起源于左冠状动脉窦及右冠状动脉窦的室性早搏心电图特征分析及射频消融治疗
谭红伟 张旭敏 邹 誉 周 建 李 莹 邱建平 刘学波
·临床研究·
起源于左冠状动脉窦及右冠状动脉窦的室性早搏心电图特征分析及射频消融治疗
谭红伟张旭敏邹誉周建李莹邱建平刘学波
200120上海,同济大学附属东方医院心内科
【摘要】目的:比较左冠状动脉窦及右冠状动脉窦起源的室性早搏(室早)心电图特征。方法:入选成功行主动脉根部室早消融的患者20例,按消融部位分为左冠状动脉窦室早组(LCC组)15例、右冠状动脉窦室早组(RCC组)5例,比较两组心电图特征。结果:RCC组患者Ⅰ导联均为R波;LCC组患者Ⅰ导联4例为QS波,10例为RS或rs波,1例为R波(χ2=16.80,P<0.01)。与RCC组比较,LCC组患者Ⅲ导联R波振幅增高 [(2.01± 0.45) mV对(1.45± 0.33) mV, P<0.05]、 aVL导联QS波振幅加深[(1.20± 0.24) mV 对(0.65± 0.21) mV, P<0.01]、R波振幅Ⅲ/Ⅱ比值及QS波振幅aVL/aVR比值增大 (1.09± 0.12 对 0.80± 0.12,P<0.001; 1.31±0.35 对 0.60±0.24, P<0.001)、Ⅰ导联QRS波时限缩短[(78± 32) ms 对(120± 13) ms,P<0.05]、aVL导联QRS波时限延长 [(128±14) ms 对(100±24) ms, P<0.05]。除1例患者因起源点临近左冠状动脉开口而放弃消融外,其余均消融成功。平均随访(13 ± 6)个月,无复发病例及并发症。结论:对于体表心电图提示室早起源于左室流出道的患者,Ⅰ导联R波提示RCC室早,Ⅰ导联RS或rs波提示LCC室早;与RCC室早相比,LCC室早Ⅲ导联R波振幅较高、aVL导联QS波振幅较大、R波振幅Ⅲ/Ⅱ比值及QS波振幅aVL/aVR比值增大。
【关键词】室性早搏;射频消融;主动脉根部;心电图
Electrocardiography
特发性室性心律失常包括室性早搏(室早)及室性心动过速(室速),主要起源于右室流出道,左室流出道也是其好发部位之一[1-2]。研究显示左室流出道特发性室性心律失常最常见的部位是主动脉窦部,少部分起源于左室间隔、二尖瓣环或左室顶部[3-6]。本研究对左冠状动脉窦(left coronary cusp, LCC)及右冠状动脉窦(right coronary cusp, RCC)起源室早的心电图特征进行比较,探讨体表心电图鉴别LCC及RCC室早的价值。
