支气管镜介导标本对儿童结核病诊断价值的系统评价和Meta分析
付文龙 张娟娟 代继宏
·论著·
支气管镜介导标本对儿童结核病诊断价值的系统评价和Meta分析
付文龙1,2张娟娟1代继宏2
目的定量评估支气管镜介导标本对儿童结核病(TB)的诊断价值。方法 检索PubMed、EMBASE、Ovid、Cochrane图书馆、中国生物医学文献数据库、中国知网和万方数据库,检索起止时间为建库至2016年2月,并回溯纳入文献的参考文献。2名研究者根据纳入与排除标准筛选文献,采用QUADAS-2量表行文献偏倚风险评估。以临床诊断和实验室诊断作为TB诊断的金标准,评估支气管镜介导标本(支气管肺泡灌洗液、支气管黏膜组织及支气管黏膜刷检)及不同检测方法诊断儿童TB的敏感度和特异度,并以胃液作为对照标本。采用Meta-Disc 1.4软件进行Meta分析,建立汇总受试者工作特征(SROC)曲线,并计算曲线下面积 (AUC)等。采用Stata 12.0软件绘制Deek′s漏斗图评估发表偏倚。结果14篇文献进入Meta分析,纳入2 781份(1 082例患儿)的支气管镜介导标本。①14篇文献报道了支气管镜介导所有标本对儿童TB的诊断,汇总敏感度和特异度分别为0.38(95%CI:0.35~0.41)和1.00(95%CI:0.99~1.00);按照标本及检测方法行亚组分析,支气管黏膜组织活检的敏感度为0.51(95%CI:0.40~0.61),特异度为1.00(95%CI:0.81~1.00);支气管肺泡灌洗液培养、涂片和PCR的敏感度分别为0.36(95%CI:0.32~0.40)、0.21(95%CI:0.15~0.28)和0.58(95%CI:0.46~0.69),特异度分别为1.00(95%CI:0.99~1.00)、1.00(95%CI:0.98~1.00)和1.00(95%CI:0.84~1.00)。②10篇文献报道胃液对儿童TB的诊断,胃液培养敏感度为0.52(95%CI:0.47~0.57),特异度为1.00(95%CI:0.98~1.00);涂片敏感度为0.25(95%CI:0.16~0.36),特异度为1.00(95%CI:0.95~1.00)。③支气管肺泡灌洗液所有检测方法诊断TB的SROC AUC为0.883 9;胃液所有检测方法诊断TB的SROC AUC为0.873 7。④支气管肺泡灌洗液培养、涂片和胃液诊断TB文献的Deeks′检验P分别为0.005、0.014和0.147。结论支气管镜介导的标本对儿童TB的诊断价值是肯定的,但支气管肺泡灌洗液作为最常用的标本采用培养和涂片对TB诊断的敏感度不优于胃液。
支气管镜;儿童;结核病;诊断价值;敏感度;特异度;系统评价;Meta分析
AbstractObjectiveTo systematically evaluate the diagnostic value of specimens via bronchoscopy for tuberculosis(TB) detection in children.MethodsThe PubMed,EMBASE, Ovid, Cochrane Library, CBM, CNKI and Wanfang database were systematically searched up to February 2016, and relevant references were manual screened. Two reviewers independently screened literatures according to the inclusion and exclusion criteria and extracted data, and assessed the risk of bias of included studies by QUADAS-2 tool. The sensitivity and specificity of test methods and specimens (bronchoalveolar lavage, bronchial brushing and tissue biopsy) via bronchoscopy were evaluated by gold standard(clinical and laboratory diagnosis). Meta-analysis was performed using Meta-Disc 1.4 software, and summary receiver operating characteristic curve (SROC) was drawn and area under the curve (AUC) and Q index were calculated. Deek′s funnel plots were drawn using Stata 12.0 software.ResultsA total of 14 studies were included involving 2 781 specimens (1 082 patients). ①Fourteen literatures reported bronchoscopy for the diagnosis of TB. The pooled sensitivity and specificity of bronchoscopy for tuberculosis detection were 0.38(95%CI:0.35-0.41)and 1.00(95%CI:0.99-1.00), respectively. Then subgroup analysis was made by the types of specimens and test methods. The pooled sensitivity and specificity of tissue biopsy were 0.51(95%CI:0.40-0.61)and 1.00(95%CI:0.81-1.00) , respectively; The pooled sensitivity and specificity of culture, acid fast bacilli on smear and PCR for bronchoalveolar lavage were 0.36(95%CI:0.32-0.40)vs1.00(95%CI:0.99-1.00), 0.21(95%CI:0.15-0.28)vs1.00(95%:0.98-1.00)and 0.58(95%CI:0.46-0.69)vs1.00(95%CI:0.84-1.00), respectively. ②Ten literatures reported gastric lavage for the diagnosis of tuberculosis, which exhibited heterogeneity(I2=93.3%). The pooled sensitivity and specificity of gastric lavage for tuberculosis detection were 0.45(95%CI:0.40-0.49)and 1.00(95%CI:0.99-1.00), respectively. The pooled sensitivity and specificity of smear for gastric lavage were 0.52(95%CI:0.47-0.57)and 1.00(95%CI:0.98-1.00), respectively. ③The SROC AUC of bronchoalveolar lavage and gastric lavage were 0.883 9 and 0.873 7, respectively; ④Pvalues of the Deek′s test of culture and smear for bronchoalveolar lavage were 0.005 and 0.014.Pvalue of the Deek′s test of gastric lavage was 0.147.ConclusionThe value of bronchoscopy for the diagnosis of tuberculosis was definitive in children. Bronchoalveolar lavage for bronchoscopy was the most common specimen, but in terms of culture and smear, it wasn′t better than gastric lavage for tuberculosis detection.
