Identifying disparity in emergency department length of stay and admission likelihood
Sean Wilson, Sharmistha Dev, Meredith Mahan, Manu Malhotra, Joseph MillerEmergency Medicine, University of California, Irvine, Orange, California 9868, USAEmergency Medicine, Henry Ford Hospital, Detroit, Michigan 480, USACorresponding Author: Sean Wilson, Email: wilsonseanpatrick@gmail.com
Identifying disparity in emergency department length of stay and admission likelihood
Sean Wilson1, Sharmistha Dev2, Meredith Mahan2, Manu Malhotra2, Joseph Miller21Emergency Medicine, University of California, Irvine, Orange, California 92868, USA2Emergency Medicine, Henry Ford Hospital, Detroit, Michigan 48202, USA
Corresponding Author: Sean Wilson, Email: wilsonseanpatrick@gmail.com
BACKGROUND: To assess whether insurance status has an effect on emergency department (ED) length of stay (LOS) and likelihood for admission or transfer to an operating room.
METHODS: This was a retrospective cross-sectional study of all encounters from January 2011 through October 2013 at an urban, academic trauma center. Analysis included multi-variable linear regression for ED LOS and logistic regression for the likelihood of admission.
RESULTS: Overall, 201 535 patients met the inclusion criteria, for which the mean age was 43.8 years, 55.9% were female, 23.4% were uninsured and 8% were of non-black race. Admission rate was 24.5% and operative rate was 1.4%. After adjusting for age, sex, triage acuity and race,the presence of insurance coverage was associated with an increased ED LOS of 575 (95%CI 552–598) vs. 567 (95%CI 543–591) minutes (P<0.01) among admitted patients and a decreased ED LOS of 456 (95%CI 381–531) vs. 499 (95%CI 423–575) minutes (P<0.01) among those transferred to an operating room. Adjusting for these same predictors, insured status remained a predictor for admission (odds ratio 1.24, 95%CI 1.20–1.28, P<0.01) and a negative predictor for transfer to the operating room (odds ratio 0.84, 95%CI 0.77–0.92, P<0.01).
CONCLUSION: The insured experienced a clinically insignificant increase in ED LOS when admitted and a 43-minute decrease in ED LOS when being transferred to the operating room. The insured were more likely to be admitted and less likely to be transferred to an operating room.
KEY WORDS:Emergency department; Health disparities; Racial disparities; Insurance
World J Emerg Med 2016;7(2):111–116
INTRODUCTION
Over the last decade, the emergency department (ED) has become an increasingly important entity in the healthcare delivery system and is now considered the primary gateway for inpatient admissions.[1]As the number of annual visits increases year after year, so has the ED length of stay (LOS) and as such, is now being tracked as a quality indicator and used as a metric for departmental efficiency.[2–5]Both patient and health system factors potentially impact ED LOS, with several studies previously addressing such factors. Racial disparities have been identified with patients of black race and Latino ethnicity experiencing longer ED LOS when compared to those of white race.[6–9]Increased use of diagnostic imaging studies, such as computed tomography and magnetic resonance imaging, as well as metropolitan hospital location have also been identified as factors that increase ED LOS.[8–9]Lastly, patients suffering from myocardial infarction and psychiatric disorders who are uninsured have been identified as at risk for experiencing an increased ED LOS.[10–11]
While a subset of patients with uninsured status has been associated with an extended ED LOS,[10–11]there has been limited focus on how insurance status affects ED LOS for the general population who require hospital admission or emergency surgery. If an association exists betweeninsurance status and ED LOS, this may identify an intrinsic bias within the delivery of healthcare. Therefore, the primary goal of this study was to assess whether insurance status has a significant effect on ED LOS for those admitted to the hospital or transferred to an operating room. The secondary goal was to determine whether there was an association between insurance status and the likelihood of admission to the hospital or transfer to an operating room.