1对象与方法
1.1研究对象
入选2013年1月至2015年6月在我院行主动脉根部室早射频消融治疗的患者20例,其中男性5例,平均年龄(56±16)岁。入选标准:(1)年龄>18岁;(2)术前体表心电图及24 h动态心电图(holter)均为频发单形性室早;(3)有心悸、胸闷等症状,服用1种以上抗心律失常药物疗效不佳;(4)体表心电图胸导联移行在V3或V3以前;(5)术前体格检查、胸片、超声心动图除外器质性心脏病。
1.2心电图分析
记录所有患者窦性心律及室早的12导联同步心电图,走纸速度100 mm/s。记录心电图时确保V1及V2导联位于第4肋间以减少对体表心电图特征的影响[7]。分析室早QRS波特征,指标包括:(1)QRS波时限;(2)下壁导联(Ⅱ、Ⅲ、aVF)及Ⅰ导联R波振幅、时限及R波振幅Ⅲ/Ⅱ比值;(3)aVL、aVR导联QS波振幅、时限及QS波振幅aVL/aVR比值;(4)胸导联V1~V6 R波及S波振幅及时限。Q、R、S指相对高振幅的波(>5 mm),q、r、s指相对低振幅的波(≤5 mm)。QRS波时限指从12导联同步记录心电图中QRS波群最早点测量至最晚点的时间。
1.3心内电生理检查和导管射频消融
所有患者在停服抗心律失常药物5个半衰期后行心内电生理检查。如患者无自发室早,则静脉滴注异丙肾上腺素诱发。室早稳定出现后,即开始电生理标测。所有患者均在Carto 3系统指导下行室早激动标测及起搏标测。先经右侧股静脉穿刺,行右室流出道激动标测。消融靶点选择标准为:局部激动领先体表心电图室早QRS波起点至少20 ms以上和(或)起搏时至少11~12个导联心电图QRS波形态与自发室早完全相同[8]。消融靶点确定后,采用冷盐水灌注消融导管,设置温度43 ℃,功率30 W,盐水流速20 mL/min试放电消融20 s。如该靶点消融有效,则继续放电消融60~100 s,否则重新行激动标测及起搏标测。如右室流出道未发现理想靶点或右室流出道消融无效,则行心大静脉及左室流出道激动标测。如激动标测提示主动脉瓣上领先,则行选择性冠状动脉造影明确消融导管与左右冠状动脉开口的关系,确保消融导管与左右冠状动脉开口之间的距离>5 mm[9-10]。主动脉根部消融能量设置与右室流出道相同。
消融成功标准为:反复多部位、多程序刺激均不能诱发与消融前形态一致的早搏;静脉滴注异丙肾上腺素不能诱发与消融前形态一致的室早;观察20~30 min,无自主出现的与消融前形态一致的室早。
1.4随访