儿童是结核病(TB)高危人群,近年发病率有增高的趋势[1~3]。据WHO统计,每年有53万~100万儿童诊断为TB,每年有13.6万儿童死于TB,至少占全球疾病负担的6%[4~7]。 由于儿童TB临床表现多样且不典型,排菌量少、痰涂片阳性率低,导致诊断困难[8,9]。TB实验室诊断常用的标本有痰、胃液及血液等,传统TB诊断方法包括痰涂片和培养。痰涂片诊断TB的阳性率较低[4,10~12],结核分枝杆菌培养耗时需3~4周。
支气管镜对于儿童TB的诊断优势在于可直观病变部位,且可从病变部位直接取材获取病原学和(或)病理学标本。支气管肺泡灌洗液、支气管黏膜刷检及组织活检为TB诊断提供了帮助,其中支气管肺泡灌洗液是胸内TB诊断的最佳标本,可显著提高诊断阳性率[10,13~15]。目前关于支气管镜对TB诊断已有较多的关注[9,16],Zhen等[17]在2015年的Meta分析探讨了以成人支气管肺泡灌洗液为标本的酶联免疫斑点试验(ELISPOT)对TB的诊断;也有关于支气管镜对儿童TB诊断的定性系统综述[18],但未发现相关定量的评价。本文系统检索相关文献,评估支气管镜介导标本和检测方法对儿童TB的诊断价值,以期为临床应用提供参考。
1 方法
1.1支气管镜介导的标本及检测方法①标本类型:支气管肺泡灌洗液、支气管黏膜组织、支气管黏膜刷检;②检测方法:结核分枝杆菌培养、抗酸杆菌涂片、PCR、活检和Xpert 结核分枝杆菌/利福平试验(MTB/RIF)。
1.2文献纳入标准①入选病例均经支气管镜介导的标本诊断TB,且能获取诊断试验四格表数据,即真阳性值(TP )、假阳性值(FP)、假阴性值(FN) 、真阴性值(TN); ②TB诊断金标准为临床诊断或实验室诊断;③对照标本为胃液;④年龄0~18岁; ⑤中文和英文语种。
1.3文献排除标准未报道相关检测方法的文献。
1.4文献检索策略计算机检索PubMed、EMBASE、Cochrane图书馆、Ovid、中国生物医学文献数据库(CBM)、中国知网和万方数据库,检索起止时间为建库至2016年2月1日。同时回溯纳入文献的参考文献。
以PubMed为例的检索式为(bronchoscopy OR bronchoscope) AND ("Bronchoalveolar Lavage" OR "Bronchoscopy biopsy" OR "bronchial brushing") AND (children OR paediatric OR pediatric OR infant) AND (tuberculosis OR TB) AND (sensitivity OR specificity OR false negative OR false positive OR diagnosis)。
以CBM为例的检索式为("婴儿"[常用字段:智能] OR "幼儿"[常用字段:智能] OR "儿童"[常用字段:智能]) AND "支气管镜"[常用字段:智能] AND ( "肺泡灌洗液"[常用字段:智能] OR "支气管黏膜刷检"[常用字段:智能] OR "支气管镜活检"[常用字段:智能]) AND ("结核"[常用字段:智能]) AND ("诊断"[常用字段:智能] OR "特异性"[常用字段:智能] OR "敏感性"[常用字段:智能] OR "灵敏度"[常用字段:智能] OR "预测值"[常用字段:智能])。
1.5文献筛选和资料提取由付文龙和张娟娟根据纳入标准筛选文献,制定资料提取表格行资料提取和录入,交叉核对。提取的内容包括: 作者、发表时间、国家、样本量、性别比、标本类型、检测方法、纳入标本数及诊断试验数据等。如文献报道的数据不完整,通过邮件与作者联系索取。
1.6文献偏倚风险采用QUADAS-2量表[19]行偏倚风险评价,包括①病例的选择(3项内容),②待评价试验(2项内容),③金标准(2项内容),④病例流程和进展(3项内容),每一条标准以“是”、“否”、“不清楚”评价。由付文龙和张娟娟独立评价,遇到分歧讨论解决。
