感染的严重程度比较 3组患儿限制及特殊使用级抗生素使用率比较差异无统计学意义(P>0.05)。与外支架管组相比,双J管组尿白细胞阳性次数较多,门诊治疗率和住院治疗率较高(P均<0.017);与无支架管组相比,双J管组尿白细胞阳性次数较多,尿白细胞阳性率、尿培养阳性率和门诊治疗率较高(P均<0.017)。外支架管组尿培养阳性率、尿白细胞阳性次数、门诊治疗率与无支架管组组间比较差异均无统计学意义(P均>0.017),见表3。 三、出院后双J管组支架管留置不同时间尿路感染的严重程度比较 双J管组中98例支架管留置时间≤45 d,86例获得规律随访,为A组;103例留置时间为46~105 d,94例获得规律随访,为B组;余44例放置时间>105 d,41例获得规律随访,为C组。A、B、C组尿白细胞阳性率、尿常规阳性次数、出院后限制及特殊使用级抗生素使用率的比较中,均为A组 四、尿路感染组和无尿路感染组患儿的远期手术成功率比较 所有患儿根据有无尿路感染分为尿路感染组(126例)和无尿路感染组(245例)。尿路感染组有7例因吻合口梗阻再手术,6例证实有梗阻加重但未手术,远期手术成功率为89.7%(113/126)。无尿路感染组只有1例因梗阻加重再手术,7例证实有梗阻加重但未手术,远期手术成功率为96.7%(237/245)。尿路感染组远期手术成功率低于无尿路感染组(χ2=7.749,P=0.005)。 表3 3组梗阻性肾积水患儿UPJ术后尿路感染的严重程度比较 注:出院后获随访例数,a221例、b93例、c23例;P1为双J管组与外支架管组比较,P2为双J管组与无支架管组比较,P3为外支架管组与无支架管组比较 表4 出院后双J管组中支架管留置不同时间的尿路感染严重程度比较 注:P1 为A组与B组比较,P2为 A组与C组比较,P3为B组与C组比较 UPJ成形术后多留置支架管[4]。留置管作为异物,容易移行和定植细菌,是感染发生的高危因素。Aydin等[5]研究发现,拔除双J管前的尿培养病原菌和双J管本身培养的病原菌相同,认为双J管细菌定植是造成UPJ术后尿路感染的主要原因。García-Aparicio等[6]研究发现,UPJ成形术后双J管细菌定植率高,使尿路感染风险升高。多项研究均发现,双J管内细菌定植率高(29.4%~58.9%),但仅有部分患者有症状,提示部分患者虽有感染但并无症状[5-7]。本研究发现,出院后双J管组患儿的尿路感染率高于无支架管组和外支架管组,外支架管组拔管出院后的尿路感染率明显下降,且与无支架管组尿路感染率相近,证实了管道留置与尿路感染之间的关系。留置双J管的感染风险增大,其原因可能是:①留置双J管期间可形成膀胱-输尿管尿液反流,废用了输尿管的蠕动排尿功能,较轻的下尿路感染容易蔓延至上尿路。有鉴于此,目前有报道在输尿管吻合术中使用含抗反流装置的双J管作为支架预防感染,报道的效果虽不理想,但值得进一步研究[8-9]。②脱落输尿管上皮细胞、白细胞、红细胞等尿液沉渣容易附着在双J管中,甚至造成管道的堵塞,进而引起尿液引流不畅,部分患儿因梗阻造成的感染需紧急拔管。③细菌容易定植于双J管,尿液对细菌的冲刷作用受限,感染较难控制,容易反复。无支架管的术式虽可降低细菌定植风险,但仍有感染发生,可能与吻合口梗阻及尿漏有关。外支架管的术式在住院期间留置管道多,易致细菌逆行感染,因而术后早期感染率并不低于内支架管术式。保持膀胱尿液无菌才能预防尿路感染,建议术后出院时应完全控制尿路感染,确认尿培养阴性,出院后注意保持尿道外口清洁(特别是女性患儿,必要时口服抗生素预防感染[10-11]。一旦感染,应多次尿培养,选用敏感抗生素,必要时可考虑急诊拔除双J管。 双J管可留置最长12个月,多建议于术后1~6个月拔除,拔管时间目前仍无统一指南,且患儿依从性差,拔管时机较为随意,甚至有病例多年后因出现严重并发症后才返院拔管,但技术难度极大[12-13]。本研究发现,双J管留置时间越长,尿路感染率越高,消耗的医疗精力和治疗费用越高。快速康复外科理念已经被大型医疗中心肯定,长时间留置双J管并不利于患儿的快速康复[14]。留置支架管的主要目的之一是防止吻合口狭窄,减少再手术率。目前多篇文献报道,无支架管术式在UPJ成形术中的运用,并未发现狭窄率增高,吻合口狭窄与否与支架管留置时间长短可能并无关系,延长置管时间并不能获得更好的远期疗效[1-2,15]。相反,本研究发现,尿路感染组远期手术成功率稍低于无感染组,且术后45 d内拔除双J管者的尿路感染率明显低于45 d以上者。权衡留置双J管造成高感染风险和防狭窄效益,本研究建议双J管应于术后1个月以内拔除。 有研究表明,术前反复尿路感染致肾瘢痕形成,影响远期肾功能,建议术前尿路感染应作为新生儿肾积水手术指征之一[16]。但目前术后尿路感染对肾功能的影响研究较少。本研究发现,术后尿路感染组的远期手术成功率低于无尿路感染组,其原因可能是:①尿路感染加重吻合口狭窄;②反复尿路感染为吻合口狭窄的临床表现;③尿路感染和吻合口狭窄两者之间相互影响。因此,建议积极控制尿路感染,合理使用抗生素,采用合适置管方式和时间,以降低尿路感染对肾积水远期手术疗效的影响。 综上所述,双J管的留置增加尿路感染风险及严重程度,尿路感染的发生影响肾积水术后远期疗效,建议术后1个月以内拔除。 [1]Kumar V, Mandhani A. Laparoscopic stentless pyeloplasty: an early experience.Indian J Urol,2010,26(1):50-55. [2]Rodriguez AR, Rich MA, Swana HS. Stentless pediatric robotic pyeloplasty.Ther Adv Urol, 2012,4(2):57-60. [3]Paz A, Amiel GE, Pick N, Moskovitz B, Nativ O, Potasman I.Febrile complications following insertion of 100 double-J ureteral stents.J Endourol,2005,19(2):147-150. [4]王林,郭宗远,吴荣德,于启海,王淑琴,杨静.小儿先天性肾积水30例的手术治疗.