所有患者术后服用阿司匹林100 mg/d,服用1个月。消融术后心电监护24 h,次日复查动态心电图。消融术后1个月、6个月门诊随诊,根据患者症状、心电图和(或)动态心电图结果判定是否复发。
1.5统计学分析
应用SPSS 16.0软件进行统计学分析。计量资料以均数±标准差表示,两组间均数比较采用独立样本t检验;计数资料以率表示,率的比较采用χ2检验。以P<0.05为差异有统计学意义。
2结果
2.1临床特征
本研究共入选20例经射频消融治疗证实起源于主动脉根部室早患者,其中LCC组15例,RCC组5例,所有患者均无器质性心脏病证据(见表1)。
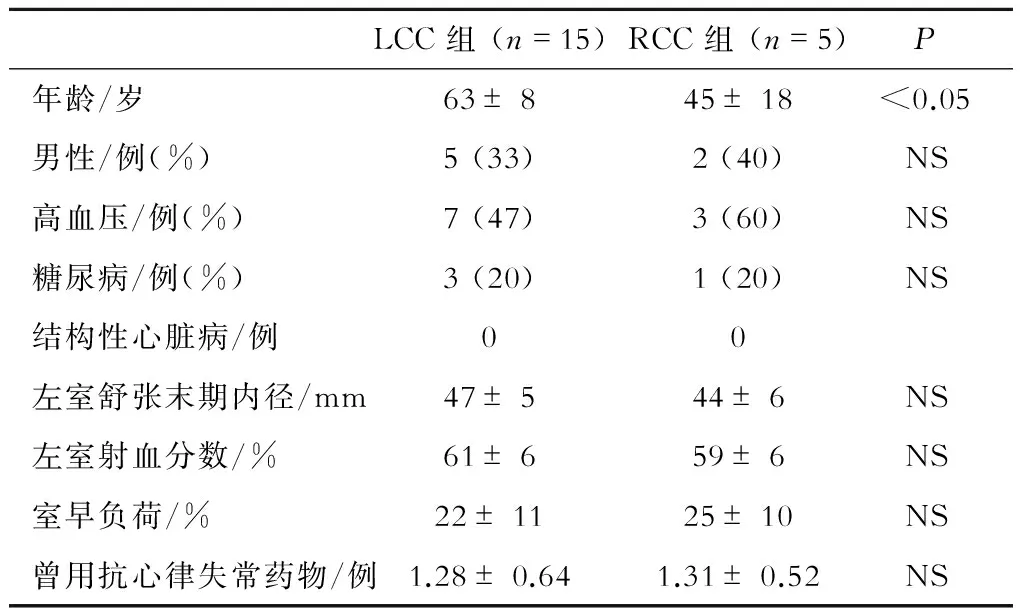
表1 两组患者临床特征比较
注:NS为差异无统计学意义(以下相同)
2.2 心电图特征比较
所有患者下壁导联(Ⅱ、Ⅲ、aVF)均为R波,aVL及aVR导联均为QS波。RCC组患者Ⅰ导联均为R波;LCC组患者Ⅰ导联4例为QS波,10例为RS或rs波,1例为R波(χ2=16.80,P<0.01)。RCC组患者V1导联2例为QS波,4例为rS波;LCC组患者V1导联4例为QS波,7例为rS波3例为qrS波,1例为R波。
与RCC组比较,LCC组Ⅲ导联R波振幅增高 [(2.01± 0.45) mV 对 (1.45± 0.33) mV,P<0.05];与RCC组比较,LCC组aVL导联QS波振幅加深 [(1.20±0.24) mV 对 (0.65±0.21) mV,P<0.01];与RCC组比较,LCC组R波振幅Ⅲ/Ⅱ比值及QS波振幅aVL/aVR比值增大 (1.09± 0.12 对0.80± 0.12,P<0.001;1.31±0.35 对0.60±0.24,P<0.001)(见表2)。
两组QRS波时限比较无显著性差异。与RCC组比较,LCC组Ⅰ导联QRS波时限缩短[(78± 32) ms 对(120± 13) ms,P<0.05];与RCC组比较,LCC组aVL导联QRS波时限显著延长 [(128±14) ms 对 (100±24) ms,P<0.05],见表2、3 。
典型的LCC室早和RCC室早体表心电图见图1。
2.3消融结果
本研究中,除1例患者因室早起源点距左冠状动脉开口<5 mm,放弃消融外,其余患者均成功消融室早。术中及术后无严重并发症。
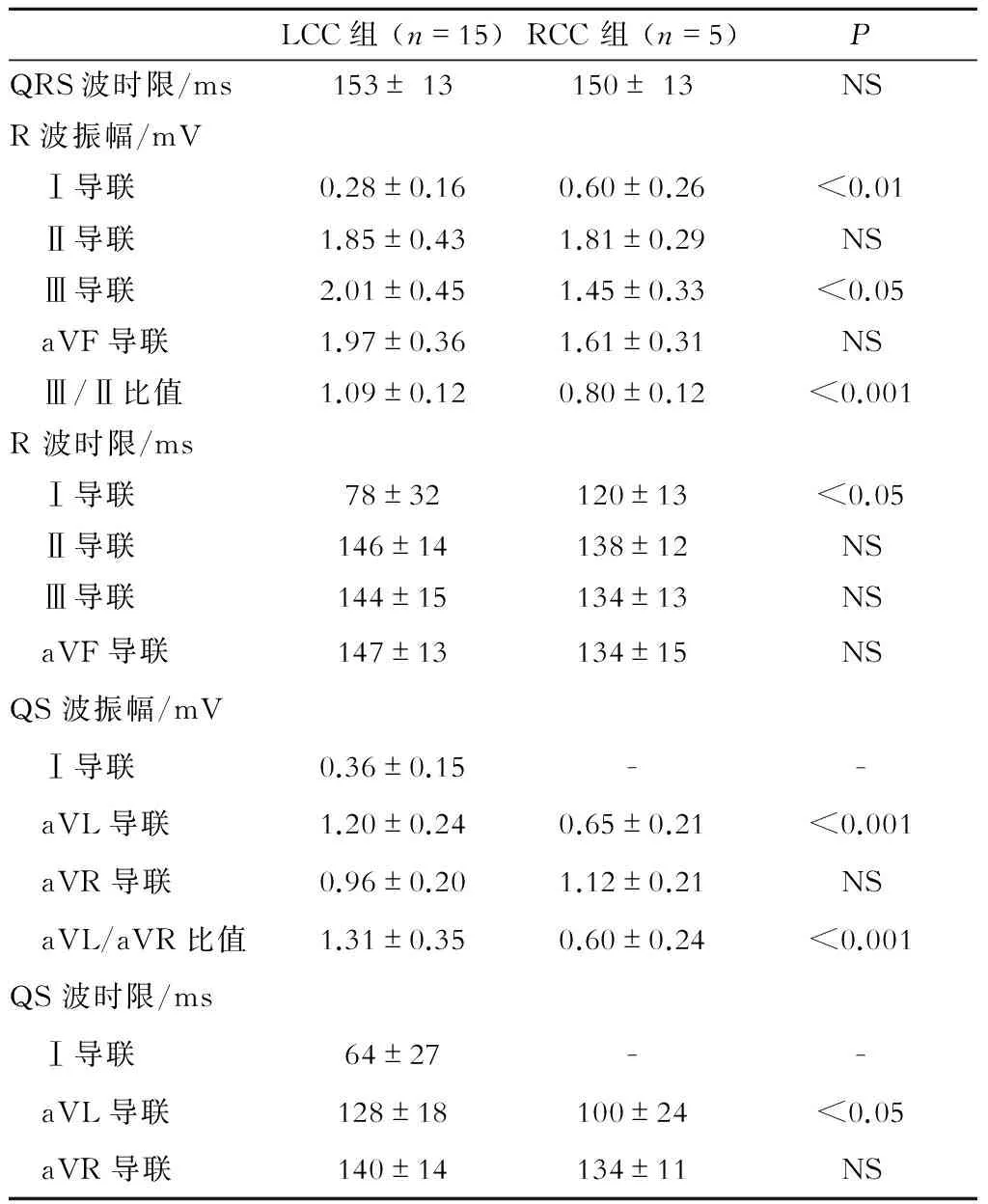
表2 两组患者心电图肢体导联指标比较
