获诊时间窗等临床病理因素对三阴性乳腺癌预后的影响
孙 矗,李洪涛,刘子梅,袁 媛,沈 赞上海交通大学附属第六人民医院肿瘤内科,上海 200233
获诊时间窗等临床病理因素对三阴性乳腺癌预后的影响
孙矗,李洪涛,刘子梅,袁媛,沈赞
上海交通大学附属第六人民医院肿瘤内科,上海 200233
[摘要]背景与目的:从症状首次出现到确诊的时间,称为获诊时间窗(diagnostic interval,DI)。三阴性乳腺癌(triple-negative breast cancer, TNBC)常见临床病理指标与DI的关系及DI对TNBC患者预后的影响尚不清楚,将对此进行深入研究。方法:回顾性分析上海市第六人民医院2009年9月—2015年9月收治的83例TNBC患者的资料。对DI等临床病理指标运用Kaplan-Meier法进行单因素分析,对其中差异有统计学意义者采用Cox回归模型进行多因素分析。运用t检验和Kruskal-Wallis检验对DI与常见指标间的关系进行深入研究。结果:DI:T3期>T1期(P=0.01),Ⅲ期>Ⅰ期(P=0.03)、Ⅱ期(P=0.01)。与DI≥3个月组相比,DI<3个月组的平均确诊年龄和TNM分期均较早(P=0.028和0.035)。T分期、N分期、新辅助化疗、TNM分期和DI是总生存时间(overall survival,OS)的影响因素,年龄、T分期、N分期、TNM分期、月经状态和新辅助化疗是无进展生存时间(progression-free survival,PFS)的影响因素,TNM分期是两者的独立影响因素。结论:疾病分期较晚者,DI较长;DI较短者确诊时的疾病分期和年龄均较早;DI是OS的影响因素;TNM分期是OS和PFS的独立影响因素。
[关键词]获诊时间窗;三阴性乳腺癌;生存分析