METHODS
Study design
This was a retrospective cross-sectional study of all patient encounters from January 2011 through October 2013 at an urban, academic Level I trauma center with an annual census of approximately 95 000 patient visits. The study site institutional review board approved this study with a waived consent.
Study setting and population
All patients who visited the study site ED during the study period were analyzed for inclusion. Patients with unspecified race and patients who were transferred to another facility, deceased, or left without completing care/ against medical advice were excluded. Unspecified race was excluded because prior studies had identifi ed it to be an important covariant in analyzing ED LOS.[6–9]The exclusion of transferred patients eliminated pediatric admissions from the final analysis, as the primary study site does not have inpatient pediatrics. There were no patients with unspecifi ed insurance status, as the medical record number for each patient was cross-matched to the institutional billing database to determine if insurance coverage was carried at the time of each visit. Details of insurance status, such as private, Medicaid or Medicare coverage, were not reliably available and therefore not obtained.
Study protocol
The ED electronic health record database was used to extract age, sex, race, triage acuity, disposition, and ED LOS for all encounters during the study period.
Measurements
Race was classifi ed as black, non-black or unspecifi ed. Triage acuity was based on the validated emergency severity index scoring system, in which severity of illness is categorized from 1 to 5, with 1 corresponding to the highest severity and 5 corresponding to the lowest.[12–16]Patient disposition was classifi ed as admitted to a general practice unit, admitted to an intensive care unit (ICU),transferred to the operating room, deceased, discharged,transferred to another facility or left without completing care/against medical advice. Admissions to the general practice unit and ICU were combined for analysis of the decision to admit and ED LOS. The interval for ED LOS represented the time from patient presentation at triage to physical departure from the ED.
Data analysis
All data are presented using standard descriptive statistics including means, standard deviations, minimums and maximums for continuous variables and using counts and percentages for categorical variables. Based on kurtosis and Q-Q plots, ED LOS was highly skewed, and a log transformation was found to most closely approximate a Gaussian distribution. ED LOS was compared between groups using independent-group t-tests for insurance status,race, acuity, and disposition using Pearson's correlation coefficient for age. ED LOS was compared between each group pair and a Benjamini-Hochberg adjustment was applied to the P value in order to control the type I error rate. A multivariable linear regression model was used to produce least-squared means and standard errors for insurance status,race, acuity and disposition while controlling for age. In order to model the odds of being admitted to the general practice unit/ICU or an operating room, a multinomial logistic regression model was used. Statistical significance was set at P<0.05. All analyses were performed using SAS 9.4. (SAS Institute Inc, Cary, NC, USA).
RESULTS
Characteristics of subjects
There were 257 504 patient encounters reviewed,of whom 48 001 were initially excluded for having unspecifi ed race. Of the remaining 209 503, an additional 7 968 were excluded based on the category of ED disposition (539 deceased, 3 562 transferred to another facility, and 3 867 left without completing service/against medical advice). After exclusion, 201 535 encounters were available for analysis (Figure 1). The mean age was 43.8years, 55.9% were female, 23.5% were uninsured, 8% were of non-black race, and admission rate was 24.5%. Baseline characteristics of all subjects are shown in Table 1.
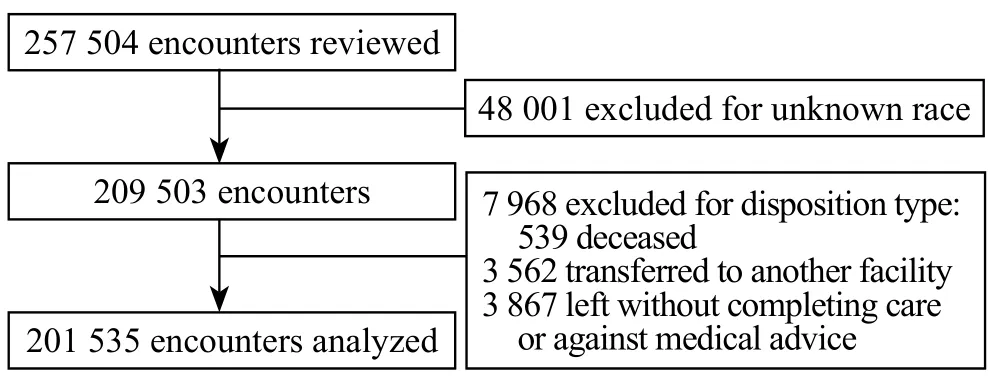
Figure 1. Flow chart of excluded patients.
