中低危分化型甲状腺癌经131I治疗后短期Tg转阴情况的动态监测
李从心,侯 敏,任 超,林岩松
中国医学科学院 北京协和医学院 北京协和医院核医学科,北京 100730
·论著·
中低危分化型甲状腺癌经131I治疗后短期Tg转阴情况的动态监测
李从心,侯敏,任超,林岩松
中国医学科学院北京协和医学院北京协和医院核医学科,北京 100730
摘要:目的动态监测分化型甲状腺癌(DTC)患者131I治疗后早期的血清学指标,探讨甲状腺球蛋白(Tg)转阴情况及其影响因素。方法纳入22例中低危DTC患者随访观察,于131I治疗当天、治疗后4周内每周动态监测患者血清促甲状腺素(TSH)、Tg、甲状腺球蛋白抗体(TgAb)水平,观察患者Tg转阴的动态规律。根据患者在观察期末Tg是否转阴分为G1组(Tg≤0.1 ng/ml,n=9)和G2组(Tg>0.1 ng/ml,n=13)两组,测定患者131I治疗后残余甲状腺对放射性碘的摄取指数,进一步分析年龄、性别、TSH、残余甲状腺等因素与131I治疗后1月末Tg转阴的关系。结果治疗当天,治疗1、2、3、4周的人群总体血清Tg转阴率分别为4.5%、18.0%、27.0%、36.0%、41.0%。单因素分析结果显示,两组患者在年龄(F=3.182,P=0.04)和残余甲状腺指数(U=4.849,P=0.026)等方面差异有统计学意义。多因素Logistic回归分析结果显示,131I后早期Tg能否转阴与残余甲状腺(OR:2.132,95%Cl:1.418~6.532,P=0.009)密切相关。结论近半数中低危DTC患者的血清Tg水平已于131I治疗后4周转阴。Tg的转阴与患者术后甲状腺残余量密切相关。
关键词:分化型甲状腺癌;131I治疗;Tg动态变化;Tg转阴;残余甲状腺
ActaAcadMedSin,2016,38(3):351-355
中低危分化型甲状腺癌(differentiated thyroid cancer,DTC)患者抑制性促甲状腺激素(thyroid stimulating hormone,TSH)<0.1 μU/ml时的甲状腺球蛋白(thyroglobulin,Tg)水平≤0.1 ng/ml对其无病状态有良好的阴性预测价值[1- 7],但目前有关Tg的研究主要侧重于131I治疗后的长期随访[8- 10],因此对病情早期监控的指导意义有限。本研究监测了中低危DTC患者131I治疗后早期的血清学指标,探讨了Tg转阴情况及其影响因素,以期为早期病情监测及随诊提供依据。
对象和方法
对象2015年3月至5月在北京协和医院核医学科行131I治疗的DTC患者49例,根据影像学及病理资料等进行术后(AJCC/UICC)TNM分期,排除复发危险度分层[11]高危患者和可能对Tg水平产生影响的高TgAb(>46 U/ml[12])患者,纳入具备连续4周监测Tg等血清学指标及影像学资料齐全的中低危患者22例,其中,男7例,女15例,平均年龄(36.1±10.7)岁(20~68岁);平均131I治疗剂量为(46.36±42.15) mCi(30~150 mCi);肿瘤病理均为甲状腺乳头状癌(papillary thyroid cancer,PTC),肿瘤最大直径均值为(1.7±0.9) cm(0.6~2.8 cm);局部淋巴结转移数量平均为(4.6±7.6)个(1~32个)。所有患者均行甲状腺全切或次全切术及131I治疗。
方法根据2009年美国甲状腺学会(American Thyroid Association,ATA)甲状腺癌治疗指南,对患者的DTC复发危险进行分层,排除高危患者,具备以下任何1条即为高危患者:(1)肉眼下可见肿瘤侵犯周围组织或器官;(2)肿瘤未能完全切除,术中有残留;(3)伴有远处转移;(4)全甲状腺切除后,血清Tg水平仍较高;(5)有甲状腺癌家族史[11]。将中低危患者纳入分层。
患者复发危险的确定方法包括手术后病理结果及影像学评估。131I治疗前常规检查包括血清学监测[Tg、甲状腺球蛋白抗体(anti-thyroglobulin,TgAb)和TSH水平测定]和影像学评估(131l全身显像、胸部CT、全身骨显像等)。所有患者131I治疗准备均参照2009年ATA甲状腺癌治疗指南[11]。每位患者在治疗当天(术后未服用甲状腺激素或停药后TSH升高至>30 μU/ml状态下)测量甲功生化,记为Tg 0;131I治疗后1个月内血清Tg及相应TSH、TgAb水平行动态监测(4周Tg测量值分别记为Tg1~Tg4,TSH和TgAb以此类推)。Tg和TgAb测定采用电化学发光免疫分析法(electro-chemiluminescence immunoassay,ECLIA)(美国罗氏公司,E170),检测范围分别为0.1000~500.0000 ng/ml和10~4000 U/ml。TSH测定采用CLIA法(德国拜耳公司,ADVIA CENTAVRXP),检测范围为0.004~150.000 μU/ml。此研究的中低危人群中,Tg测量值均在检测范围(0~500 ng/ml)内,TSH测量值若超过其测定范围则记为150 μU/ml。根据患者观察期终末的血清Tg水平分为G1组(Tg≤0.1 ng/ml,n=9)和G2组(Tg>0.1 ng/ml,n=13)两组。