1.7统计学方法采用Meta-Disc 1.4软件行Meta分析。采用χ2检验行统计学异质性分析,P≤0.1为文献间存在显著异质性;采用I2对异质性进行定量,I2≤50%为中至低度异质性,采用固定效应模型描述;I2>50%为高度异质性,采用随机效应模型描述。根据标本类型和检测方法行亚组分析。对无法合并效应量文献行描述性分析。建立汇总受试者工作特征(SROC)曲线,并计算曲线下面积 (AUC)和Q*指数。以Stata 12.0软件绘制Deek′s漏斗图评估发表偏倚。P<0.05为差异有统计学意义。

2 结果
2.1文献检索结果共检索到文献651篇,图1显示文献筛选流程,14篇文献进入Meta分析[18,20~32]。

图1文献筛选流程图
2.2纳入文献的基本特征14篇文献来自7个国家(中国5篇,印度3篇,南非2篇,土耳其1篇,美国1篇,英国1篇,法国1篇)。共纳入1 082例患儿,2 781份支气管镜介导的标本。TB的种类:肺结核9篇[18,20,22,24,27~30,32],支气管内膜结核2篇[21,23],复杂胸内结核1篇[31],未分类2篇[25,26]。纳入文献的基本信息见表1,诊断参数见表2,支气管镜介导和胃液任一标本阳性即认为病例实验室阳性,诊断4格表数据均以例数表示。
2.3文献偏倚评价结果QUADAS-2量表评估结果显示,①病例选择:5篇文献[22,23,26,27,31]纳入病例非连续或随机,有高度偏倚,余9篇文献为低度偏倚;②待评价试验:4篇[18,21,29,30]文献采用双盲法评估结果,为低度偏倚,10篇文献[20,22~28,31,32]为高度偏倚;③金标准:13篇文献[18,20~31]为低度偏倚,文献[32]为不清楚;④病例流程和进展:14篇文献均为低度偏倚。
2.4Meta分析结果
2.4.1支气管镜介导所有标本对TB的诊断价值14篇文献报道了支气管镜介导标本对TB的诊断。异质性检验P<0.001,I2=83.0%,文献间具异质性,随机效应模型Meta分析结果显示,汇总敏感度0.38(95%CI:0.34~0.41),特异度为1.00(95%CI:0.99~1.00)。
2.4.2支气管肺泡灌洗液对TB的诊断14篇文献报道

表2 支气管镜介导标本和胃液对儿童结核病诊断的参数信息
了支气管肺泡灌洗液对TB的诊断。异质性检验P<0.001,I2=86.0%,采用随机效应模型合并结果。Meta分析结果显示,汇总敏感度0.37(95%CI:0.34~0.40),特异度为1.00(95%CI:0.99~1.00)。
根据标本和检测方法不同行亚组分析(图2), 11篇文献[20~23,25,26,28~32]报道了支气管肺泡灌洗液培养,异质性检验P<0.001,I2=79.5%,采用随机效应模型,汇总敏感度0.36(95%CI:0.32~0.40),特异度1.00(95%CI:0.99~1.00);5篇文献[18,22,30~32]报道了支气管肺泡灌洗液涂片,异质性检验P<0.001,I2=91.3%,采用随机效应模型,汇总敏感度0.21(95%CI:0.15~0.28),特异度1.00(95%CI:0.98~1.00);3篇文献[22,25,28]报道了支气管肺泡灌洗液PCR,异质性检验P<0.001,I2=0,固定效应模型汇总敏感度0.58(95%CI:0.46~0.69),特异度1.00(95%CI:0.84~1.00);2篇文献报道了支气管肺泡灌洗液Xpert MTB/RIF,异质性检验P=0.430,I2=0,固定效应模型的汇总敏感度0.55(95%CI:0.44~0.65),特异度1.00(95%CI:0.98 ~1.00)。
2.4.3组织活检对TB的诊断4篇文献[22,26~28]报道了支气管镜黏膜组织活检(图2),异质性检验P=0.062,I2=59.1%,采用随机效应模型,汇总敏感度0.51(95%CI:0.40~0.61),特异度1.00(95%CI:0.81~1.00)。

图2支气管镜介导不同标本和检测方法对儿童结核病诊断的汇总敏感度和特异度
2.4.4支气管黏膜刷检对TB的诊断文献[24]显示支气管黏膜刷检培养、涂片及PCR诊断TB的敏感度分别为0.33(95%CI:0.17~0.54),0.30(95%CI:0.14~0.50)和0.33(95%CI:0.17~0.54),特异度均为1.00(95%CI:0.86~1.00)。3种检测方法汇总敏感度为0.32(95%CI:0.22~0.43),特异度1.00(95%CI:0.95~1.00)。
