儿童胫骨近端局灶性纤维软骨发育不良6例影像表现
黎芳丽,肖怀春,李春旺,伍光春,金 科
(南华大学儿科学院,湖南省儿童医院,长沙 410007)
儿童胫骨近端局灶性纤维软骨发育不良6例影像表现
黎芳丽,肖怀春,李春旺,伍光春,金 科
(南华大学儿科学院,湖南省儿童医院,长沙 410007)
目的:探讨儿童胫骨近端局灶性纤维软骨发育不良(Focal Fibrocartilagions Dysplasia,FFCD)的影像表现。方法:6例经手术病理证实为FFCD,对X线及MRI表现进行分析,总结FFCD的X线及MRI特点。6例病例中,男性5例,女性1例,4例位于左侧胫骨近段干骺端内侧,2例位于左侧胫骨近段干骺端内侧。结果:6例患儿X线均表现为患侧胫骨近端呈内翻改变,内侧骨皮质局部凹陷,可见条带状斜行透亮区,边界清晰,内侧骨质均可见明显硬化。在MRI上表现,6例患儿表现为胫骨近端条带状异常信号影,T1WI呈低信号,T2WI呈低信号,边界清晰,与X线上骨质缺损区对应;胫骨内侧可见带状长T1中等T2信号,与X线上骨质硬化对应;其中2例病变周围骨髓出现水肿。3例行增强扫描患儿病变未见强化。结论:FFCD是罕见的良性病变,以儿童多见,病变部位主要位于长骨,尤其是胫骨近端干骺端内侧,FFCD在X线及MRI上具有特征性,依据这些特点可作出较准确的诊断。
儿童;胫骨;局灶性纤维软骨发育不良;影像表现
儿童骨骼局灶性纤维软骨发育不良是一种罕见良性病变,多发生于儿童,病变主要发生于长骨,尤其是胫骨近端,也可累及股骨、尺骨等其它长骨。目前,国内关于FFCD病例报道仅5例[1,2],放射科医师对其影像特点认识不足,容易误诊。本文总结我院6例胫骨近端FFCD病例,分析其影像特点,以提高对本病的认识。
1 资料与方法
1.1 一般资料 回顾性分析2010~2014年期间本院经手术病理证实的6例FFCD患儿的临床资料和影像表现。本组病例6例中男性5例,女性1例,4例位于左侧胫骨近段干骺端内侧,2例位于左侧胫骨近段干骺端内侧。年龄1岁~3岁1月,平均年龄2.2岁。临床主要表现为步态异常及患侧小腿内翻畸形,伴患肢缩短(3例)。体查患肢未扪及明显包块,无压痛,未触及假关节活动,肢端血运、感觉良好。6例患儿出生情况均正常,无产伤史及外伤史。6例患儿实验室检查血常规、凝血全套、电解质、肝肾功能、乙肝病毒表面抗原均正常。
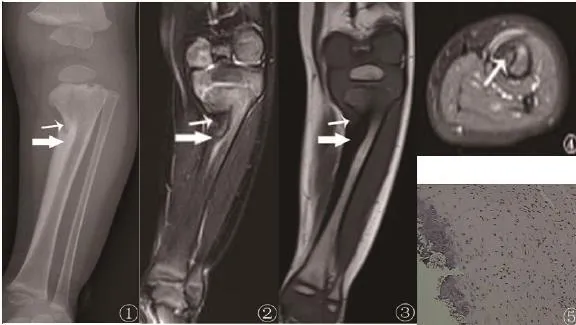
图1~5男,3岁1月,左下肢内翻畸形1年余。图1 X线正位示胫骨近端呈内翻改变,干骺端内侧骨皮质局部凹陷,可见条带状斜行透亮区(细箭),边界清晰,内侧骨质可见明显硬化(粗箭);图2 MR冠状位T2WI抑脂示胫骨近端内侧可见条带状稍低信号(细箭),胫骨内侧呈低信号改变(粗箭);图3MR冠状位T1WI示胫骨近端内侧可见条带状稍低信号(细箭),胫骨内侧呈低信号改变(粗箭);图4 MR轴位T1WI抑脂增强示条带状异常信号灶无强化;图5(HEx100)镜下可见大量纤维组织增生、玻璃样变,另可见区域小灶性软骨细胞灶。
1.2 仪器与方法 6例均行X线及MRI扫描。X线检查使用Siemens(DR机)摄胫骨正侧位平片。MRI扫描使用Siemens 1.5T Avanto MR 扫描仪,体部线圈。本组病例属于回顾性分析,扫描序列及参数因技术员未完全统一,但均同时采集轴位、冠状位及矢状位图像,以T1WI、T2WI及抑脂序列为主,其中3例行MRI增强扫描。扫描范围覆盖患侧胫骨及骨骺。