Main results
After adjusting for age, sex, triage acuity and race,the presence of insurance coverage was associated with an increased average LOS of 575 (95%CI 552–598)versus 567 (95%CI 543–591) minutes for those being admitted (n=49 418, P<0.01). Conversely, the presence of insurance was associated with a decreased average LOS of 456 (95%CI 381–531) versus 499 (95%CI 423–575) minutes for those being transferred to the operating room (n=2 780, P<0.01). Results of multivariate modeling for ED LOS among patients admitted or transferred to the operating room are listed in Table 2. Lower severity Emergency Severity Index score, nonblack race and female gender were also associated with increased ED LOS among admitted patients. Females requiring hospital admission averaged 23 minutes longer ED LOS compared with males (P<0.01).
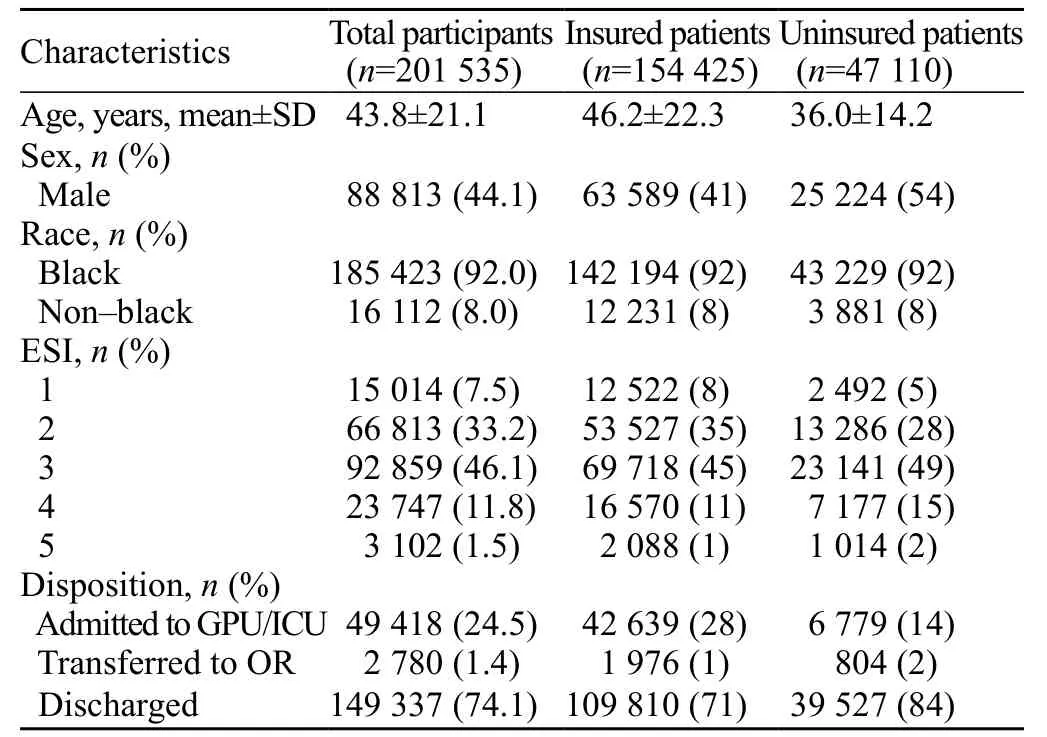
Table 1. Baseline characteristics of study population
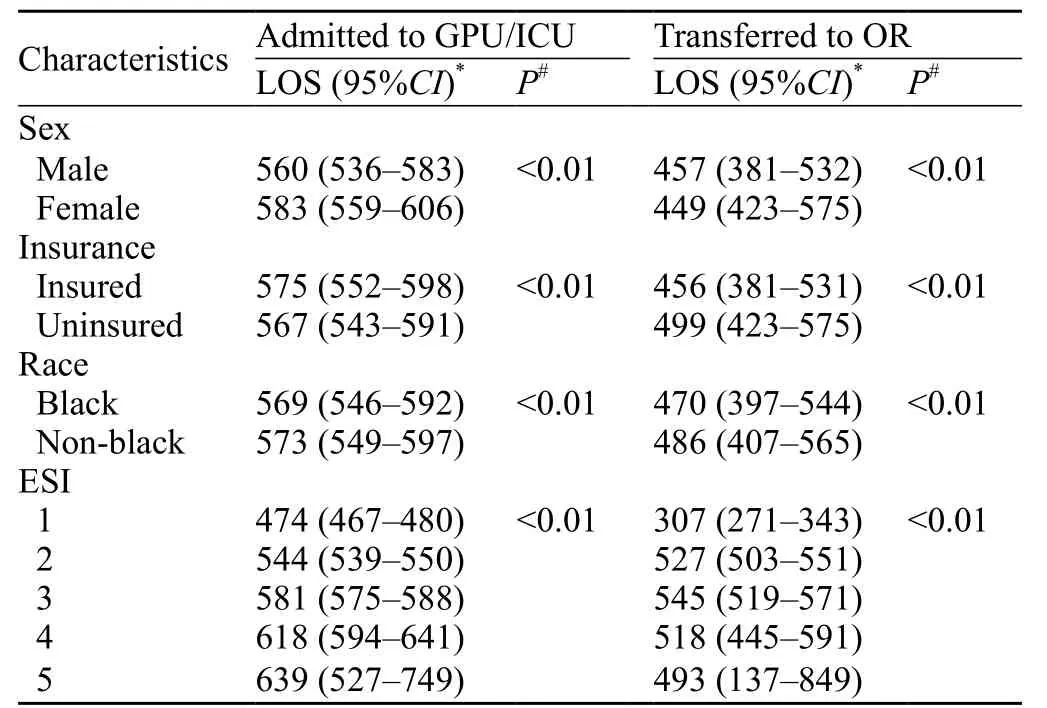