根据ATA指南[11],所有患者均于131I治疗后48 h:(1)给予L-T4抑制治疗(2~2.5 μg·kg·d-1);(2)行131I全身显像(双源γ高能平行孔准直器Infinia Hawkeye 4,GE 医疗,USA);(3)测定患者131I治疗后残余甲状腺对放射性碘的摄取指数(残余甲状腺摄碘计数/全身碘摄取计数)。所有131I全身显像报告由3位经验丰富的核医学医/技师独立完成,最终3人在残余甲状腺对放射性碘的摄取指数测定上达成一致。
统计学处理采用SPSS 22.0统计软件。作出131I治疗后Tg转阴率的动态随时间变化曲线,分析曲线特点;根据患者在观察期终末的血清Tg水平分为两组:G1(Tg≤0.1 ng/ml,n=9),G2(Tg>0.1 ng/ml,n=13),采用单因素方差分析、χ2检验和Mann-Whitney U检验、Kruskal-Wallis秩和检验分别比较2组患者年龄、性别、131I治疗4周时TSH水平、颈部局部淋巴结转移、肿瘤腺外侵犯和131I治疗4周后Tg转阴的相关性等特征差异。P<0.05为差异有统计学意义。
结果
131I治疗后Tg随时间发生的变化131I治疗后早期,患者Tg总体转阴率呈上升趋势。4周观察期内,治疗当天及每周结束时的人群总体转阴率依次为4.5%、18.0%、27.0%、36.0%、41.0%(图1)。至观察期末,22例患者中有9例血清Tg转阴(<0.1 ng/ml)。
两组患者TSH随时间变化情况131I治疗后早期,两组患者TSH均呈明显下降趋势。在4周观察期内,G1组患者的平均TSH水平始终明显高于G2组(图2)。单因素分析结果显示,两组患者在性别(χ2=0.646,P=0.372)、131I治疗后4周时TSH水平(F=1.450,P=0.249)、肿瘤腺外侵犯(U=1.464,P=0.691)、局部淋巴结转移(χ2=0.627,P=0.361)和ps-Tg即Tg 0水平(F=2.193,P=0.819)
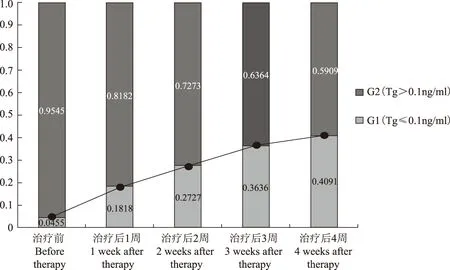
图 1甲状腺球蛋白转阴人群百分比变化趋势
Fig 1Variation trend of thyroglobulin negative conversion proportion

TSH:促甲状腺激素
TSH:thyroid stimulating hormone
图 2131I治疗后4周内两组TSH的散点分布及均值曲线比较
Fig 2The scatter diagram and average curves of TSH between the 2 groups within 4 weeks after131I therapy
方面差异无统计学意义;在年龄(F=3.182,P=0.040)和残余甲状腺指数(U=4.849,P=0.026)等方面差异有统计学意义(表1)。多因素Logistic回归分析结果显示,131I后早期Tg能否转阴与残余甲状腺(OR:2.132,95%Cl:1.418~6.532,P=0.009)密切相关,与年龄(OR:2.188,95%Cl:1.318~15.044,P=0.117)和颈部淋巴结转移(OR:2.000,95%Cl:1.356~11.230,P=0.852)无关。
讨论
目前研究显示,中低危DTC人群的抑制性Tg≤0.1 ng/ml对DTC的复发有良好的阴性预测价值[1- 7]。Smallridge等[7]研究发现,中低危人群抑制性Tg低于0.1 ng/ml时DTC的复发、转移率均低于1%。目前有关中低危人群Tg的研究侧重于131I治疗后长期随访中Tg转阴对清甲效果及远期预后的预测作用,例如Stevic等[13]对患者5 d、3个月、半年病情转归的追踪显示,残余甲状腺影响131I治疗后较长时间内的Tg转阴。但这些研究的随访周期长短不一,较长的随访周期难免遗漏131I治疗后短期内的Tg变化,且文献中鲜有131I治疗后短期内动态观察Tg变化、转阴时间及其影响因素的报道[8- 10,13- 14]。本研究则规律性观察了131I治疗后4周内早期131I治疗后Tg的动态变化。
通过对131I治疗后短期内的Tg等血清学指标进行动态监测,本研究发现131I治疗后至4周观察期末有41%的患者血清Tg转阴,提示有望早在131I治疗后1个月时即可通过Tg的转阴预测到患者良好预后的可能性。由于目前各指南仍建议在131I治疗后至少半年以上患者进行131I治疗后清甲效果及风险分层再评估,这意味着在此评估之前,医生针对这些中高危患者将采取密切随诊的方式,患者将处于紧张状态,本研究则有助于更早地动态地评估预后,并对疾病分期作出适时早期调整,从而为及时放宽Tg转阴患者随诊密度提供了循证依据,也因此及时、尽早地减轻了患者对疾病的担忧和焦虑,有助于其病情恢复和提高生活质量。