2 结果
2.1 影像表现 6例患儿X线均表现为患侧胫骨近端内侧呈内翻改变,内侧骨皮质局部凹陷,可见条带状斜行透亮区,边界清晰,内侧骨质可见明显硬化;邻近骨皮质旁未见骨膜反应(图1~5)。6例患儿MRI均表现为胫骨近端呈内翻改变,可见条带状异常信号影,T1WI呈低信号,T2WI呈低至稍高信号,边界清晰;内侧骨皮质增厚,T1WI、T2WI及抑脂上均呈低信号;周围软组织间隙清晰,未见软组织肿块;其中2例病变周围骨髓出现水肿。3例行增强扫描患儿病变未见强化。
2.2 病理结果 光镜下示6例病变组织内均见较多纤维组织增生,部分纤维组织有玻变及黏液样变,未见异型性细胞。3例镜下可见小灶性软骨组织(图5),余3例未见软骨组织(图10)。
3 讨论
3.1 概述 FFCD是罕见的良性骨病变,本病由Bell等[3]于1985年首次命名。至今FFCD发病机制仍未阐明,主要包括以下三种学说:间充质细胞原基的分化障碍[3]产伤或者某种未知的创伤后的不完全修复,从而导致骺板远端骨质的特征性缺损[4]异常的肌腱或纤维束带栓系于干骺端,阻碍了骨膜的自然滑动,从而导致长骨畸形,如果纤维束带断裂,畸形则会自然矫正[5,6]。目前,第三种学说被国外学者广泛认可。FFCD好发于长骨,尤其是胫骨,其次是股骨、尺骨,肱骨、桡骨、指骨(趾骨)等亦可累及[4],以儿童多见,男女发病1:1,双侧发病1:1,双侧均累及罕见,以13月~24月(学步期)发病为主[7]。临床表现主要包括单侧肢体成角畸形,肢体缩短;由于下肢承重,畸形可随年龄加重;病变位于上肢时,发病较晚[6,8]。据文献报道约45%胫骨近端FFCD可自愈[4,5,9]。
3.2 病理基础及影像特点 尽管FFCD是罕见的良性病变,但病理表现变化多样,可从良性纤维软骨组织演变为致密纤维肌腱组织[5]。大体病理上可见纤维结缔组织卡压在骨皮质缺损区上。镜下可表现为致密纤维组织、纤维软骨、透明软骨或其混合成份。文献报道部分FFCD患者病理上只表现为致密纤维组织,可没有软骨成份[10]。因此,软骨成份并非是诊断FFCD的必要条件[11]。Gottschalk等[12]认为FFCD病理分型根据软骨成份有无至少分为两类:有软骨成份及无软骨成份。本组病例中,3例镜下可见小灶性软骨组织,3例未见软骨组织。
FFCD的主要病变是束带状致密纤维组织,因此影像上具有明显的特征性。X线是FFCD的首选影像检查方法。X线诊断要点如下: 病变主要发生在胫骨近端干骺端内侧 骨质缺损透亮区 呈斜行走形,边界清晰病变侧骨质硬化[6,13]。 Nakase和Herman 等报道FFCD患儿在X线上病变周围可见骨膜反应[14,15]。MRI检查能对纤维组织、纤维软骨及其混合病变定性,而CT难于区分纤维组织及邻近肌肉组织。因此,MRI对于FFCD的诊断及鉴别诊断更优于CT。国外报道大部分FFCD患者主要以X线及MRI检查为主。本组病例均未行CT检查。在MRI,FFCD主要表现为条带状长T1 短T2信号,与X线上的骨质缺损区对应,骨质硬化区亦呈长T1(稍)短T2信号,周围软组织间隙清晰,无软组织肿块形成[7,8,16]。本组6例X线及MRI表现与文献报道基本一致。鉴于FFCD影像表现极具特征性,Jibri等[9]认为FFCD诊断并不一定需要病理检查。