Table 2. Multivariate length of stay for those admitted to GPU/ICU or transferred to operating room
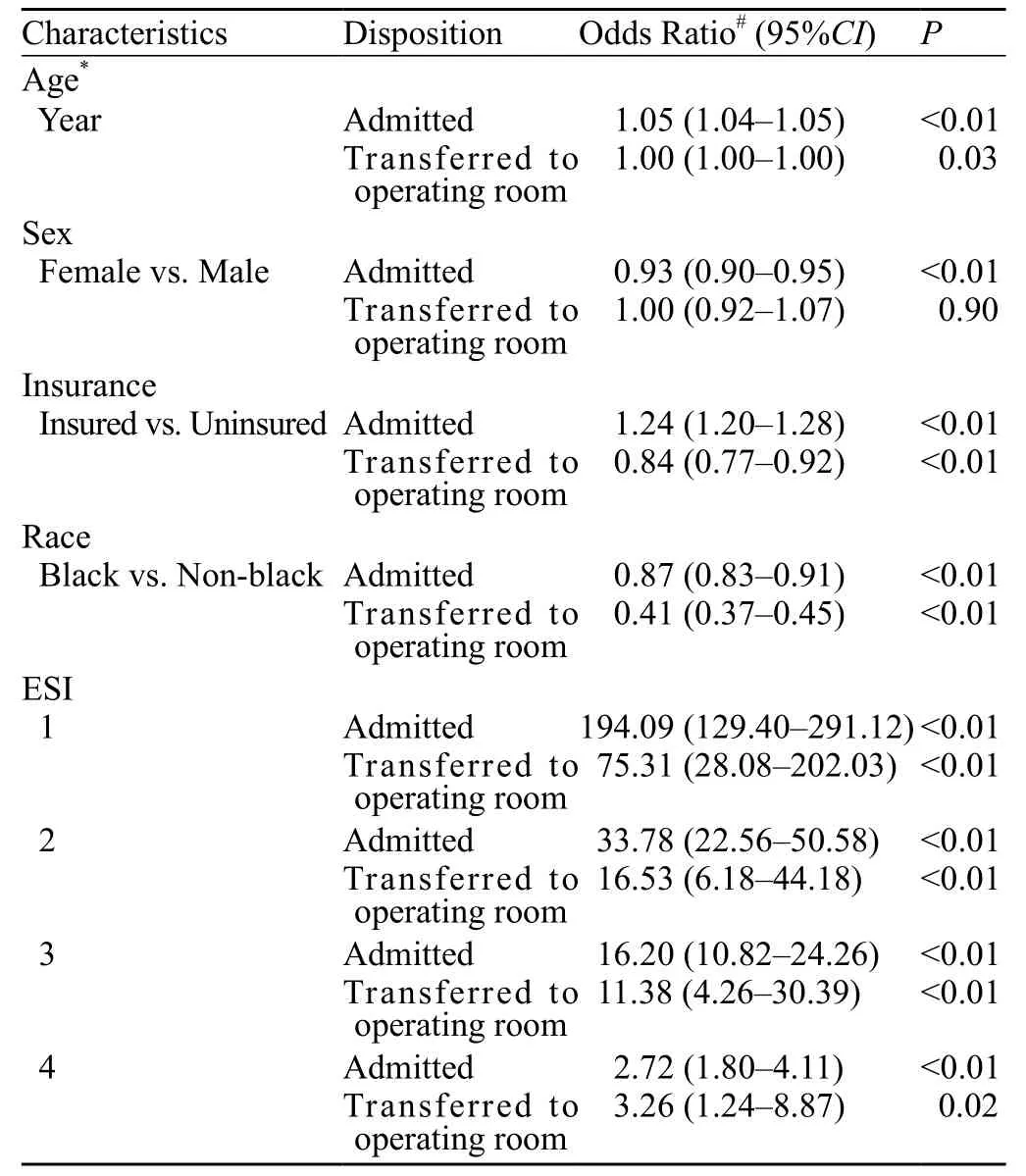
Table 3. Adjusted odds ratio for disposition type
Secondary outcome
Adjusting for the same predictors, insurance status was positively associated with admission to the general practice unit/ICU (adjusted odds ratio [OR] 1.24, 95%CI 1.20–1.28) and negatively associated with transfer to an operating room (adjusted OR 0.84, 95%CI 0.77–0.92). Additional results of multivariate modeling for admission are listed in Table 3. Black race was associated with a decreased likelihood of admission (OR 0.87, 95%CI 0.83–0.91) and transfer to an operating room (OR 0.41,95%CI 0.37–0.45).
DISCUSSION
The primary study aim was to assess the relationship between insurance status and ED LOS; the underlying hypothesis was that uninsured patients would experiencelonger ED LOS. After adjusting for other important covariates, there appears to be a likely clinically insignifi cant difference of only 8-minute in ED LOS for admitted adults based on insurance status. If anything,the uninsured at this urban teaching hospital had slightly lower ED LOS while waiting for admission. However,the same was not true with those being transferred to the operating room, with the uninsured experiencing a 43-minute longer ED LOS. Although such delay could be associated with increased risk for surgical complications,[17–20]this result should be interpreted with caution, as the analysis did not correct for potential confounders. The likely primary confounder was that the analysis did not adjust for operative patients who were transferred from outside hospitals to this tertiary care center. Such patients may have signifi cantly higher rates of insurance coverage and shorter waits for the operating room if the diagnosis had been made prior to the transfer between institutions.