乳腺癌是全球女性最常见的恶性肿瘤,是女性癌症相关性死亡的首要原因[1]。三阴性乳腺癌(triple-negative breast cancer,TNBC),是雌激素受体(estrogen receptor,ER)、孕激素受体(progestrogen receptor,PR)和人类表皮生长因子受体2(human epidermal growth factor receptor-2,HER-2)均无表达的乳腺癌类型,占所有乳腺癌的12%~17%[2]。与其他亚型相比,TNBC复发率更高、无进展生存时间(progression-free survival,PFS)和总生存时间(overall survival,OS)更短。复发TNBC患者的中位OS是1~2年,而转移性TNBC患者只有1年[3-4]。年龄、肿瘤大小和分期等常见临床病理指标对预后的影响,已有不少文献报道[5-7],本文将纳入更多指标进一步分析。
对肿瘤患者来说,症状出现后的快速确诊,对于改善预后、提高生存质量十分重要。从症状出现到疾病确诊的时间,称为获诊时间窗(diagnostic interval,DI)[8-9]。较短的DI有助于获得较早的分期和较好的预后[10-11]。有文献报道,DI的大小受包括年龄在内的诸多因素影响[8,12-14]。然而,对TNBC群体中DI的特征及其与预后之间关系的研究,国内外鲜有报道,本文将对此进行深入探讨。
1 资料和方法
1.1病例收集
收集上海市第六人民医院2009年9月—2015 年9月收治的、经病理学检查证实的83例TNBC患者。随访从患者确诊之日(穿刺或手术活检)开始计算,随访至2015年9月30日。随访方式包括门诊和电话随访。患者死亡、失访或随访截止仍生存者均记为截尾值。OS定义为术后第1天至患者死亡或末次随访的时间,PFS定义为术后第l天至首次出现复发或转移的时间。ER、PR阴性指免疫组化染色阳性细胞在1%以下[15-17]。排除因体检或其他原因(非乳腺癌相关症状)获诊的病例。
1.2统计学处理