3.3 鉴别诊断 先天性发育畸形:Blount’s病主要表现胫骨近端骨骺部成角呈鸟嘴状改变,胫骨长轴内收[17]。先天性胫骨假关节的主要特点是胫骨中下段向前外侧弯成角畸形,两骨端变尖并硬化,患肢缩短。约55%胫骨假关节患者合并神经纤维瘤病I型[18]。
骨肿瘤与肿瘤样病变:鉴别诊断包括纤维瘤病、骨纤维结构不良、Ollier’s 病、嗜酸性肉芽肿等[12]。这些病变常伴有软组织肿块,长骨畸形少见。嗜酸性肉芽肿免疫组化S-100为阳性。
代谢性骨病:如佝偻病常累及全身骨骼,FFCD易与其鉴别。
创伤后遗改变及感染:创伤后遗改变及感染在临床上常有典型的病史。
总之,FFCD是罕见的良性骨病变,多见于儿童,临床缺乏特异性,而其在X线及MRI上极具有特征性,放射科医师认识并熟悉这些征象,有助于作出正确诊断,指导临床治疗。
[1] 梅海波, 赫荣国, 朱光辉, 等. 儿童骨骼局灶性纤维软骨发育不良的诊断与治疗, 中华医学会第八次全国小儿外科学术会[J].2010: 1.
[2] 赵静品, 刘彤颜, 崔建岭, 等. 局灶性纤维软骨发育不良一例报告[J]. 医学影像学杂志, 1996 : 181-182.
[3] Bell SN, Campbell PE, Cole WG, et al. Tibia vara caused by focal fibrocartilaginous dysplasia. Three case reports[J]. J Bone Joint Surg Br. 1985 Nov;67(5):780-4.
[4] Jouve JL, Kohler R, Mubarak SJ, et al. Focal fibrocartilaginous dysplasia ("fibrous periosteal inclusion"): an additional series of eleven cases and literature review[J]. J Pediatr Orthop. 2007 Jan-Feb; 27(1): 75-84.
[5] Choi IH, Kim CJ, Cho TJ, et al. Focal fibrocartilaginous dysplasia of long bones: report of eight additional cases and literature review[J]. J Pediatr Orthop. 2000 Jul-Aug; 20(4): 421-7.
[6] Ando A, Hatori M, Hosaka M, et al A patient with focal fibrocartilaginous dysplasia in the distal femur and review of the literature[J]. Tohoku J Exp Med. 2008 Aug; 215(4): 307-12.
[7] Vanhoenacker FM, Gielen JL, Vandervliet E, et al. Focal fibrocartilaginous dysplasia[J]. JBR-BTR. 2008 Mar-Apr; 91(2): 67.
[8] Eren A, Cakar M, Erol B, et al. Focal fibrocartilaginous dysplasia in the humerus[J]. J Pediatr Orthop B. 2008 May; 17(3): 148-51.