Notably, this study did not find a likely clinically significant difference of only 4-minute in ED LOS between admitted black and non-black patients. This is in direct contrast to prior studies that have demonstrated inequality in ED LOS for black patients who were admitted.[6–9]This may in part be due to prior studies appreciating a between hospital difference in ED LOS for race. It was also observed that black patients experienced a 16-minute decreased ED LOS when awaiting transfer to the operating room, but the clinical significance of this additional wait in the non-black patient remains unclear. The observed differences in Emergency Severity Index level and ED LOS were expected, as patients with higher severities of illness likely require briefer testing and decision-making before a disposition is set to admit or operate. Finally, the average 23-minute increased ED LOS for admitted female patients is notable and deserves further analysis. Whether this refl ects greater complexity in the evaluation and decision-making process of admitting female patients, differences in comorbidities in the population, or potential gender bias is unknown.
These gender disparities for those admitted and insurance and racial disparities for those transferred to the operating room are critically important, as ED LOS has been associated with worse outcomes in the shortand long-term.[21–23]For example, patients who wait longer for an ICU bed have increased 10-day mortality.[21]With blunt trauma patients who require intubation, ED LOS is an independent risk factor for the development of pneumonia.[22]Patients with non-ST-segment-elevation myocardial infarction who had increased ED LOS are at risk for being less adherent to recommended medical therapies and suffering increased rates of recurrent myocardial infarction.[8]Increased ED LOS is also associated with decreased patient satisfaction.[24]These and other factors have led the Centers for Medicare and Medicaid Services to now include ED LOS as a clinical quality measure.[3]
The secondary aim of this study was to assess the relationship between insurance status and admission likelihood. To date, published data on this subject has been mixed.[25–28]A study by Svenson et al[25]demonstrated that insurance status was an independent predictor for admission among those with head injuries. In a similar study by White et al,[26]the opposite was observed with no difference in admission for both the general population or in a subset of severely injured trauma patients. A third study, by Ruger et al,[27]observed that the insured had an increased likelihood of admissions to the general hospital, but not the ICU or operating room.
Interestingly, in this study there were increased odds of hospital admission and decreased odds of transfer to the operating room among insured patients. This should also be interpreted with caution as the analysis did not allow for adjustment of patient transfers into the primary study site, which may have a higher likelihood for admission and higher insured rate, thereby potentially falsely elevating the OR for admission. Furthermore,the analysis did not adjust for comorbid conditions that may affect the likelihood for admission. It is possible that uninsured patients had less comorbid conditions but presented more frequently for non-emergent medical problems. Regardless, this finding that the insured are less likely to have emergent surgery does deserve further study, especially since they vary signifi cantly from those of Ruger et al,[27]in which there was no appreciable difference in likelihood of transfer to the operating room. This could reflect the uninsured presenting with greater need for emergent surgery due to poor access to health care. It could also reflect a higher proportion of uninsured among trauma patients who require emergency surgery.
Finally, the results of black race being associated with decreased odds of admission and emergency surgery should also be interpreted with caution for the same reasons as the insured status on admission and transfer to the operating room likelihood. While the results deserve a further study, a key potential confounder is that transfers into the tertiary care site of the study bias the likelihood of admission toward the non-black patient.This is because the majority of patients transferred to the tertiary care study site for evaluation is far more likely to require higher levels of care and are from a non-urban setting with a smaller black patient demographic.