DI以3个月为界值[18],采用t检验和Kruskal-Wallis检验比较组间差异。将可能影响预后的临床病理因素(年龄、月经状态、家族史、DI、T分期、N分期、TNM分期、手术方式、是否接受新辅助化疗和原发灶所在象限)量化赋值后,以OS、PFS作为反映预后的指标,进行统计分析。单因素分析采用Kaplan-Meier法,对可能影响预后的指标进行初筛,用log-rank检验比较显著性水平。统计描述及分析采用SPSS 19.0软件,P<0.05为差异有统计学意义。将单因素分析提示差异有统计学意义的指标,纳入Cox回归模型进行多因素分析并筛选独立预后因素。
2 结 果
2.1临床病理特征与DI的分组分析
各指标的统计描述见表1。83例患者的中位确诊年龄是56岁(24~92岁),中位DI为0.67个月(0.17~24.30个月),平均肿块大小为2.59 cm (1~7 cm)。将年龄、N分期、原发灶象限、病理类型、月经状态和手术方式进行分组分析发现,各组内的DI差异无统计学意义(P=0.34、0.17、0.69、0.90、0.27和0.28)。将TNM分期和T分期进行分组分析后发现,T1和T3两组间DI差异有统计学意义(P=0.01),而T1和T2、T2和T3之间差异无统计学意义(P均>0.05);Ⅲ期和Ⅱ期、Ⅲ期和Ⅰ期之间DI差异有统计学意义(P=0.01、0.03),Ⅰ期和Ⅱ期之间差异无统计学意义(P>0.05,图1)。以3个月为界值对DI分组,发现DI<3个月组与DI≥3个月组之间,年龄、TNM分期的差异有统计学意义(P=0.028、0.035),PFS、OS、肿瘤大小和淋巴结转移数的差异无统计学意义(P均>0.05,表2)。
2.2DI等临床病理指标对PFS和OS的影响
83例患者的中位OS是30个月,中位PFS 为27个月。死亡7例。复发转移16例。其中,骨转移5例,骨合并肺转移2例,肺转移1例,肝转移2例,其余部位转移6例。单因素分析显示,T分期、N分期、新辅助化疗、TNM分期和DI是OS的影响因素,年龄、T分期、N分期、TNM分期、月经状态和新辅助化疗是PFS的影响因素,生存曲线见图2。对单因素分析中差异有统计学意义的指标,进一步应用Cox多因素分析,结果显示,TNM分期是OS和PFS的独立影响因素(P=0.025和0.007,表3)。