本研究在两组患者年龄和TSH匹配的情况下,进一步针对影响血清Tg转阴的单因素分析表明,患者在131I治疗后4周末血清Tg水平能否转阴,与患者术后甲状腺残余量及年龄有关。多因素回归分析进一步证实,残余甲状腺与Tg早期转阴之间密切相关,推测其可能是由于131I治疗破坏了过多的残余甲状腺引发的一过性血清Tg升高,从而延缓了这部分患者的Tg转阴时间;而年龄较大的患者有可能因其对TSH的敏感性减退,导致Tg下降相对缓慢,故131I治疗4周末血清Tg转阴者相对较少。尽管TSH对Tg的变化有很大影响,但在本研究中,通过对两组患者TSH的比较及单因素分析均发现,TSH水平并非是影响Tg转阴的独立因素。

表 1 临床病理特征与131I治疗后4周末血清Tg水平的单因素分析比较
TSH:促甲状腺激素;ps-Tg:131I治疗前刺激性甲状腺球蛋白
TSH:thyroid stimulating hormone;ps-Tg:pre-ablative thyroglobulin
综上,本研究结果显示,经131I治疗后4周,近半数中低危DTC患者即可通过Tg的转阴预示良好预后,这为放宽此部分患者的临床处置与随访密度提供了更为早期的依据,也将更早缓解患者因DTC造成的焦虑等不良情绪。Tg的转阴与患者术后甲状腺残余量密切相关。
参考文献
[1]Abdul-Sater L,Henry M,Majdan A,et al. What are thyroidectomy patients really concerned about [J]. Otolaryngol Head Neck Surg,2011,144(5):685- 690.
[2]Webb RC,Howard RS,Stojadinovic A,et al.The utility of serum thyroglobulin measurement at the time of remnant ablation for predicting disease-free status in patients with differentiated thyroid cancer:a meta-analysis involving 3947 patients [J].J Clin Endocrinol Metab,2012,97(8):2754- 2763.
[3]Malandrino P,Latina A,Marescalco S,et al.Risk-adapted management of differentiated thyroid cancer assessed by a sensitive measurement of basal serum thyroglobulin [J].J Clin Endocrinol Metab,2011,96(6):1703- 1709.
[4]Brassard M,Borget I,Edet-Sanson A,et al. Long-term follow-up of patients with papillary and follicular thyroid cancer:a prospective study on 715 patients [J].J Clin Endocrinol Metab,2011,96(5):1352- 1359.
[5]Giovanella L,Maffioli M,Ceriani L,et al. Unstimulated high sensitive thyroglobulin measurement predicts outcome of differentiated thyroid carcinoma [J].Clin Chem Lab Med,2009,47(8):1001- 1004.
[6]Chindris AM,Diehl NN,Crook JE,et al. Undetectable sensitive serum thyroglobulin (<0.1 ng/ml) in 163 patients with follicular cell-derived thyroid cancer:results of rhTSH stimulation and neck ultrasonography and long-term biochemical and clinical follow-up [J]. J Clin Endocrinol Metab,2012,97(8):2714- 2723.