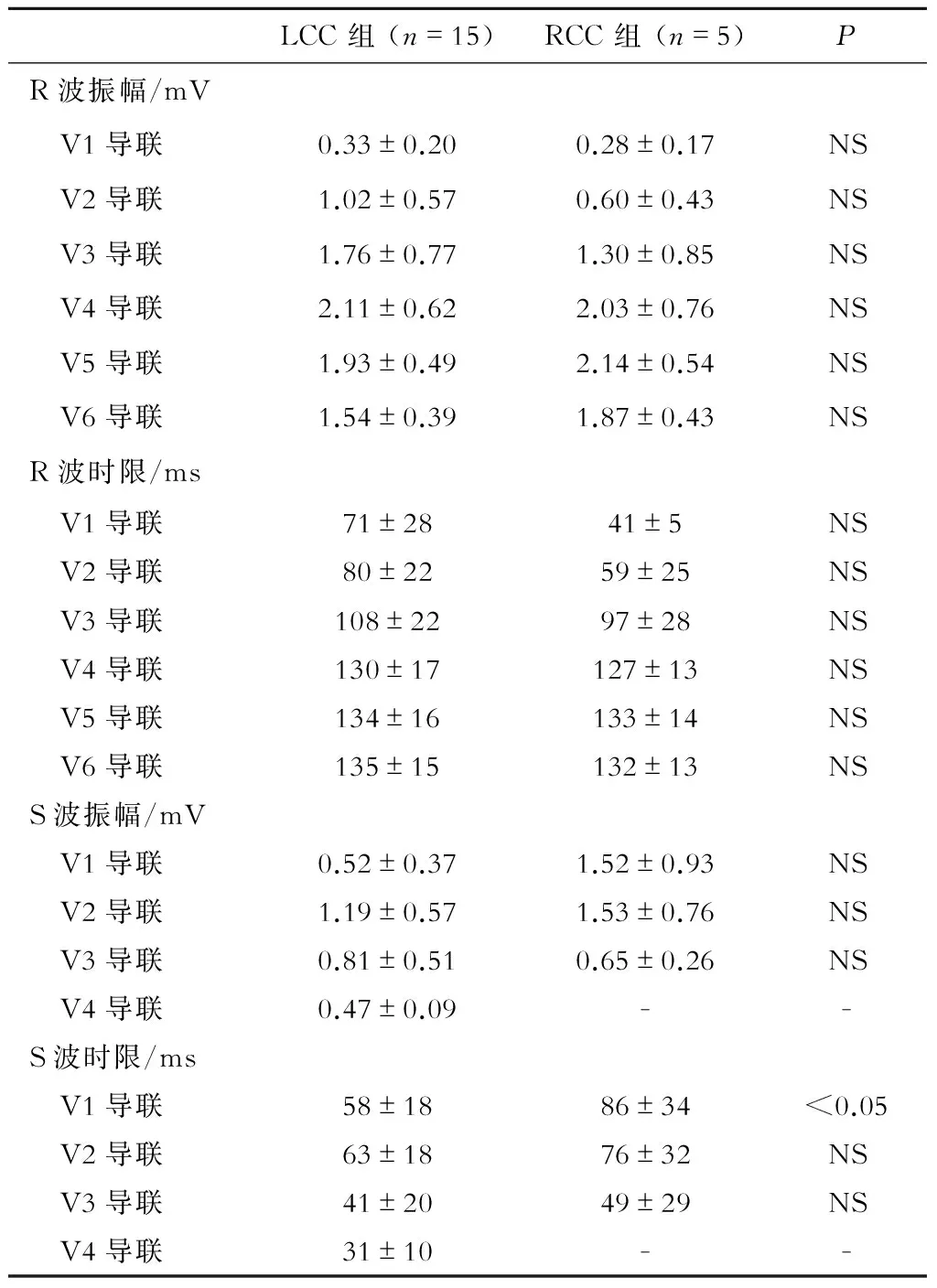
表3 两组患者心电图胸导联指标比较

注:A为LCC室早体表心电图, Ⅰ导联呈RS型,aVL/aVR>1.00;B为RCC室早体表心电图, Ⅰ导联呈R型,aVL/aVR<1.00
2.4随访结果
术后超声心动图检查显示主动脉瓣及瓣下结构与功能均未受影响。门诊平均随访(13 ± 6)个月,无复发病例,无并发症发生。
3讨论
本研究入选20例体表心电图怀疑左室流出道起源室早的患者,结合射频消融最终靶点,分析左冠窦及右冠窦起源的室早的心电图特征,结果发现:(1)Ⅰ导联R波提示RCC室早,Ⅰ导联出现S或s波提示LCC室早;(2)与RCC室早相比,LCC室早Ⅲ导联R波振幅较高、aVL导联QS波振幅较大、R波振幅Ⅲ/Ⅱ比值及QS波振幅aVL/aVR比值增大;(3)经导管射频消融治疗LCC及RCC室早是一种安全、有效的方法。
LCC与RCC室早具有不同心电图特征,与其解剖有关。主动脉根部位于心脏中心,由3个瓦氏窦组成,LCC及RCC与室间隔肌部相邻,而无冠窦位于左右房之间,与房间隔相邻[11-12]。研究证实,心室肌延伸到主动脉或肺动脉-心室连接部以上,这些心室肌延伸可能是室早消融的靶点[12-13]。本研究发现RCC室早Ⅰ导联均为R波,而LCC室早Ⅰ导联均有S或s波;LCC室早Ⅲ导联R波振幅及aVL导联QS波振幅增加,其原因可能为LCC较RCC的位置更高,且更偏左。
体表心电图具有无创、简便等特点,对于室早导管消融具有重要指导价值。Ouyang等[11]发现,V1、V2导联R/S比值及R波时限能较准确区分右室流出道室早与主动脉根部室早。Lin等[14]发现,LCC室早胸导联移行在V2导联,而RCC室早一般在V3。这些指标也可以简便、较准确地区分室早起源,但由于胸导联受电极贴片位置影响较大,有局限性[7]。本研究发现对体表心电图提示室早可能起源于主动脉根部患者,Ⅰ导联R波提示RCC室早,Ⅰ导联RS或rs波提示LCC室早;Ⅲ导联R波振幅较高、aVL导联QS波振幅较深、R波振幅Ⅲ/Ⅱ比值及QS波振幅aVL/aVR比值增大提示室早起源于LCC。
本研究的局限性:(1)样本量较小;(2)未纳入无冠窦室早(无冠窦起源室早较少[10]);(3)未使用术中心腔内超声检查,仅通过术中影像学检查无法准确定位部分起源于LCC和RCC交界处室早[15]。
参考文献