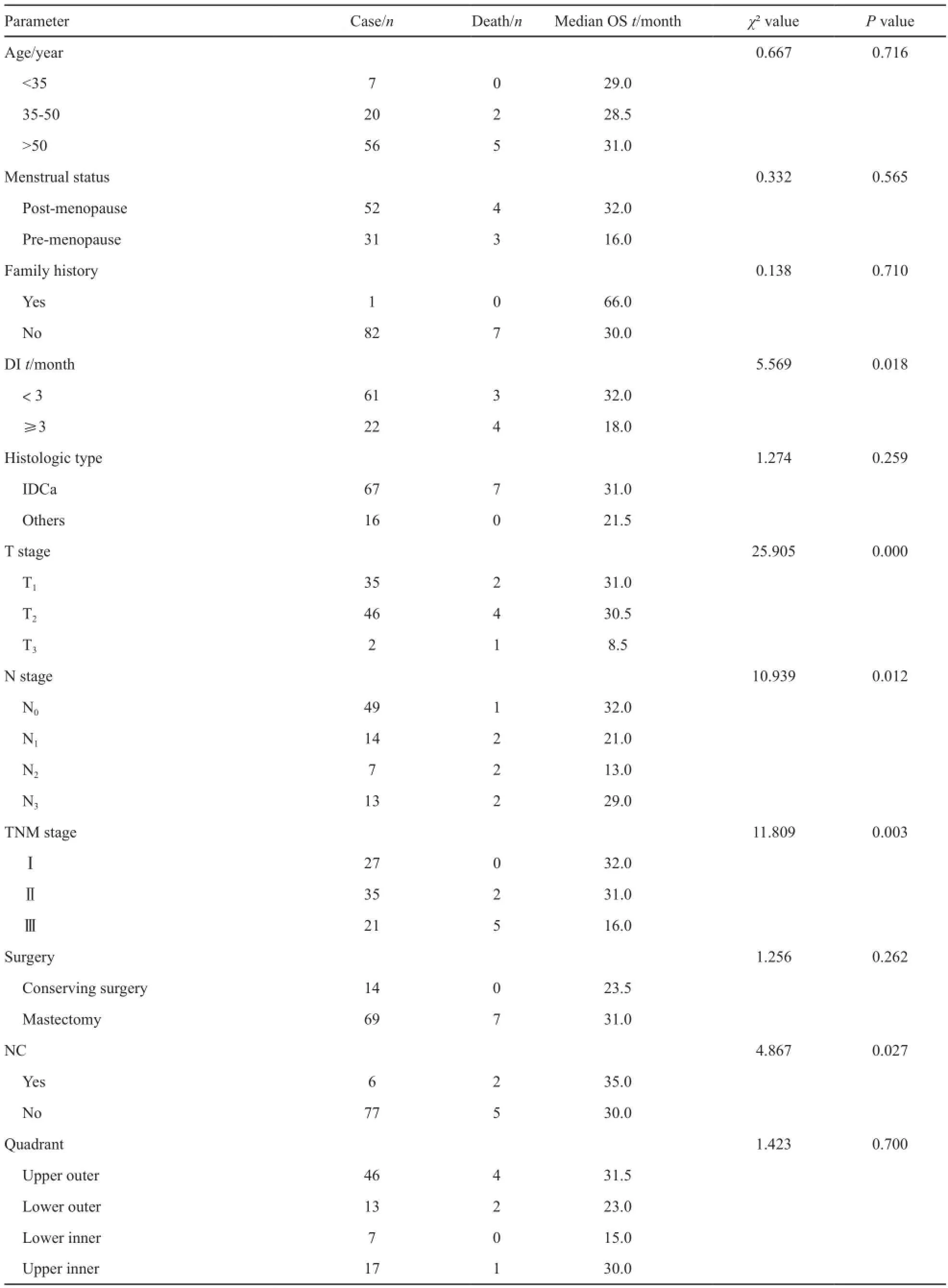
表1 83例TNBC患者临床病理特征及预后单因素分析Tab.1 Clinicopathological characteristics and univariate analysis of 83 TNBC patients
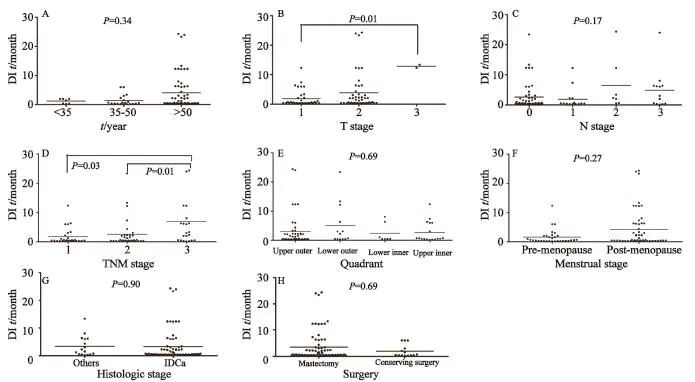
图1 DI的分组散点图Fig.1 Grouped scatter plot of DI
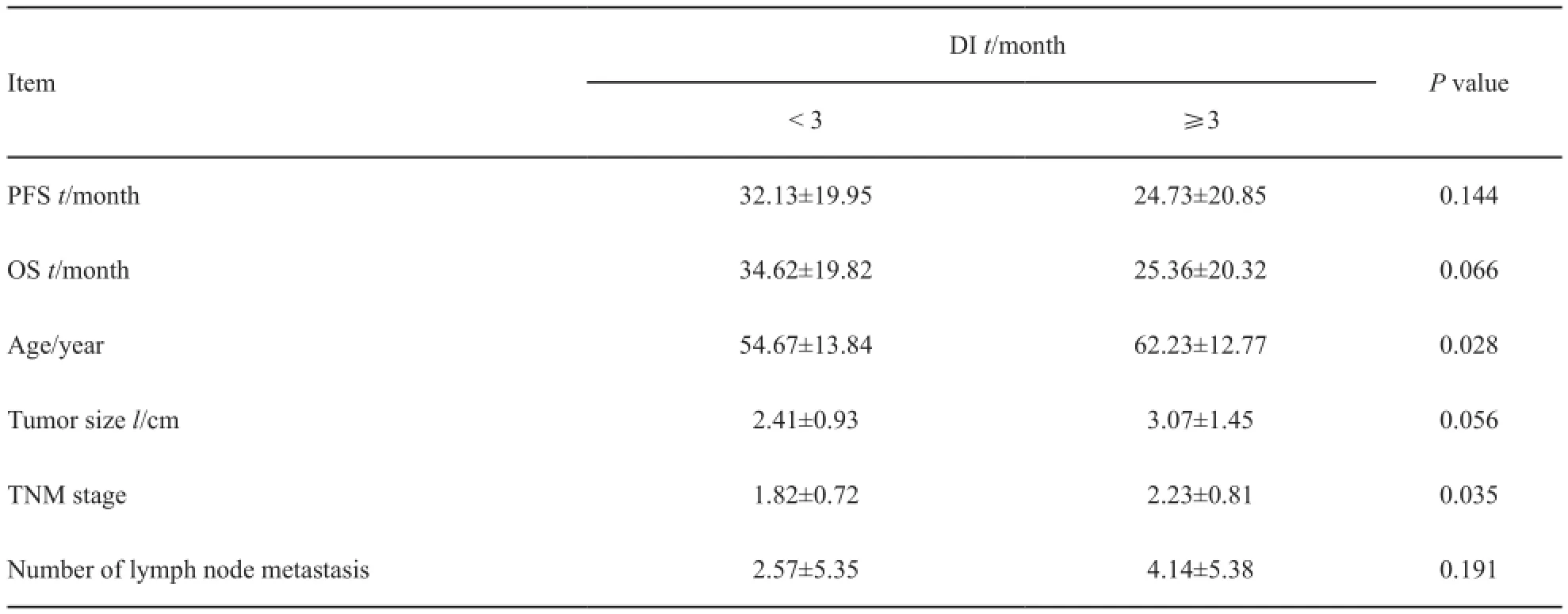
表2 DI的分组分析Tab.2 Grouped analysis of DI
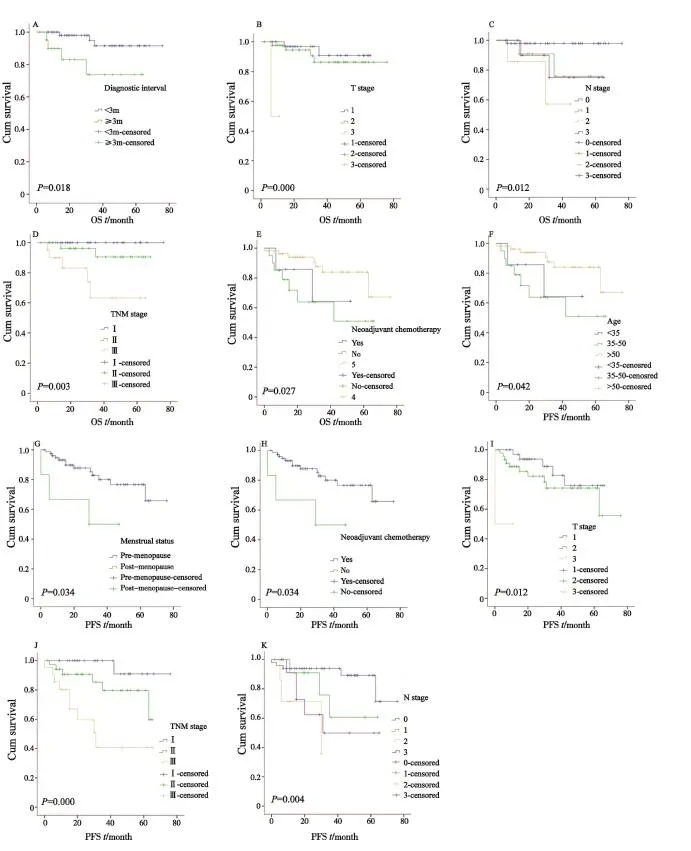
图2 生存曲线Fig.2 Survival curve
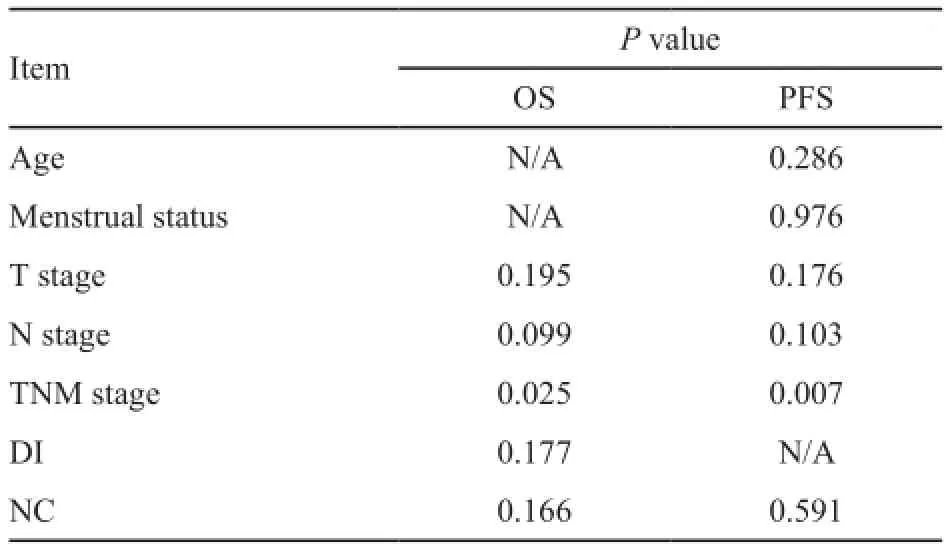
表3 OS和PFS的多因素分析Tab.3 Multivariate analysis of possible factors with OS and PFS
3 讨 论
有文献将DI分为患方延迟(从发现症状到寻医就诊的时间)和医方延迟(从首次就诊到确诊或起始治疗的时间)[18]。研究表明,患方延迟与进展期获诊(即诊断时疾病已是进展期)和不良预后相关[19-20],医方延迟的相关研究较少。我们的入组患者就诊后3~5 d即获确诊(手术或穿刺活检),医方延迟差异不明显,因此未予分析。
