Ten years trend in maternal mortality at Kilimanjaro Christian Medical Center Tanzania, 2003 to 2012: A descriptive retrospective tertiary hospital based study
Eusebious W. Maro, Neema R. Mosha, Michael Johnson Mahande, Joseph Obure, Gileard Masenga
1Department of Obstetrics and Gynecology, Kilimanjaro Christian Medical Center, Box 3010 Moshi, Tanzania
2Institute of Public Health, Community Health Department, Kilimanjaro Christian Medical University College, Box 2240 Moshi, Tanzania
Ten years trend in maternal mortality at Kilimanjaro Christian Medical Center Tanzania, 2003 to 2012: A descriptive retrospective tertiary hospital based study
Eusebious W. Maro1*, Neema R. Mosha2, Michael Johnson Mahande2, Joseph Obure1, Gileard Masenga1
1Department of Obstetrics and Gynecology, Kilimanjaro Christian Medical Center, Box 3010 Moshi, Tanzania
2Institute of Public Health, Community Health Department, Kilimanjaro Christian Medical University College, Box 2240 Moshi, Tanzania
ARTICLE INFO
Article history:
Received
Received in revised form Accepted
Available online
Trend
Objective: To determine the trend, causes and characteristics of maternal deaths in a tertiary hospital in northern Tanzania. Methods: A descriptive retrospective review of hospital based maternal death data that occurred at Kilimanjaro Christian Medical Center (KCMC) between the years 2003 to 2012. Descriptive statistics were used to summarize the socio-demographic characteristics, causes and risk factors for maternal deaths using STATA version 12. Yearly maternal mortality ratio was calculated to estimate the trend over years under the review. Results: Between years 2003 to 2012, a total of 34 953 live deliveries and 172 maternal deaths were recorded at KCMC, giving an overall MMR of 492.1/100 000 live deliveries. Direct causes accounted for 107(62.2%) of maternal deaths, indirect causes 49(28.5%) and 16(9.3%) were due to both direct and indirect causes. Hemorrhage was the overall leading cause of maternal death, accounting for 33(19.2%) of mortality, followed by hypertensive disorders in pregnancy 31(18.0%). HIV/ AIDS and heart diseases accounted for 8.7% and 6.4% of maternal deaths, and were the leading causes of indirect maternal deaths by contributing 31% and 22% respectively. Majority 67(38.9%) of deaths were attributed to type II delay followed by type I delay 59(34.3%). Conclusions: Maternal mortality ratio is still very high in northern Tanzania with hemorrhage and hypertensive diseases the major preventable causes of deaths. Eff orts must be made at the community, lower and tertiary health facilities to improve risk detection, management of risk cases to prevent severe forms of diseases and ensure timely referrals.
1. Introduction
Maternal mortality is the main indicator of society’s level of development as well as the proxy indicator of the level of health care delivery system. Every day, approximately 800 women die from complications of pregnancy and childbirth worldwide. Sub-Saharan Africa and South Asia account for 86% of global maternal deaths[1].
Maternal deaths remain a big challenge in most developing countries including Tanzania, although most of these deaths can be averted even in circumstances of resource limited countries. Despite numerous eff orts to reduce its burden, maternal mortality has continued to be a top global agenda. While other regions like Eastern Asia, Southern Asia, and Northern Africa has remarkably reduced maternal mortality ratio (MMR) by 65%, 64%, and 57% respectively between 1990 and 2013, Sub Saharan Africa has reduced MMR by only 49% representing 3.6% decrease in maternal mortality annually. This is far below the 5.5% annual decline rate necessary to achieve the fifth Millennium Development Goal (MDG) which targets reduction of maternal mortality by two-thirds by the year 2015[1]. Now, as we are in 2015, the targeted year for 75% reduction of maternal deaths, the level of maternal mortality in Tanzania is unacceptably high, albeit varying MMR reported by various agencies. Furthermore the reduction rate is unknown.
MMR in Tanzania vary from one reporting organization to another, ranging from 450 to 790 per 100 000 live births[2-4]. However, according to the Tanzania Demographic and Health Survey (TDHS) report of 2010 and WHO report of 2014, the MMR in Tanzania is estimated to be 454 and 410 per 100 000 live births respectively. There is no clear trend whether the country is moving towards or away from the MDG. This calls for further evaluations in terms of progress and interventions.