[1]Prystowsky EN, Padanilam BJ, Joshi S, et al. Ventricular arrhythmias in the absence of structural heart disease [J]. J Am Coll Cardiol, 2012, 59(20):1733-1744.
[2]Chun KR, Satomi K, Kuck KH, et al. Left ventricular outflow tract tachycardia including ventricular tachycardia from the aortic cusps and epicardial ventricular tachycardia [J]. Herz, 2007, 32(3):226-232.
[3]Lin CY, Chung FP, Lin YJ, et al. Radiofrequency catheter ablation of ventricular arrhythmias originating from the continuum between the aortic sinus of Valsalva and the left ventricular summit: Electrocardiographic characteristics and correlative anatomy [J]. Heart Rhythm, 2016, 13(1):111-121.
[4]Yamada T, Litovsky SH, Kay GN. The left ventricular ostium: an anatomic concept relevant to idiopathic ventricular arrhythmias [J]. Circ Arrhythm Electrophysiol, 2008, 1(5):396-404.
[5]罗庆志,金奇,吴立群. 频发室性早搏所致心肌病的电生理特征及其处理 [J]. 国际心血管病杂志, 2014,40(3): 137-139.
[6]宋卫锋,张嘉莹,吴晓羽,等. Carto-3指导下射频消融治疗左室特发性室性心动过速体会 [J]. 国际心血管病杂志, 2014,40(2): 131-133.
[7]Anter E, Frankel DS, Marchlinski FE, et al. Effect of electrocardiographic lead placement on localization of outflow tract tachycardias [J]. Heart Rhythm, 2012, 9(5):697-703.
[8]Yoshida N, Yamada T, McElderry HT, et al. A novel electrocardiographic criterion for differentiating a left from right ventricular outflow tract tachycardia origin: the V2S/V3R index [J]. J Cardiovasc Electrophysiol, 2014, 25(7):747-753.
[9]Yamada T, McElderry HT, Doppalapudi H, et al. Idiopathic ventricular arrhythmias originating from the aortic root: prevalence, electrocardiographic and electrophysiologic characteristics, and results of radiofrequency catheter ablation [J]. J Am Coll Cardiol, 2008, 52(2):139-147.
[10]Yamada T, Lau YR, Litovsky SH, et al. Prevalence and clinical, electrocardiographic, and electrophysiologic characteristics of ventricular arrhythmias originating from the noncoronary sinus of Valsalva [J]. Heart Rhythm, 2013, 10(11):1605-1612.
[11]Ouyang F, Fotuhi P, Ho SY, et al. Repetitive monomorphic ventricular tachycardia originating from the aortic sinus cusp: electrocardiographic characterization for guiding catheter ablation [J]. J Am Coll Cardiol, 2002, 39(3):500-508.