TNBC患者的治疗需要手术和辅助治疗(如放化疗)密切配合。因此,除DI之外,辅助治疗延迟(adjuvant treatment delay,AD)也值得关注,即从手术结束到辅助治疗开始的时间。De Melo Gagliato等[21]研究发现,对于乳腺癌患者来说,AD≥2个月会对OS产生影响。Trufelli等[22]研究发现,AD每延长1个月,浸润性乳腺癌患者的死亡风险提高1.3倍,并且AD是其独立危险因素。但也有文献表明,AD不会影响患者的生存率[23-24]。本研究入组的患者,术后均立即接受了辅助治疗,因此AD这一指标并未纳入考量。考虑到本研究数据来源机构所在地的特殊性(地处上海,诊疗比较规范),而我国又是一个医疗水平发展很不平衡的国家,因此对于中国大多数TNBC患者群体来说,其生存研究中应该对AD这一指标给予足够的重视。
本研究统计分析还显示,TNM分期是OS和PFS的独立影响因素。分期越高,PFS和OS越短,预后越差。相比普通类型乳腺癌,TNBC诊断时分期通常较晚,远处转移风险也较高。一旦转移,主要疗法还是全身化疗。然而,目前针对转移性TNBC的一线化疗方案效果并不理想,这也是此类患者预后差的原因之一。最近,Hu等[25]研究发现,与传统治疗方案相比,顺铂联合吉西他滨可延长转移性TNBC患者的中位PFS。并且,以顺铂代替紫杉醇作为转移性TNBC的一线治疗用药,在不明显增加化疗相关不良反应的同时,还可以减轻患者的经济负担,从而有利于增加患者的治疗依从性。
早诊断、早治疗对肿瘤患者的综合管理十分重要,其关键就是缩短DI。本研究为期0.67个月的DI值暂无法与其他TNBC患者群体的DI数据进行比较,因为国内外尚未见相关报道。然而目前,DI在其他肿瘤患者群体中的研究已经开展。Din等[8]对15种常见肿瘤进行研究发现,中位DI较短的肿瘤包括乳腺癌(27 d)、睾丸癌(41 d)和胰腺癌(59 d),较长的包括骨髓瘤(149 d)、肺癌(113 d)和白血病(102 d)。在乳腺癌、膀胱癌和宫颈癌中,诊断之前出现“NICE症状”者DI较短。“NICE症状”指与癌症可疑相关的、需要急迫处理(比如就诊)的症状[26]。