Maternal mortality is a result of a number of complications that beset pregnant women worldwide. About 73% of all maternal deaths worldwide between 2003 and 2009 were due to direct obstetric causes and deaths due to indirect causes accounted for 27.5% of all deaths. Between 2003 and 2009, hemorrhage, hypertensive disorders, and sepsis were responsible for more than half of maternaldeaths worldwide. The most common direct causes of maternal death are hemorrhage (27.1%), hypertensive disorders (14.0%), and sepsis (10.7%). The rest of deaths were due to abortion 7.9%, embolism 3.2% and all other direct causes of death (9.6%). More than a quarter of deaths were attributable to indirect causes. Indirect causes such as malaria, anemia, HIV/AIDS and cardiovascular disease, complicate pregnancy or are aggravated by it[5].
In Tanzania, most deaths are attributed to obstructed labor, puerperal sepsis, postpartum hemorrhage, complications of unsafe abortion, and preeclampsia[6]. A hospital-based study conducted at Muhimbili National Hospital in Tanzania about a decade ago found that maternal deaths were attributed by eclampsia 23.5%, postpartum hemorrhage, 23.3% and anaemia in pregnancy, 11.3%. Although the current hospital-based data suggest underestimation of MMR, the observed constant maternal mortality risk calls for further strengthening of emergency obstetric care to reduce direct obstetric causes of maternal deaths[4].
The concept of three phases of delay was stated by Deborah Maine in 1991 in fi nding the determinants of maternal deaths in the course of management of pregnancy complications[7]. Type I delay results from failure to seek medical treatment on time, type II delay results from diffi culty in transportation: there may be no ambulance or other transport vehicle available, and roads may be in poor or impassable condition and type III delay occurs when the woman has arrived at the hospital[8]. In Tanzania these delays were found to be of varying degrees in each phase of the delays[9]. At Kilimanjaro Christian Medical Center (KCMC), maternal deaths review from 2000 to 2007, the second delay was also mentioned, although the problem was not specifi cally addressed[10].
Efforts to reduce maternal mortality focusing on several interventions to aff ect the risk factors and causes have been put in place since the MDGs were set. It would be important to assess the trend of causes on maternal mortality over years to help refl ect/ indicate the combined success of whatever has been practiced over years.
Tanzania being one of the countries with higher MMR needs an update of the maternal mortality trends, causes and characteristics from various sources including KCMC being one of its tertiary hospitals. Such statistics will help the Ministry of Health (MoH) and other National and International stakeholders to assess the level of success with the existing interventions and plan forward beyond achieving the MDGs.
Report from this study will contribute to other regional maternal mortality reports within the country and therefore provide the policy makers with essential data needed in the health care planning and priorities.
2. Methods
2.1. Study design
This was a retrospective descriptive hospital based study that utilized all maternal deaths data which occurred at KCMC from January 1, 2003 to December 31, 2012. A total of 34 953 births were recorded during the study period.
2.2. Study setting
The study was conducted at the department of Obstetrics and Gynecology at KCMC, located in Moshi Urban District. KCMC is a zonal consultant, research and teaching hospital which receives pregnant women coming for delivery services from the local community in Kilimanjaro region as well as from the nearby regions in the northern part of Tanzania including Tanga, Arusha and Manyara, as well as neighboring districts in Kenya near the border. The hospital has an average annual delivery of 3 300, of which 33% are cesarean deliveries.
Pregnant women in the active phase of labor are initially monitored in a special room at the antenatal ward before being transferred at the delivery suit once they attain advanced stage of labor. The labor ward has four beds partitioned along the sterile room, with the sterile corridor serving for the extras. There are two operating theaters along the labor ward, used for cesarean section services and other obstetric surgical emergencies. The hospital has four full time obstetricians attending patients and providing medical and residency training in obstetrics and gynecology. The Department of Obstetrics at KCMC serves as a zonal referral center for complicated obstetric patients.
2.3. Data source
Information about maternal deaths was obtained from several sources including the in-patients registers/log books kept in the obstetrics and gynecology wards, labor ward as well as medical and surgical Intensive Care Units (ICU). This was complemented by the hospital birth registry, patients fi les kept within the medical records department and the Tanzania MoH surveillance forms kept within the department.
The MoH surveillance forms are designed to timely record all maternal deaths which occurs at all healthcare centers in the country. In KCMC hospital, this form is usually fi lled by the resident doctor who attended the patient as well as the Zonal Reproductive and Child Health (RCH) coordinator within 48 h of any maternal death. Information collected includes socio-demographic characteristics, maternal disease and complication before and during delivery, complication after delivery and other factors describing the three phases of delays leading to maternal deaths.