2.4.5胃液对TB的诊断价值纳入10篇文献[17,18,20,21,23,25,26,29~31],异质性检验P<0.001,I2=93.3%,随机效应模型汇总敏感度为0.45(95%CI:0.40~0.49),特异度1.00(95%CI:0.99~1.00)。
根据检测方法行亚组分析(图3), 8篇文献[20,21,23,25,26,29~31]采用胃液培养,异质性检验P<0.001,I2=95.4%,汇总敏感度0.52(95%CI:0.47~0.57),特异度1.00(95%CI:0.98~1.00);5篇文献[17,18,29~31]采用涂片,异质性检验P=0.006,I2=72.5%,汇总敏感度0.25(95%CI:0.16~0.36),特异度1.00(95%CI:0.95~1.00); 1篇文献[25]采用PCR,敏感度0.31(95%CI:0.22~0.42),特异度1.00(95%CI:0.95~1.00)。
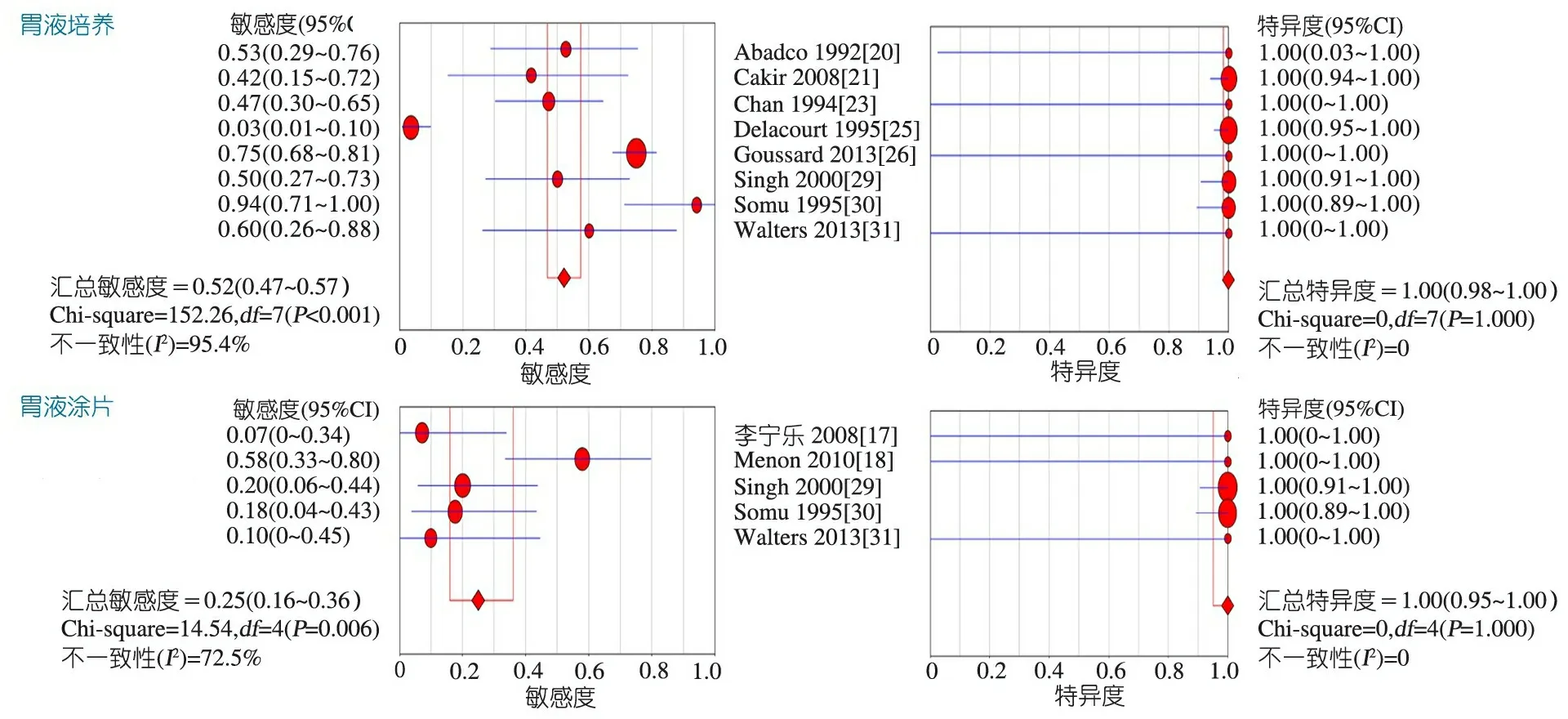
图3胃液不同检测方法对儿童结核病诊断的汇总敏感度和特异度
2.5SROC分析支气管镜介导所有标本及检测方法(5种)诊断TB的SROC AUC为0.881 8,Q*为0.812 3(图4A);其中支气管肺泡灌洗液所有(4种)、培养和涂片检测诊断TB的SROC AUC分别为0.883 9、0.864 7和0.787 2,Q*分别为0.814 5、0.795 3和0.724 8;胃液所有检测方法诊断TB的SROC AUC为0.873 7,Q*为0.804 2(图4B),其中胃液培养和涂片诊断TB的SROC AUC分别为0.892 9和0.737 8,Q*分别为0.823 7和0.683 4。
2.6发表偏倚分析支气管镜介导所有标本及检测方法文献的漏斗图不对称(图4C),且Deek′s检验P<0.05,提示存在发表偏倚;支气管肺泡灌洗液培养和涂片诊断TB文献的Deek′s检验P分别为0.005和0.014。胃液诊断儿童TB文献的漏斗图略不对称(图4D),Deek′s检验P=0.147,提示发表偏倚不显著,胃液培养诊断儿童TB文献的Deek′s检验P=0.935。其他各亚组因文献数量少未行发表偏倚检验。
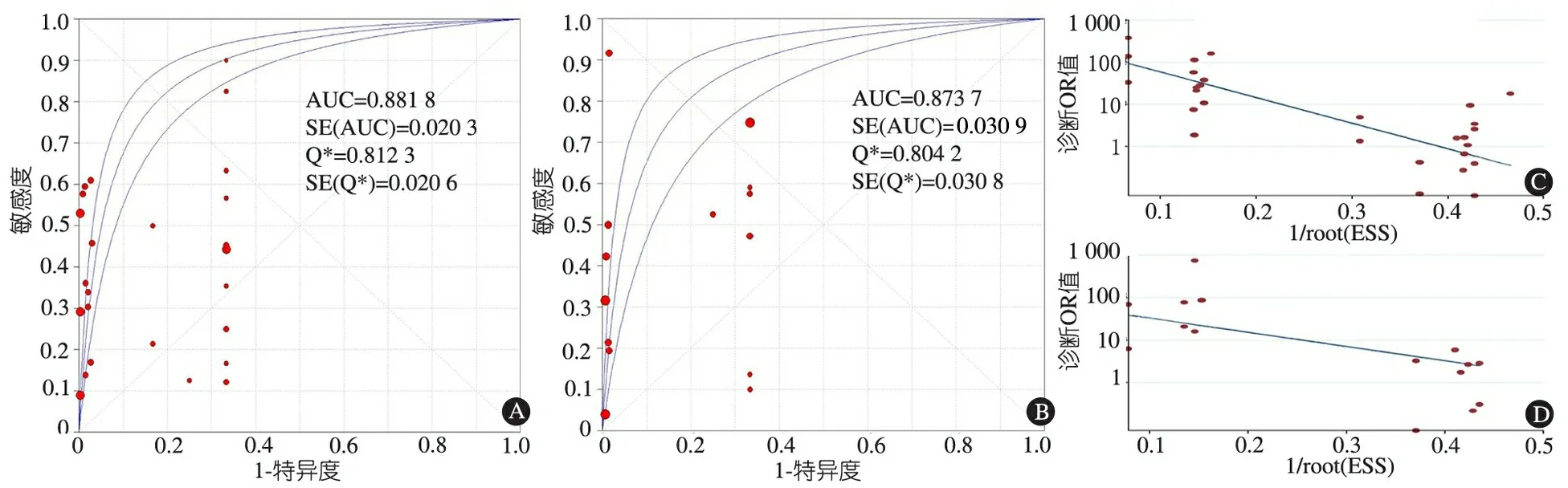
图4诊断儿童结核病汇总受试者工作特征曲线(SROC)和发表偏倚Deek′s漏斗图
注A:支气管镜介导所有标本及检测方法诊断结核病的SROC;B:胃液所有检测方法诊断结核病的SROC;C:支气管镜介导所有标本及检测方法诊断结核病文献的Deek′s漏斗图;D:胃液所有检测方法诊断儿童结核病文献的Deek′s漏斗图
3 讨论
本文Meta分析纳入14篇文献,根据QUADAS-2量表条目来评价文献偏倚风险,在金标准、病例流程和进展的偏倚风险为低度,在病例选择上5/14篇文献为高度偏倚,待评价试验10/14篇为高度偏倚,总体偏倚风险为低度。同时纳入文献间存在一定的临床异质性,如标本类型(支气管肺泡灌洗液、支气管黏膜刷检和组织)、检测方法(培养、涂片、PCR、活检及Xpert MTB/RIF)、目标人群(年龄、感染部位及状态不同)、研究方案(前瞻性、回顾性研究)及TB诊断参考标准(临床、实验室)等均有所不同,报告敏感度的文献间存在显著的统计学异质性,行亚组分析但仍不能完全消除异质性,且支气管镜介导的所有标本和支气管肺泡灌洗液培养的文献存在发表偏倚,结合GRADE证据质量评价工具,支气管镜介导标本及其检测方法诊断儿童TB的证据质量为低至中。
本文SROC分析显示,支气管镜介导所有标本和检测方法诊断TB的AUC 为0.881 8,胃液对TB诊断AUC 0.873 7,提示两者对儿童TB有较好的诊断价值。支气管镜介导的3种标本对TB诊断价值,其中支气管黏膜组织活检的敏感度最高为0.51,支气管刷检的敏感度最低为0.32,特异度均为1.00,但由于这2种标本纳入文献较少,结果存在不精确性,有待进一步评估。支气管肺泡灌洗液作为最常用的标本,诊断总体敏感度为0.37,以其为标本的4种检验方法中,PCR对TB诊断的敏感度最高为0.58,这与既往研究结果相近。Tian等[33]在2015年以支气管肺泡灌洗液为标本PCR对痰涂片阴性TB诊断的Meta分析结果显示,敏感度为0.54,而另外2篇[34,35]基于各种标本的Meta分析结果显示PCR诊断TB敏感度分别为0.85和0.96;本文支气管肺泡灌洗液涂片敏感度最低为0.21,培养敏感度为0.36,Xpert MTB/RIF敏感度为0.55。尹青琴等[36]基于各种标本Xpert MTB/RIF的Meta分析结果提示儿童和成人的敏感度分别为0.74和0.90。本文结果与既往研究不一致,主要考虑有2方面原因,一是与儿童携菌率低有关[36],二是用于支气管镜检查的TB多不典型。