对于乳腺癌来说,“NICE症状”包括乳腺肿块、乳腺皮肤改变、橘皮样变、乳头溢液或出血和单侧乳头湿疹;“non-NICE症状”包括乳腺疼痛、贫血、厌食、乏力和体重下降[8]。本研究并未以初诊症状为分组要素对DI进行统计学分析,因为本研究入组的患者均是以“NICE症状”为首诊原因。或许由于“non-NICE症状”缺乏特异性,患者不易因此就诊,导致就诊者以“NICE症状”为主。
本研究在国内首次对TNBC群体的DI及其与疾病预后的关系进行了分析。结果显示:①T3期患者的DI>T1期,Ⅲ期患者>Ⅱ期和Ⅰ期,理论上讲,T分期和TNM分期较晚者,症状应该更明显,其DI应该较短,然而我们的结论与之不符,原因可能是T3期和Ⅲ期患者病例数较少,且T3期和Ⅲ期患者平均年龄较大,该人群对症状重视程度不够;② DI<3个月组与DI≥3个月组相比,前者平均确诊年龄和TNM分期均早于后者,通常年轻患者群体对症状重视程度较高、就诊意识较强,因而DI较短,由于及时就诊,获诊时的TNM分期也较早;③ T分期、N分期、新辅助化疗、TNM分期和DI是OS的影响因素,确诊年龄、T分期、N分期、TNM分期、月经状态和新辅助化疗是PFS的影响因素,其中,TNM分期是OS和PFS的独立影响因素。这一结果再次强调了TNM分期对疾病诊治的重要价值。
[参考文献]
[1] FOROUZANFAR M H, FOREMAN K J, DELOSSANTOS A M, et al. Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis [J]. Lancet, 2011,378(9801): 1461-1484.
[2] FOULKES W D, SMITH I E, REIS-FILHO J S. Triplenegative breast cancer [J]. N Engl J Med, 2010, 363(20):1938-1948.