Our study included all maternal deaths as defi ned by ICD-10 that occurred at KCMC during the period between January 1, 2003 and December 31, 2012, who were recorded in the patient case records, in-patients recording books (registers) and MoH maternal mortality surveillance forms.
2.4. Study variables
Maternal mortality was the primary outcome variable and was defi ned as the death of a woman while pregnant or within 42 d of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes.
Other secondary variables included sepsis, haemorrhage, eclampsia, obstructed labour, abortion, ectopic pregnancy, anaesthetic complication and pulmonary embolism, maternal medicalconditions, number of antenatal care visits, referral from another facility, booking gestational age, haemoglobin level at last antenatal clinic and mode of delivery. Also demographic characteristics such as maternal age, parity, marital status, level of education, religion and occupation were included for analysis.
2.5. Study procedures
A list of maternal deaths diagnosis with their respective hospital registration numbers were extracted from a combination of hospital birth registry database and registers from antenatal ward, labor and delivery suit, as well as medical and surgical ICU. The list was used to extract fi les from the medical records department. To compliment for the missing data from the fi les, Tanzania MoH maternal mortality surveillance forms were used.
A standardized data collection form was developed and used to extract all relevant information pertaining to study variable from the source documents listed above. The collected information was immediately transferred into a computer data base containing all corresponding variables needed for the study.
2.6. Data processing and analysis
Data were entered into a computer database using Microsoft Excel software and then transferred to STATA version 12 (StataCorp, Texas,USA) for analysis. Data cleaning and error range check to enhance validity and consistency was adhered before data analysis. We used proportion to describe the maternal characteristics and causes of maternal deaths. Yearly MMR was determined by estimating the number of maternal deaths over a total number of live births conducted at KCMC in that particular year. Overall MMR was also calculated as the total number of maternal deaths per 100 000 live deliveries. The assessment of the three types of delay was also done based on the information gathered from the MoH surveillance forms.
2.7. Ethical clearance
The study was approved by Tumaini University College Research Ethical Committee prior to initiation of the study. Privacy and confi dentiality on the information obtained concerning the patients was adhered by using patient hospital registration number instead of their names.
3. Results
3.1. MMR
A total of 34 953 live deliveries and 172 maternal deaths were recorded between January 1, 2003 to December 31 2012 corresponding to overall MMR of 492.1/100 000 live births.
3.2. Maternal mortality trend
A progressive annual decline in MMR was recorded despite the increase in number of deliveries between the years 2003 to 2012. MMR at KCMC was found to decline by an average of 4.5% per year over the study period (Figure 1).
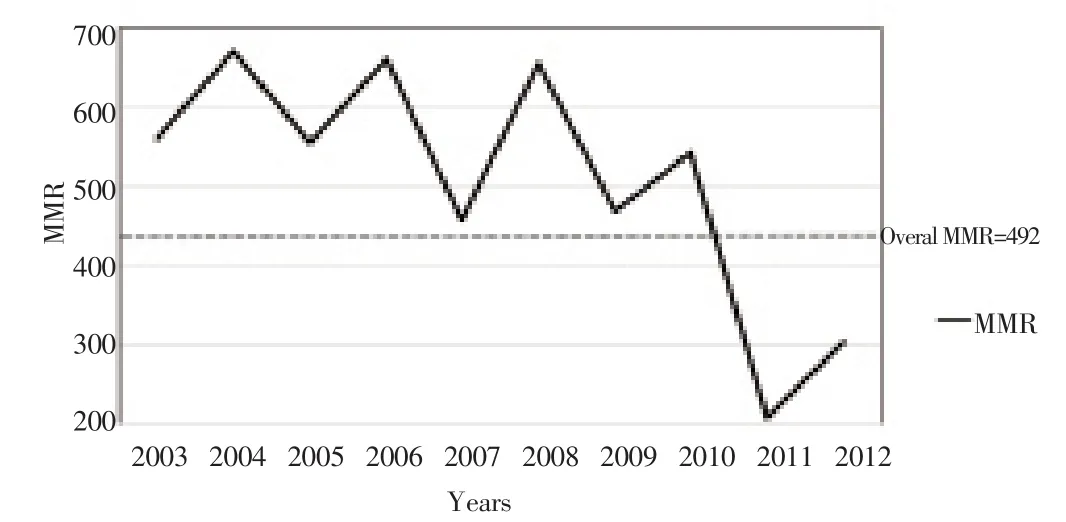
Figure 1. The annual trend of maternal mortality, total number of deliveries and number of midwives at KCMC hospital between the years 2003 and 2012.