胃液的收集与支气管镜的检查均为侵入性操作,而支气管肺泡灌洗液作为支气管镜检查最常用的标本,两者常被用于对比。本文关于胃液对TB的诊断有3种检测方法,其中PCR仅有1篇文献;培养和涂片的敏感度分别为0.52和0.25,均优于支气管肺泡灌洗液,与已报道的文献结果一致[18],考虑主要有以下几方面原因[30]:①多项研究中每例患儿是连续取3 d清晨的胃液标本,而支气管肺泡灌洗液每例患儿大多仅留取1个标本。②儿童TB通常含菌量少,影像学有肺实质浸润或淋巴结肿大,因此分离细菌相对困难。③支气管肺泡灌洗液是注入生理盐水后获取的,进一步稀释气道分泌物浓度,检出少数结核分枝杆菌可能性减少。④由于技术原因,支气管镜不一定能到达病变的确切部位,特别是在年幼儿童的小气道。因此,样本可能不包含受影响段的分泌物。
本文系统评价的局限性:①未能获取未发表的文献,因而不能排除潜在的发表偏倚;②只纳入英文和中文文献,可能存在语种偏倚。
[1]罗汶鑫. 支气管镜术与多项无创检查对痰菌阴性儿童肺结核的诊断应用. 重庆医科大学, 2014
[2]Marais BJ, Schaaf HS. Tuberculosis in children. Cold Spring Harb Perspect Med, 2014, 4(9): a017855
[3]Seddon JA, Shingadia D. Epidemiology and disease burden of tuberculosis in children: a global perspective. Infect Drug Resist, 2014, 7: 153-165
[4]WHO. Global Tuberculosis Report. Geneva: World Health Organization. 2014
[5]Dodd PJ, Gardiner E, Coghlan R, et al. Burden of childhood tuberculosis in 22 high-burden countries: a mathematical modelling study. Lancet Glob Health, 2014, 2(8): e453-459
[6]Detjen AK, DiNardo AR, Leyden J, et al. Xpert MTB/RIF assay for the diagnosis of pulmonary tuberculosis in children: a systematic review and meta-analysis. Lancet Respir Med, 2015, 3(6): 451-461
[7]WHO. Global Tuberculosis Report. Geneva: World Health Organization; 2015. In: http://apps.who.int/iris/bitstream/10665/191102/1/9789241565059_eng.pdf?ua=1, 2015
[8]Seddon JA, Graham SM. Childhood TB: can the End TB Strategy deliver? Trans R Soc Trop Med Hyg, 2016, 110(3): 155-157
[9]Goussard P, Gie R. The role of bronchoscopy in the diagnosis and management of pediatric pulmonary tuberculosis. Expert Rev Respir Med, 2014, 8(1): 101-109