[9] Jibri Z, Chakraverty J, Thomas P, et al. Focal fibrocartilaginous dysplasia and spontaneously resolving bowing of the leg[J]. J Pediatr. 2013 Nov; 163(5): 1527.
[10] Santos M, Valente E, Almada A, et al. Tibia valga due to focal fibrocartilaginous dysplasia: case report[J]. J Pediatr Orthop B. 2002 Apr; 11(2): 167-71.
[11] Kim CJ, Choi IH, Cho TJ, et al. The histological spectrum of subperiosteal fibrocartilaginous pseudotumor of long bone (focal fibrocartilaginous dysplasia)[J]. Pathol Int. 1999 Nov; 49(11): 1000-6.
[12] Gottschalk HP, Light TR, Smith P. Focal fibrocartilaginous dysplasia in the ulna: report on 3 cases[J]. J Hand Surg Am. 2012 Nov; 37(11):2300-3.
[13] Rodríguez P, Parra ML, Miralles M, et al. Unilateral femoral deformity due to a focal fibrous tether[J]. Eur Radiol. 1998; 8(4): 603-5.
[14] Nakase T, Yasui N, Araki N, et al. Florid periosteal reaction and focal fibrocartilaginous dysplasia. [J]. Skeletal Radiol. 1998 Nov; 27(11):646-9.
[15] Herman TE, Siegel MJ, McAlister WH. Focal fibrocartilaginous dysplasia associated with tibia vara[J]. Radiology. 1990 Dec; 177(3):767-8.
[16] Meyer JS, Davidson RS, Hubbard AM, et al. MRI of focal fibrocartilaginous dysplasia[J]. J Pediatr Orthop. 1995 May-Jun; 15(3):304-6.
[17] Ruchelsman DE, Madan SS, Feldman DS. Genu valgum secondary to focal fibrocartilaginous dysplasia of the distal femur[J]. J Pediatr Orthop. 2004 Jul-Aug; 24(4): 408-13.
[18] Pannier S. Congenital pseudarthrosis of the tibia[J]. Orthop Traumatol Surg Res. 2011 Nov; 97(7): 750-61.
Imaging characteristics of focal fibrocartilaginous dysplasia in young children with tibia vara
Li Fang-li, Gao Hui, Xiao Huai-chun, Li Chun-wang, Wu Guang-chun, Jin Ke
(Academy of Pediatrics,University of South China Changsha 410007,China, Children's Hospital of Hunan Province Medical Image Center,Changsha 410000 China)
Objective To explore the imaging characteristics of focal fibrocartilaginous dysplasia in young child with tibia vara. Methods Analyze the X-ray and MRI images of 6 cases which were confirmed as focal fibrocartilaginous dysplasia by surgery and pathology. The medical imaging features of focal fibrocartilaginous dysplasia were summarized. In the total 6 cases (including male=5, female=1), 3 of them occurred in the left tibia, another 3 cases occurred in the right tibia. FFCD occurred on the left tibia. Results Radiographically, these lesions were characterized by a well-defined lucent defect in the 6 cases, there was sclerosis along the lateral border of the lesion, and superior-medially, there was an absent bone margin. The MRI findings were virtually identical in all cases. Areas corresponding to the cortical lucency on plain films were hypointense on T1WI and T2WI, while the areas corresponding to the distal sclerosis were hypointense on T1WI and intermediate on T2WI without enhancement. 2 cases appeared the marrow edema surrounding the lesions. Conclusion Focal fibrocartilaginous dysplasia is an uncommon, benign bone lesion that caused deformity of the tibia in young children. However, Focal fibrocartilaginous dysplasia can be diagnosed accurately based on the typical features displayed on X-ray and MRI.
Children; Tibia; Focal fibrocartilaginous dysplasia; Imaging characteristics
R726.8
A
1673-016X(2016)02-0023-03
2015-08-20
湖南省科技计划项目基金资助项目(2014RS4012)
金科 ,E-mail:jinke001@sina.com