3.3. Characteristics of women with maternal deaths
The characteristics of women who encountered maternal deaths are presented on Table 1. The mean age (±SD) in years of women who experienced maternal death was 28.5(±6.8), with the range of 30 years. About 41.9% (72 women) were aged between 25–34 years. More than half (57.6%) of the women who died reported to have no any formal education, while 29.2% had primary education and 5 (3.5%) had tertiary education. The majority (77.3%) were either married or cohabiting. More than half of maternal deaths (52.3%) were coming from rural areas. Most (80.8%) of the maternal deaths occurred among women who were referred from other health facilities.
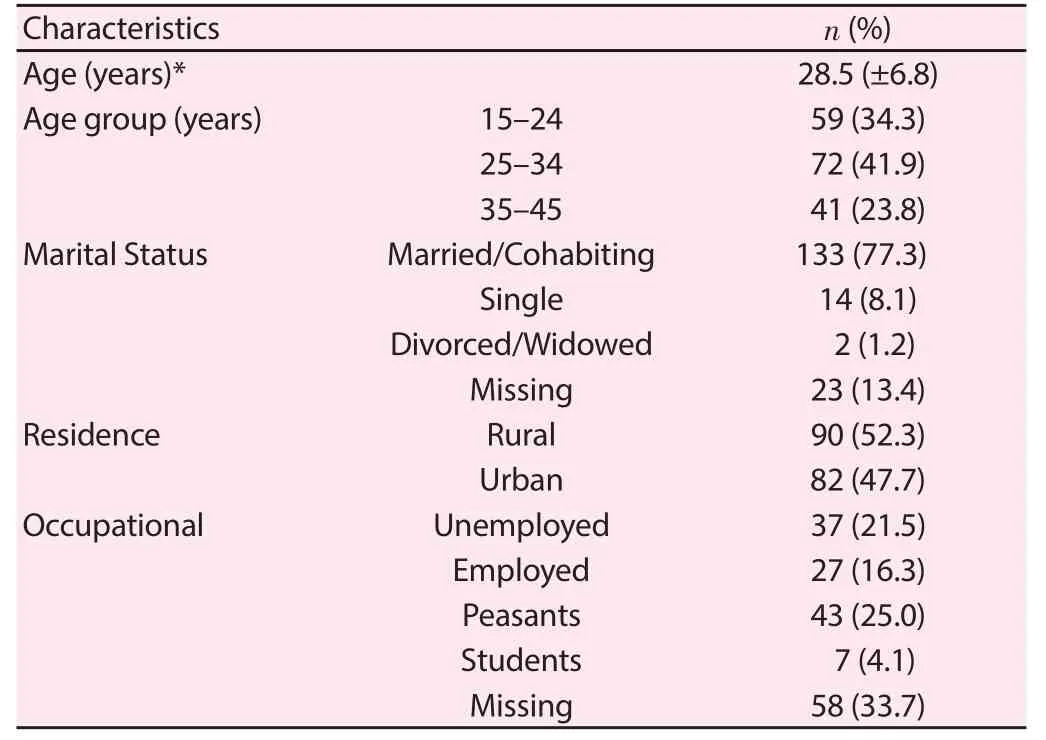
Table 1 Distribution of social-demographic characteristics of maternal mortality at KCMC.
3.4. Obstetric characteristics of women with maternal deaths
The obstetrics characteristics of women who experienced maternal deaths are shown in Table 2. The median (IQR) of gravidity was 3(2–5), out of which the gravidity of 39(22.7%) women could notbe ascertained. Nearly forty percent 67(38.9%) of these women had a parity of 2–4. The mean (±SD) gestational age at the time of maternal deaths was 32.8 (±7.3) weeks and the range of 33 weeks. Over a third of deaths 56(32.6%) occurred among women who had gestational age between 28–36 weeks, while only 14(8.1%) of the deaths were < 28 weeks of gestation age. More than half of women who died (54.1%) had attended ANC at least once.

Table 2 Distribution of obstetrics characteristics of maternal death at KCMC Hospital (n = 172).