[10]Shin JA, Chang YS, Kim TH, et al. Fiberoptic bronchoscopy for the rapid diagnosis of smear-negative pulmonary tuberculosis. BMC Infect Dis, 2012, 12: 141
[11]Kamal R, Sharma R, Sahasrabuddhe T, et al. A prospective study to evaluate the utility of bronchoalveolar lavage by fiberoptic bronchoscopy in sputum smear negative patients with high suspicion of pulmonary tuberculosis. Medical Journal of Dr. DY Patil University, 2012, 5(1): 43
[12]Yuksekol I, Bal S, Ozkan M, et al. The value of fiberoptic bronchoscopy in diagnosis of smear negative pulmonary tuberculosis. Tuberk Toraks, 2003, 51(4): 405-409
[13]Boonsarngsuk V, Suwannaphong S, Laohavich C. Combination of adenosine deaminase activity and polymerase chain reaction in bronchoalveolar lavage fluid in the diagnosis of smear-negative active pulmonary tuberculosis. Int J Infect Dis, 2012, 16(9): e663-668
[14]Tamura A, Shimada M, Matsui Y, et al. The value of fiberoptic bronchoscopy in culture-positive pulmonary tuberculosis patients whose pre-bronchoscopic sputum specimens were negative both for smear and PCR analyses. Intern Med, 2010, 49(2): 95-102
[15]Altaf Bachh A, Gupta R, Haq I, et al. Diagnosing sputum/smear-negative pulmonary tuberculosis: Does fibre-optic bronchoscopy play a significant role? Lung India, 2010, 27(2): 58-62
[16]Venkateshiah SB, Mehta AC. Role of Flexible bronchoscopy in the diagnosis of pulmonary tuberculosis in immunocompetent individuals. Journal of Bronchology, 2003, 10(4): 300-308
[17]Li Z, Qin W, Li L, et al. Accuracy of bronchoalveolar lavage enzyme-linked immunospot assay to diagnose smear-negative tuberculosis: a meta-analysis. Int J Clin Exp Med, 2015, 8(8): 12637-12643