[12]ada H. Catheter ablation of tachyarrhythmias from the aortic sinuses of Valsalva—when and how? [J].Circ J, 2012, 76(4):791-800.
[13]Hasdemir C, Aktas S, Govsa F, et al. Demonstration of ventricular myocardial extensions into the pulmonary artery and aorta beyond the ventriculo-arterial junction [J]. Pacing Clin Electrophysiol, 2007, 30(4):534-539.
[14]Lin D, Ilkhanoff L, Gerstenfeld E, et al. Twelve-lead electrocardiographic characteristics of the aortic cusp region guided by intracardiac echocardiography and electroanatomic mapping [J]. Heart Rhythm, 2008, 5(5):663-669.
[15]Bala R, Garcia FC, Hutchinson MD, et al. Electrocardiographic and electrophysiologic features of ventricular arrhythmias originating from the right/left coronary cusp commissure [J]. Heart Rhythm, 2010,7(3):312-322.
(收稿:2016-02-21修回:2016-04-25)
(本文编辑:梁英超)
·基础研究·
通信作者:刘学波,Email:lxb70@hotmail.com
doi:10.3969/j.issn.1673-6583.2016.03.012
Electrocardiographic characteristics and radiofrequency catheter ablation of premature ventricular contractions originating from left and right coronary cusp
TANHongwei,ZHANGXumin,ZOUYu,ZHOUJian,LIYing,QIUJianping,LIUXuebo.
DepartmentofCaridology,ShanghaiEastHospitalaffiliatedtoTongjiUniversity,Shanghai200120,China
【Abstract】Objective:This study was undertaken to compare the electrocardiography characteristics of premature ventricular contractions (PVCs) from left coronary cusp (LCC) and right coronary cusp RCC. Methods:We studied 20 consecutive patients who underwent successful catheter ablation for PVCs originating from LCC (n=15) and RCC (n=5). Characteristics of 12-lead ECG were analyzed. Results:All patients with RCC PVCs presented R morphology in lead Ⅰ, whereas in patients with LCC PVCs, 4 presented QS morphology, 10 presented RS or rs and 1 presented R morphology (P<0.01). The R wave amplitude in lead Ⅲ were significantly higher [(2.01± 0.45) mV vs. (1.45± 0.33) mV, P<0.05] and the Q wave amplitude in aVL were significantly deeper [(1.20± 0.24) mV vs. (0.65± 0.21) mV, P<0.01] in patients with LCC PVCs than that in patients with RCC PVCs. Compared with RCC PVCs, the Ⅲ/Ⅱ ratio of R wave amplitude and aVL/aVR ratio of QS wave amplitude were significantly larger in patients with LCC PVCs (1.09± 0.12 vs. 0.80± 0.12; 1.31±0.35 vs. 0.60±0.24, both P<0.001).The QRS duration was significantly shorter in lead I [(78± 32) ms vs. (120± 13) ms, P<0.05] and longer in lead aVL [(128±14) ms vs. (100±24) ms, P<0.05] in patients with LCC PVCs than that in patients with RCC PVCs. The ablation procedures succeeded in all patients except far one whose ablation was not performed because the origin of the PVCs was identified close to the ostium of left coronary artery. There were no major procedural complications. No patient developed PVCs recurrence during a mean follow-up of (13 ± 6) months. Conclusion:In patients with left ventricular out-flow tract PVCs, a relatively large R wave in lead Ⅰ is seen in RCC PVCs while RS or rs wave in lead Ⅰ seen in LCC PCVCs. LCC PVCs shows higher R wave in lead Ⅲ, deeper Q wave in aVL, higher Ⅲ/Ⅱ ratio of R wave amplitude and aVL/aVR ratio of QS wave amplitude.
【Key words】Premature ventricular contractions; Radiofrequency ablation; Aortic root;