A high proportion of deaths (22.7%) occurred after more than 10 d of hospital admission whereas 20.3% occurred within 24 h and 22.2% within 1 week of hospital admission with the median time of hospital stay being 4 d. For the deaths which occurred after more than 24 h in the hospital, the leading cause of deaths were hypertensive diseases (18.1%), followed by HIV in pregnancy (13.9%), sepsis (10.9%), abortion (10.9%), heart diseases (7.2%) and others (14.6%). Among 35(20.3%) deaths that occurred within 24 h, Hemorrhage and sepsis were the leading causes by 8(22.8%) each, followed by hypertensive disorders of pregnancy 5(14.3%). A high proportion of women who died (50.0%) were admitted during antepartum stage (before onset of labor), with majority of birth attendants (37.2%) being doctors. The majority of these deaths (33%) were delivered by cesarean sections.
Table 3 shows the medical causes of all the maternal deaths which occurred at KCMC from 2003 to 2012. Overall, majority 107(62.2%) of maternal deaths were attributed to direct causes. Only 16(9.3%) were due to both direct and indirect causes. Hemorrhage was the overall leading cause of maternal death, accounting for 33(19.2%) of mortality, followed closely by hypertensive disorders in pregnancy 31(18.0%). Other direct causes included sepsis 19(11.0%) and abortion 14(8.1%). HIV/AIDS and heart diseases were the leading indirect causes of maternal deaths contributing to 15(31%) and 11(22%) respectively. Other indirect causes included anemia 7(4.1%) malaria 3(1.7%) and others 12(6.9%).

Table 3 Causes of maternal death at KCMC Hospital (2003–2012).
When assessing the types of delays associated with maternal deaths (Table 4), the analysis showed that 5.9% of the deaths had no delays. Majority of deaths 67(38.9%) were attributed to type II delay, which were due to late referral from another facility 63(36.6%) and poor infrastructure 4(6%). Type I delay was responsible for 59(34.3%) maternal deaths and these were reported to be due to lack of resources in the family 18(10.5%) and delay in decision making at the family level in 41(23.8%) of deaths. Type III delay was shown to be responsible for 36(20.0%) maternal deaths, whereby 14(8.1%) deaths were due to delay in receiving treatment in the health facility, 12(7.0%) due to lack of supplies and equipments at health facility, 9(5.2%) due to inadequate provider’s skills and 1(0.6%) was due to inadequate staff . Table 4 shows the distribution of maternal deaths at KCMC according to the three types of delays between 2003 through 2012.
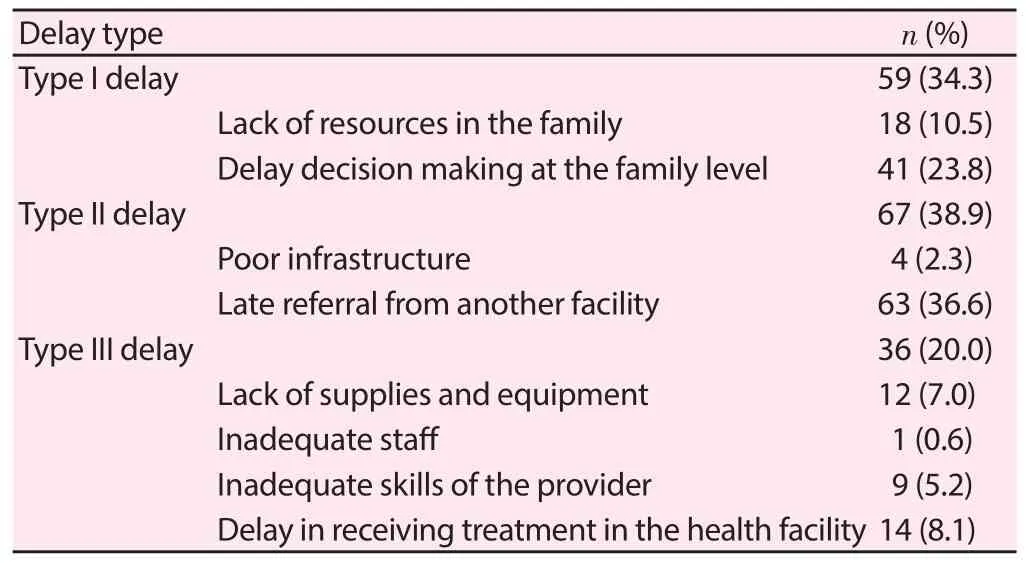
Table 4 Distribution of maternal deaths at KCMC according to the three types of delays between 2003 and 2012.