[18]Menon RP, Lodha R, Singh U, et al. A prospective assessment of the role of bronchoscopy and bronchoalveolar lavage (BAL) in evaluation of children with pulmonary tuberculosis. J Trop Pediatr, 2011, 57(5): 363-367
[19]邬兰, 张永, 曾宪涛. QUADAS-2在诊断准确性研究的质量评价工具中的应用. 湖北医药学院学报, 2013, (03): 201-208
[20]Abadco DL, Steiner P. Gastric lavage is better than bronchoalveolar lavage for isolation of Mycobacterium tuberculosis in childhood pulmonary tuberculosis. Pediatr Infect Dis J, 1992, 11(9): 735-738
[21]Cakir E, Uyan ZS, Oktem S, et al. Flexible bronchoscopy for diagnosis and follow up of childhood endobronchial tuberculosis. Pediatr Infect Dis J, 2008, 27(9): 783-787
[22]曹丽洁, 黄英, 李渠北, 等. 纤支镜术及其肺泡灌洗术在儿童疑难肺结核的诊断应用. 中华医学会第十七次全国儿科学术大会, 2012: 1
[23]Chan S, Abadco DL, Steiner P. Role of flexible fiberoptic bronchoscopy in the diagnosis of childhood endobronchial tuberculosis. Pediatr Infect Dis J, 1994, 13(6): 506-509
[24]Chen QP, Ren SF, Wang XF, et al. Comparison of bronchial brushing and sputum in detection of pediatric pulmonary tuberculosis. Ital J Pediatr, 2016, 42(1): 11
[25]Delacourt CMD, Poveda J-DMD, Chureau C, et al. Use of polymerase chain reaction for improved diagnosis of tuberculosis in children. J Pediatr, 1995, 126(5): 703-709
[26]Goussard PM, Gie RP, Kling S, et al. Bronchoscopic assessment of airway involvement in children presenting with clinically significant airway obstruction due to tuberculosis. Pediatr Pulmonol, 2013, 48(10): 1000-1007
[27]李宁乐, 汪天林. 小儿肺结核56例临床分析. 中国全科医学, 2008, 11(17): 1587-1588
[28]孟燕妮, 陈艳萍, 李秀龙, 等. 结核感染T细胞斑点试验联合纤维支气管镜检在结核病患儿诊断中的应用. 疑难病杂志, 2014, (9): 907-909,912
[29]Singh M, Moosa NV, Kumar L, et al. Role of gastric lavage and broncho-alveolar lavage in the bacteriological diagnosis of childhood pulmonary tuberculosis. Indian Pediatr, 2000, 37(9): 947-951
[30]Somu N, Swaminathan S, Paramasivan CN, et al. Value of bronchoalveolar lavage and gastric lavage in the diagnosis of pulmonary tuberculosis in children. Tuber Lung Dis, 1995, 76(4): 295-299