新医学,2005, 36(7):402-403. [5]Aydin HR, Irkilata L, Aydin M, Gorgun S, Demirel HC, Adanur S, Keles M, Atilla A, Atilla MK.Incidence of bacterial colonisation after indwelling of double-J ureteral stent.Arch Ital Urol Androl,2016,87(4):291-294. [6]García-Aparicio L, Blázquez-Gómez E, Martin O, Krauel L, de Haro I, Rodó J.Bacterial characteristics and clinical significance of ureteral double-J stents in children.Actas Urol Esp,2015,39(1):535-536. [7]Uvin P, Van Baelen A, Verhaegen J, Bogaert G.Ureteral stents do not cause bacterial infections in children after ureteral reimplantation.Urology,2011,78(1):154-158. [9]Park CJ, Kim HW, Jeong S, Seo S, Park Y, Moon HS, Lee JH. Anti-reflux ureteral stent with polymeric flap valve using three-dimensional printing: an in vitro study. J Endourol,2015,29(8):933-938. [10]Moore SS, Bahat H, Rachmiel M, Ziv-Baran T, Youngster I, Goldman M. Guidelines for urinary tract infections and antenatal hydronephrosis should be gender specific.Acta Paediatr,2015,104(11):e512-e517. [11]Ferroni MC, Lyon TD, Rycyna KJ, Dwyer ME, Schneck FX, Ost MC, Cannon GM, Stephany HA.The role of prophylactic antibiotics after minimally invasive pyeloplasty with ureteral stent placement in children. Urology,2016,89:107-111. [12]Wu FM, Lim M, Deng Z, Heng CT, Tiong HY.Successful endourological management of the ‘forgotten’ stent in a transplanted kidney.Urol Int,2014,92(3):373-376. [13]Pais VM Jr, Chew B, Shaw O, Hyams ES, Matlaga B, Venkatesh R, Page J, Paterson RF, Arsovska O, Kurtz M, Eisner BH.Percutaneous nephrolithotomy for removal of encrusted ureteral stents: a multicenter study.J Endourol,2014,28(10):1188-1191. [14]Shinnick JK, Short HL, Heiss KF, Santore MT, Blakely ML, Raval MV.Enhancing recovery in pediatric surgery: a review of the literature.J Surg Res,2016,202(1):165-176. [15]Seo IY, Oh TH, Lee JW.Long-term follow-up results of laparoscopic pyeloplasty.Korean J Urol,2014,55(10):656-659. [16]Suda K, Koga H, Okawada M, Doi T, Miyano G, Lane GJ, Yamataka A.The effect of preoperative urinary tract infection on postoperative renal function in prenatally diagnosedureteropelvic junction obstruction: indications for the timing of pyeloplasty.J Pediatr Surg,2015,50(12):2068-2070. (本文编辑:林燕薇) Effect of different insertion technique and indwelling time of urethral catheter on urinary tract infection after pyeloureteroplasty XieQigen,LiZuoqing,XuZhe,SunJunjie,ZhouLi,SuCheng. DepartmentofPediatricSurgery,theFirstAffiliatedHospitalofSunYat-senUniversity,Guangzhou510080,China ,SuCheng,E-mail:sucheng@mail.sysu.edu.cn Objective To evaluate the effect of different catheter insertion technique and indwelling time upon the incidence of urinary tract infection in the children who underwent pyeloureteroplasty. Methods Clinical data of 371 children undergoing pyeloureteroplasty were collected. According to the catheter insertion technique, all participants were divided into double J stent (n=245), external stent (n=103) and stent-less groups (n=23). Based upon postoperative indwelling time, children in the double J stent group were further divided into the A (indwelling time ≤45 d), B (46-105 d) and C subgroups (>105 d). All children were divided into the urinary tract infection (n=126) and non-urinary tract infection groups (n=245). Preoperative clinical data, routine urine examination and urine culture results were obtained. The positive rate of white blood cell in urine, frequency of positive white blood cell in urine, positive rate of urine culture test, percentage of hospitalization treatment, percentage of outpatient treatment, use of antibiotics and long-term success rate of surgery were statistically compared among all groups. Results The urinary tract infection rate before and early after surgery did not significantly differ among the double J stent, external stent and stent-less groups (allP>0.05). After hospital discharge, the percentage of urinary tract infection in the double J stent group wasup to 21.7%, significantly higher compared with 2.1% in the external stent (P<0.01) and 0% in the stent-less groups (P<0.017). In the double J stent group, postoperative frequency of positive white blood cell in urine, percentage of outpatient and hospitalization treatment were all higher compared with those in the external stent group (allP<0.017). Compared with the stent-less group, the frequency of positive white blood cell in urine, positive rate of white blood cell in urine, positive rate of urine culture test and percentage of outpatient treatment were significantly higher in the double J stent group (allP<0.017). In the A subgroup, the positive rate of white blood cell in urine, frequency of positive white blood cell in urine and use of antibiotics after hospital discharge were significantly lower compared with those in the B and C subgroups(allP<0.017). The positive rate of urine culture test and percentage of hospitalization treatment in the A subgroup were considerably lower than those in the B and C subgroups (allP<0.017). The percentage of outpatient treatment in the A and B subgroups was significantly lower compared with that in the C subgroup (bothP<0.017). In the urinary tract infection group, the long-term success rate of success rate was calculated as 89.7%, significantly lower than 96.7% in the non-urinary tract infection group (P<0.01). Conclusions Indwelling of double J stent increases the risk and severity of urinary tract infection. The incidence of urinary tract infection affects the long-term efficacy of hydronephrosis surgery. It is recommended to remove the double J stent at postoperative 1 month. Pyeloureteroplasty; Catheterization; Urinary tract infection 10.3969/j.issn.0253-9802.2016.11.008 510080 广州, 中山大学附属第一医院小儿外科 ,苏诚,E-mail:sucheng@mail.sysu.edu.cn 2016-06-30)对象与方法

结 果

讨 论