4. Discussion
This study found a combined MMR of 492.7 per 100 000 following a 10 years (2003–2012) review. The MMR seen in this study is relatively lower compared to the other review done at the Tanzanian National Referral Hospital conducted 8 years ago with a MMR of 512/100 000 live births[4]. In addition, MMR reported in our review is however higher than a study report of data collected from four hospitals in Dar es Salaam, Tanzania, which found maternal deaths to be 218/ 100 000 live births[11].
Overall, similar high MMR was also found in other studies done in tertiary referral hospitals in developing countries in Kenya and Nigeria, which reported MMR of 426/100 000 live births and 1 513.4/100 000 live births respectively[12,13]. The relatively lower MMR at KCMC compared to Muhimbili National Hospital in Tanzania, could be attributed to the general improvement in maternal health services made during the time interval between the two studies. A study at the National hospital included the data from the year 1999 to 2005 while our study included data from 2002 to 2012. As well the higher MMR at KCMC compared to four hospital study conducted in Dar es Salaam could be attributed to diff erential access to maternal health services between Moshi, Kilimanjaro which is a small city compared to Dar es Salaam, the largest, most populated commercial city in Tanzania. The four urban hospitals in Dar es Salaam provides an increased access to immediate emergency services as well as treatment of complicated cases due to relatively adequate skilled birth attendants compared to the limited access and availability of skilled attendants in Kilimanjaro region. In addition, the presence of Muhimbili national hospital in Dar es Salaam could mean that most complicated maternal cases from Dar es Salaam hospitals are easily referred to Muhimbili leading to a higher MMR at Muhimbili and lower MMR at the Dar es Salaam hospitals.
As expected, MMR at KCMC is higher than the national MMR[1,14], and this is partly attributed to the fact that KCMC is a referral hospital attending complicated cases compared to the national reported population surveys with mixed causes and degree of complications as it relates to the maternal deaths.
Despite the increase in number of deliveries conducted at KCMC over period of time, MMR gradually declined over years, suggesting the improved knowledge and skills of providers in managing emergence obstetric cases in an environment of limited human resource availability.
In our study, 62.2% of deaths were due to direct causes while 28.5% were contributed by indirect causes. This is in agreement with other hospital-based and community-based studies done in Tanzania and other African countries[4,11,13,15-17]. Furthermore, hemorrhage was the leading cause of maternal deaths by 19.2% followed closely by hypertensive disorders in pregnancy which contributed 18%. Similar fi ndings were observed in studies done within the country and most of African countries[12,15], however this was not the case for many studies done in developed countries and even from the previous study done in Muhimbili National Hospital in Dar es Salaam[4] where hypertensive disorders in pregnancy was the leading cause of maternal deaths. This shows that more eff orts should be put on the implementation of the evidence-based methods of preventing and managing these two leading obstetrics emergencies in order to reduce deaths due to direct causes.
Forty-nine deaths (28.5%) were due to indirect causes whereby 15(8.7%) of them were HIV/AIDS associated maternal deaths, followed by 11(6.4%) deaths due to heart diseases in pregnancy. These fi ndings are similar to another study conducted in Tanzania[15]. The findings show maternal HIV is still a challenge in the efforts to reduce maternal deaths. This underscores the need to scale up the use of lifelong ART to all HIV positive pregnant and lactating women. In addition, improving family planning services to women living with HIV is paramount to prevent unintended pregnancies or planning pregnancies in favorable healthy conditions. Anemia and malaria are other preventable conditions which contributed to 5.8% indirect maternal deaths at KCMC hospital. This was also reported in a research done in one of the Teaching University Hospital in Ghana[18].
In this review, the mean age of maternal deaths was 28.5(6.8), with 12.8% of deaths occurring among women below 20 years of age. A high proportion (41.9%) of women who died were in the age group of 25–35 years, and were multigravid (50.4%). These fi ndings correspond to other studies done in Tanzania and other African settings[4,12,15,16,18].
About 80.2% of the maternal deaths at KCMC occurred among patients referred from other districts hospitals. These results are similar to other study reports conducted in Africa[12,13,18]. In addition, the results confi rm the status of KCMC as a referral and consultant zonal hospital in Tanzania. More deaths (50%) occurred among women who presented to the hospital during antepartum. This could indicate the magnitude of complicated patients referred at KCMC who eventually succumb to deaths despite eff orts to provide quality appropriate and adequate care.