[7]Smallridge RC,Meek SE,Morgan MA,et al. Monitoring thyroglobulin in a sensitive immunoassay has comparable sensitivity to recombinant human tsh-stimulated thyroglobulin in follow-up of thyroid cancer patients [J].J Clin Endocrinol Metab,2007,92(1):82- 87.
[8]Kloos RT. Thyroid cancer recurrence in patients clinically free ofdisease with undetectable or very low serum thyroglobulin values [J]. J Clin Endocrinol Metab,2010,95(12):5241- 5248.
[9]Rosario PW,Furtado MS,MineiroFilho AF,et al.Value of repeat stimulated thyroglobulin testing in patients with differentiated thyroid carcinoma considered to be free of disease in the first year after ablation [J].Thyroid,2012,22(5):482- 486.
[10]Nascimento C,Borget I,Troalen F,et al. Ultrasensitive serum thyroglobulin measurement is useful for the follow-up of patients treated with total thyroidectomy without radioactive iodine ablation [J]. Eur J Endocrinol,2013,169(5):689- 693.
[11]Cooper DS,Doherty GM,Haugen BR,et al.Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer [J]. Thyroid,2009,19(11)1167- 1214.
[12]张文杰,邓候富,潘明志,等. 分化型甲状腺癌患者内源性TgAb对血清Tg测定值、Tg阳性率的影响[J]. 生物医学工程学杂志,2013,30(4):803- 807.
[13]Stevic I,Dembinski TC,Pathak KA,et al.Transient early increase in thyroglobulin levels post-radioiodine ablation in patients with differentiated thyroid cancer [J].Clin Biochem,2015,48(10- 11):658- 661.
[14]桑士标,李清茹,姜继伟,等. DTC术后131I清甲治疗短期内血清Tg和TgAb变化及临床意义[J]. 标记免疫分析与临床,2014,21(6):649- 653.
基金项目:国家自然科学基金(30970850)和卫生部行业科研专项项目(201202012)Supported by the National Natural Sciences Foundation of China(30970850)and the Minister of Health Industry Special Scientific Research Project (201202012);第一、二位作者对本文贡献一致 The first two authors contributed equally to this article
通信作者:林岩松电话:010- 69155610,电子邮件:linys@pumch.cn
中图分类号:R736.1
文献标志码:A
文章编号:1000- 503X(2016)03- 0351- 05
DOI:10.3881/j.issn.1000- 503X.2016.03.020
Corresponding author:LIN Yan-songTel:010- 69155610,E-mail:linys@pumch.cn
(收稿日期:2015- 06- 24)
Serial Thyroglobulin Variation Trend Shortly after Radioiodine Therapy in Poorly to Moderately Differentiated Recurrent Thyroid Cancer
LI Cong-xin,HOU Min,REN Chao,LIN Yan-song
Department of Nuclear Medicine,PUMC Hospital,CAMS and PUMC,Beijing 100730,China
ABSTRACT:ObjectiveTo dynamically observe the early change of thyroglobulin(Tg) levels after131I therapy in differentiated thyroid cancer(DTC) patients. MethodsThe study enrolled 22 post-total-thyroidectomy DTC patients and they were stratified as low to intermediate recurrence according to the 2009 American Thyroid Association Guidelines. The clinical data including pre-ablation stimulated Tg (ps-Tg),corresponding thyroid stimulating hormone(TSH),anti-thyroglobulin (TgAb) values,and the afterwards parameters were dynamically measured each week in the first month after131I therapy. Values collected at the first time were defined as Tg 0 and TSH0,while Tg1 and TSH1 were collected at the first week after131I therapy respectively. Then the variation trend curves of Tg were drawn,and factors influencing the variation of Tg were analyzed. Two groups were divided according to Tg levels:G1 (Tg≤0.1 ng/ml,n=9) and G2(Tg>0.1 ng/ml,n=13). ResultsThe rates of negative Tg were 4.5%,18.0%,27.0%,36.0%,and 41.0%,respectively,exactly before131I therapy and the 1st,2nd,3rd,and 4thweek after the therapy. One-way analysis of variance showed that the two groups statistically differed in age (F=3.182,P=0.04) and remnant thyroid (U=4.849,P=0.026). Multivariate logistic regression analysis showed that early negative Tg was related to remnant thyroid tissue (OR:2.132;95%Cl:1.418- 6.532,P=0.009).ConclusionsNegative Tg can be achieved in nearly half of DTC patients by the end of first month after131I therapy. The negative conversion is closely related with the volume of remnant thyroid tissue.
Key words:differentiated thyroid cancer;radioiodine therapy;thyroglobulin variation trend;thyroglobulin turning negative;remnant thyroid issue