[3] DENT R, TRUDEAU M, PRITCHARD K I, et al. Triplenegative breast cancer: clinical features and patterns of recurrence [J]. Clin Cancer Res, 2007, 13(15): 4429-4434. [4] KASSAM F, ENRIGHT K, DENT R, et al. Survival outcomes for patients with metastatic triple-negative breast cancer:implications for clinical practice and trial design [J]. Clin Breast Cancer, 2009, 9(1): 29-33.
[5] ARRIAGADA R, LE M G, DUNANT A, et al. Twenty-five years of follow-up in patients with operable breast carcinoma [J]. Cancer, 2006, 106(4): 743-750.
[6] FAN Y P, LIU C L, CHIANG I J, et al. Development of a prognostic nomogram for identifying those factors which influence the 2- and 5-year survival chances of Taiwanese women diagnosed with breast cancer [J]. Eur J Cancer Care (Engl), 2011, 20(5): 620-626.
[7] SCHMIDT M, VICTOR A, BRATZEL D, et al. Long-term outcome prediction by clinicopathological risk classification algorithms in node-negative breast cancer--comparison between Adjuvant!, St Gallen, and a novel risk algorithm used in the prospective randomized Node-Negative-Breast Cancer-3 (NNBC-3) trial [J]. Ann Oncol, 2009, 20(2):258-264.
[8] DIN N U, UKOUMUNNE O C, RUBIN G, et al. Age and gender variations in cancer diagnostic intervals in 15 cancers: analysis of data from the UK Clinical Practice Research Datalink [J]. PLoS One, 2015, 10(5): e0127717.
[9] NEAL R D, DIN N U, HAMILTON W, et al. Comparison of cancer diagnostic intervals before and after implementation of NICE guidelines: analysis of data from the UK General Practice Research Database [J]. Br J Cancer, 2014, 110(3):584-592.
[10] TØRRING M L, FRYDENBERG M, HANSEN R P, et al. Time to diagnosis and mortality in colorectal cancer: a cohort study in primary care [J]. Br J Cancer, 2011, 104(6): 934-940.
[11] RICHARDS M A, WESTCOMBE A M, LOVE S B, et al. Influence of delay on survival in patients with breast cancer:a systematic review [J]. Lancet, 1999, 353(9159): 1119-1126.
[12] WELLER D, VEDSTED P, RUBIN G, et al. The Aarhus statement: improving design and reporting of studies on early cancer diagnosis [J]. Br J Cancer, 2012, 106(7): 1262-1267.
[13] LYRATZOPOULOS G, NEAL R D, BARBIERE J M, et al. Variation in number of general practitioner consultations before hospital referral for cancer: findings from the 2010 National Cancer Patient Experience Survey in England [J]. Lancet Oncol, 2012, 13(4): 353-365.
[14] NEAL R D, ALLGAR V L. Sociodemographic factors and delays in the diagnosis of six cancers: analysis of data from the “National Survey of NHS Patients: Cancer” [J]. Br J Cancer, 2005, 92(11): 1971-1975.
[15] ALLRED D C, CARLSON R W, BERRY D A, et al. NCCN Task Force Report: estrogen receptor and progesterone receptor testing in breast cancer by immunohistochemistry [J]. J Natl Compr Canc Netw, 2009, 7(Suppl 6): S1-S21.
[16] HAMMOND M E H, HAYES D F, DOWSETT M, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer[J]. J Clin Oncol, 2010, 28(16):2784-2795.
[17] HAMMOND M E H. ASCO-CAP guidelines for breast predictive factor testing: an update [J]. Appl Immunohistochem Mol Morphol, 2011, 19(6): 499-500.
[18] UNGER-SALDAÑA K. Challenges to the early diagnosis and treatment of breast cancer in developing countries [J]. World J Clin Oncol, 2014, 5(3): 465-477.
[19] RICHARDS M A, WESTCOMBE A M, LOVE S B, et al. Influence of delay on survival in patients with breast cancer:a systematic review [J]. Lancet, 1999, 353(9159): 1119-1126.