Of the women who died, most of them 57.6% had not received formal education. The fi ndings correspond with other study done in Tanzania which showed an increased risk of maternal death among illiterate women[19]. Similar results were also reported in Kenya[14]. This shows the role of education in increasing access to health information and services as well as in making appropriate health decisions.
Type II delay accounted for the most of (38.9%) maternal deaths at KCMC hospital. The main reasons attributed to this delay were late referral from another lower health facility and poor infrastructure. In fact, late referral from another lower facility (36.6%) and delay in decision making at the family level (23.3%) were reported as the main reasons for most of the delays. This shows the need to enhance capacity of provider’s to improve risk detection threshold, provide appropriate management and provision of timely referrals to eligible patients. In addition, strengthening capacity of individual familiesfor birth preparedness, health facilities and community systems to facilitate transportation of women referred to higher level facilities for the advance care.
In addition, type III delay contributed to about 20.9% of maternal deaths at KCMC. Our findings are less than what was reported in previous study in Nigeria[13]. The major reasons reported for this delay were delay in the diagnosis and lack of supplies and equipments needed for emergency interventions such as blood for transfusion at both levels of health facilities including KCMC. This shows the limited health service delivery at facility level as it relates to skilled birth attendants, supplies and infrastructure challenges. Some study participants had missing information from their records which may have accounted to elimination from the analysis or misclassifi cation bias. However, the use of MoH maternal mortality surveillance forms that are filled within 48 h of maternal deaths ensured the study captures most of the needed information and reduced the recall and misclassifi cation bias.
Hospital based study provide little representation of what is happening in the community and therefore may lead to underreporting, however a big sample size of over 10 years period provided quick, timely and cause specific trends of maternal mortality. In addition, the sample may not represent the general population as patients seen at KCMC are either self-referral or formally refereed. KCMC being a consultant and referral hospital means many complicated obstetric cases would be referred to the center hence leading to selection bias and lack of generalizability. This may however help answer the study questions as maternal deaths are mostly related to some complications and KCMC provide better catchment areas for such cases.
A descriptive study with cases only and lack of comparison group cannot provide the causative factors for maternal deaths. Lastly it was diffi cult to ascertain community factors which contributed to the delays in seeking health care.
MMR is still very high in Tanzania, with preventable causes such as hemorrhage and hypertension being the major causes. HIV/AIDS associated maternal deaths were also signifi cantly prevalent in this cohort.
Eff orts must be made to improve the management of hemorrhage and hypertension at the level of both health facility and the community where most of these deaths are referred from. Building capacity and systems at the family and community level is important to facilitate referrals of pregnant women eligible for advanced care. The national rollout of Option B plus (Life Long ART for HIV positive pregnant and lactating women) should continue with anticipated benefi t of keeping mothers alive.
Declare of interest statement
The authors declare that they have no competing interests.
Acknowledgments
We would like to thank the Departments of Obstetrics and Gynecology and Community Health at Kilimanjaro Christian Medical Center to enable this study to be done. Moreover, we are indebted to all women whose information was utilized in this study, without them this study couldn’t have been done.
[1] World Health Organization. Trends in maternal mortality: 1990 to 2013. Estimates by WHO, UNICEF, UNFPA. The World Bank and the United Nations Population Division. Geneva: WHO; 2014.
[2] UNICEF (2007, 11 June 2003). Progress for Children-Maternal Mortality. A World Fit for Children Statistical Review. Available from: http://www.unicef.org/progressforchildren/2007n6/index_41855.htm. [Accessed in August, 2013].
[3] World Bank. Millennium Development Goals. (2008). Available from: http://www.developmentgoals.org/. [Accessed in Feb, 2009).
[4] Kazaura M, Kidanto H Massawe S. Maternal mortality at Muhimbili National Hospital, Tanzania, 1999–2005: Levels, causes and characteristics. East Afr J Public Health 2006; 3(2): 23-25.
[5] Lale Say, Doris Chou, Alison G, Özge T, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Global Health 2014; 2(6): e323-e333.
[6] Walraven G, Mkanje R, van Roosmalen J, van Dongen P, Dolmans W. Assessment of maternal mortality in Tanzania. Br J Obstetr Gynaecol 1994; 101(5): 414-417.