[31]Walters E, Goussard P, Bosch C, et al. GeneXpert MTB/RIF on bronchoalveolar lavage samples in children with suspected complicated intrathoracic tuberculosis: A pilot study. Pediatr Pulmonol,2014,49(11):1133-1137
[32]Shen AD, Jiao W, Shen C, et al. Rapid diagnosis of childhood pulmonary TB using bronchoalveolar lavage fluid by Xpert MTB/RIF assay. Int J Infect Dis, 2014, 21: 303
[33]Tian P, Shen Y, Wang Y, et al. Diagnostic value of nucleic acid amplification tests on bronchoalveolar lavage fluid for smear-negative pulmonary tuberculosis: a meta-analysis. Biosci Rep, 2015, 35(4):e00232
[34]Ling DI, Flores LL, Riley LW, et al. Commercial nucleic-acid amplification tests for diagnosis of pulmonary tuberculosis in respiratory specimens: meta-analysis and meta-regression. PLoS One, 2008, 3(2): e1536
[35]Greco S, Rulli M, Girardi E, et al. Diagnostic accuracy of in-house PCR for pulmonary tuberculosis in smear-positive patients: meta-analysis and metaregression. J Clin Microbiol, 2009, 47(3): 569-576
[36]尹青琴, 焦伟伟, 孙琳, 等. Xpert结核分枝杆菌/利福平试验对结核病及耐多药结核病诊断价值的Meta分析. 中国循证儿科杂志, 2012, 7(5): 341-348
(本文编辑:丁俊杰)
Diagnostic value of specimens via bronchoscopy for tuberculosis in children: a systematic review and meta-analysis
FUWen-long1,2,ZHANGJuan-Juan1,DAIJi-hong2
(1KeyLaboratoryofDevelopmentalDiseasesinChildhood,MinistryofEducation, 2CenterofRespiratoryDisordersofChildren′sHospital,ChongqingMedicalUniversity,Chongqing400014,China)
DAI Ji-hong,E-mail:danieljh@163.com
Bronchoscopy; Children; Tuberculosis; Diagnostic value; Sensitivity;Specificity;Systematic review;Meta-analysis
重庆医科大学附属儿童医院1 儿童发育与疾病教育部重点实验室,2 呼吸中心重庆,401104
代继宏,E-mail:danieljh@163.com
10.3969/j.issn.1673-5501.2016.03.006
2016-03-30
2016-05-17)