[20] UNGER-SALDAÑA K, INFANTE-CASTAÑEDA C. Delay of medical care for symptomatic breast cancer: a literature review [J]. Salud Publica Mex, 2009, 51(Suppl 2): s270-s285.
[21] DE MELO GAGLIATO D, GONZALEZ-ANGULO A M, LEIX, et al. Clinical impact of delaying initiation of adjuvant chemotherapy in patients with breast cancer [J]. J Clin Oncol, 2014, 32 (8): 735-744.
[22] TRUFELLI D C, MATOS L L, SANTI P X, et al. Adjuvant treatment delay in breast cancer patients [J]. Rev Assoc Med Bras, 2015, 61(5): 411-416.
[23] ELMORE J G, NAKANO C Y, LINDEN H M, et al. Racial inequities in the timing of breast cancer detection, diagnosis,and initiation of treatment [J]. Med Care, 2005, 43(2): 141-148.
[24] HERSHMAN D, MCBRIDE R, JACOBSON J S, et al. Racial disparities in treatment and survival among women with earlystage breast cancer [J]. J Clin Oncol, 2005, 23(27): 6639-6646.
[25] HU X C, ZHANG J, XU B H, et al. Cisplatin plus gemcitabine versus paclitaxel plus gemcitabine as first-line therapy for metastatic triple-negative breast cancer (CBCSG006): a randomised, open-label, multicentre, phase 3 trial [J]. Lancet Oncol, 2015, 16(4): 436-446.
[26] National Institute for Health and Clinical Excellence (Great Britain). Referral guidelines for suspected cancer: quick reference guide[M]. National Institute for Health and Clinical Excellence, 2005.
DOI:10.19401/j.cnki.1007-3639.2016.06.010
中图分类号:R737.9
文献标志码:A
文章编号:1007-3639(2016)06-0538-08
收稿日期:(2016-01-15 修回日期:2016-03-17)
通信作者:沈 赞 E-mail:sshenzzan@vip.sina.com
The infuence of diagnostic interval and other clinicopathological factors on the prognosis of triple-negative breast cancer
SUN Chu, LI Hongtao, LIU Zimei, YUAN Yuan, SHEN Zan
(Department of Oncology, Sixth People's Hospital, Shanghai Jiao Tong University, Shanghai 200233, China)Correspondence to: SHEN Zan E-mail: sshenzzan@vip.sina.com
[Abstract]Background and purpose: The time from frst onset of symptoms or signs to a defnitive diagnosis is defned as diagnostic interval (DI). The relation of DI to other clinicopathological parameters and the impact of DI on prognosis of patients with triple-negative breast cancer (TNBC) remain unclear. This article plans to make an intensive study of these questions. Methods: The clinical records of a series of 83 consecutively presenting unselected patients referred to the Shanghai Sixth People's Hospital with diagnosed TNBC between September 2009 and September 2015 were retrospectively reviewed. Clinical and pathological factors included were investigated by univariate analysis using the Kaplan-Meier method, the factors associated with prognosis were further evaluated by multivariable analysis with Cox progression model. t-test and Kruskal-Wallis test were used to study the correlation between DI and other characters. Results: DI: stage T3>T1(P=0.01), stage Ⅲ>Ⅱ (P=0.03) and Ⅰ (P=0.01). Compared with patients of DI≥3 months, the <3 months group had earlier age (P=0.028) and TNM stage (P=0.035). T stage, N stage, neoadjuvant chemotherapy, TNM stage and DI are infuencing factors of overall survival (OS). Age, T stage, N stage, TNM stage,menstrual status and neoadjuvant chemotherapy are infuencing factors of progression-free survival (PFS). TNM staging is an independent infuencing factor for OS and PFS. Conclusion: Patients with later disease stage were more likely to have a longer DI; The shorter DI, the earlier age and stage of disease; DI is the infuence factor of OS; TNM stage is an independent infuencing factor for OS and PFS.
[Key words]Diagnostic interval; Triple-negative breast cancer; Survival analysis