[7] Maine D. Safe motherhood progress, options and issues. New York: Columbia University Center for Population and Family Health; 1991.
[8] Ransom EK, Yinger NV. Making motherhood safer: Overcoming obstacles on the pathway of care. Washington: Population Reference Bureau; 2002: 1-36.
[9] Mbaruku G, van Roosmalen J, Kamugisha C, Nturugelewa E, Bergström S. Perceptions of obstetric risk among health staff, traditional birth attendants and community members in rural Tanzania. Paper III. In: Mbaruku G, editor. Enhancing survival of mothers and their newborns in Tanzania. Doctoral thesis. Karolinska University Press, Stockholm; 2005. [10] Bergsjø P, Vangen S, Lie RT, Lyatuu R, Lie-Nielsen E, Oneko O. Recording of maternal deaths in an East African university hospital. Acta Obstetr Gynecolog 2010; 89: 789-793.
[11] Nyamtema A, Urassa D, Roosmalen J. Maternal health interventions in resource limited countries: a systematic review of packages, impacts and factors for change. BMC Pregnancy Childbirth 2011; 11: 30.
[12] Yego F, Williams JS, Byles J, Nyongesa P, Aruasa W, D’Este C. A retrospective analysis of maternal and neonatal mortality at a teaching and referral hospital in Kenya. BMC Reprod Health 2013; 10: 13.
[13] TU Agan, EI Archibong, JE Ekabua, EI Ekanem, SE Abeshi, TA Edentekhe, et al. Trends in maternal mortality at the University of Calabar Teaching Hospital, Nigeria, 1999–2009. Int J Womens Health 2010; 2: 249-254.
[14] National Bureau of Statistics (NBS) [Tanzania], ICF Macro. Tanzania Demographic and Health Survey 2014. Dar es Salaam, Tanzania: NBS and ICF Macro. 2014. Available from: http://www.nbs.go.tz/. [Accessed in Jan, 2014].
[15] Evance I, Mbaruku G, Masanja H, Kahn K. Causes and risk factors for maternal mortality in rural Tanzania - Case of Rufiji Health and Demographic Surveillance Site (HDSS). Afr J Reprod Health 2013; 17(3): 119-130.
[16] Nelissen JT, Mduma E, Ersdal H, Evjen-Olsen B, Roosmalen J, Stekelenburg J. Maternal near miss and mortality in a rural referral hospital in northern Tanzania: a cross-sectional study. BMC Pregnancy Childbirth 2013; 13: 141.
[17] Yego F, D’Este C, Byles J, Williams JS, Nyongesa P. Risk factors for maternal mortality in a Tertiary Hospital in Kenya: a case control study. BMC Pregnancy Childbirth 2014; 14: 38.
[18] SK Gumanga, DZ Kolbila, BBN Gandau, A Munkaila, H Malechi, K Kyei-Aboagye. Trends in maternal mortality in Tamale Teaching Hospital, Ghana. Ghana Med J 2011; 45(3): 105-110.
[19] Evjen-Olsen B, Hinderaker S, Lie R, Bergsjø P, Gasheka P, Kvåle G. Risk factors for maternal death in the highlands of rural northern Tanzania: a case-control study. BioMed Central Public Health 2008; 8: 52.
ent heading
10.1016/j.apjr.2016.04.012
*Corresponding author: Eusebious W. Maro, MD, Department of Obstetrics and Gynecology, Kilimanjaro Christian Medical Center, Box 3010 Moshi, Tanzania.
E-mail: sebiwilly@gmail.com
Maternal mortality ratio Tanzania
 Asian Pacific Journal of Reproduction2016年3期
Asian Pacific Journal of Reproduction2016年3期
- Asian Pacific Journal of Reproduction的其它文章
- A rare cause of infertility: A late complication of female genital mutilation
- Corpus callosum agenesis: Role of fetal magnetic resonance imaging
- Chilled and post-thawed semen characteristics of buffalo semen diluted in tris extender enriched with date palm pollen grains (TPG)
- Establishment, characterization and cryopreservation of Fars native goat fetal fibroblast cell lines
- Somatic embryogenesis and in vitro flowering in Hybanthus enneaspermus (L.) F. Muell.-a rare multipotent herb
- Pollutant exposure in Manila Bay: Effects on the allometry and histological structures of Perna viridis (Linn.)