Limitations
There were multiple limitations with this study. Firstly, it was performed within a single urban institution with a population predominantly of black race, which may not be generalized to other institutions or regions with different racial demographics. Secondly, the crosssectional nature of this study and use of the electronic health record database produced significant limitation as the data collection was limited to only information available from established administrative data stores. Most notably, this prevented the collection of data on chief complaint and patient comorbid conditions that may have significantly impacted the multivariable models. Finally, there were a significant proportion of patients that had unspecified race and were therefore excluded,which could ultimately produce a skewed result.
In conclusion, insurance status was not associated with a clinically significant difference in ED LOS for admitted patients. Uninsured patients averaged a 43-minute longer ED LOS awaiting emergent surgery. Future studies should work to identify specific factors that affect ED LOS between the insured and uninsured cohort. Although the insured were more likely to be admitted and less likely to be transferred to the operating room, these findings are subject to confounding factors and deserve a further study.
Funding: None.
Ethical approval: The study site institutional review board approved this study with a waived consent.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors: Wilson S proposed the study and wrote the first draft. All authors read and approved the fi nal version of the paper.
REFERENCES
1 Gonzalez Morganti K, Bauhoff S, Blanchard JC, Abir M, Iyer N,Smith A, et al. The evolving role of emergency departments in the United States. Santa Monica, CA: RAND Corporation; 2013.
2 Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997–2007. JAMA 2010; 304: 664–770.
3 Centers for Medicare and Medicaid Services. 2014 clinical quality measures Available at: http://www.cms.gov/Regulationsand-Guidance/Legislation/EHRIncentivePrograms/2014_ ClinicalQualityMeasures.html. Accessed December 3, 2014.
4 Asplin BR. Measuring crowding: time for a paradigm shift. Acad Emerg Med 2006; 13: 459–461.
5 Herring A, Wilper A, Himmelstein DU, Woolhandler S, Espinola JA, Brown DF, et al. Increasing length of stay among adult visits to U.S. Emergency departments, 2001–2005. Acad Emerg Med 2009; 16: 609–616.
6 Pines JM, Russell Localio A, Hollander JE. Racial disparities in emergency department length of stay for admitted patients in the United States. Acad Emerg Med 2009; 16: 403–410.
7 Karaca Z, Wong HS. Racial disparity in duration of patient visits to the emergency department: teaching versus non-teaching hospitals. West J Emerg Med 2013; 14: 529–541.
8 Diercks DB, Roe MT, Chen AY, Peacock WF, Kirk JD, Pollack CV Jr, et al. Prolonged emergency department stays of non-ST-segment-elevation myocardial infarction patients are associated with worse adherence to the American College of Cardiology/ American Heart Association guidelines for management and increased adverse events. Ann Emerg Med 2007; 50: 489–496.
9 Stephens RJ, White SE, Cudnik M, Patterson ES. Factors associated with longer length of stay for mental health emergency department patients. J Emerg Med 2014; 47: 412–419.
10 Bekmezian A, Chung PJ, Cabana MD, Maselli JH, Hilton JF, Hersh AL. Factors associated with prolonged emergency department length of stay for admitted children. Pediatr Emerg Care 2011; 27: 110–115.
11 Gardner RL, Sarkar U, Maselli JH, Gonzales R. Factors associated with longer ED lengths of stay. Am J Emerg Med 2007; 25: 643–650.
12 Storm-Versloot MN, Ubbink DT, Chin a Choi V, Luitse JS. Observer agreement of the Manchester Triage System and the Emergency Severity Index: a simulation study. Emerg Med J 2009; 26: 556–560.
13 Storm-Versloot MN, Ubbink DT, Kappelhof J, Luitse JS. Comparison of an informally structured triage system, the emergency severity index, and the manchester triage system to distinguish patient priority in the emergency department. Acad Emerg Med 2011; 18: 822–829.
14 Durani Y, Brecher D, Walmsley D, Attia MW, Loiselle JM. The Emergency Severity Index version 4: reliability in pediatric patients. Pediatr Emerg Care 2009; 25: 751–753.
15 Elshove-Bolk J, Mencl F, van Rijswijck BT, Simons MP, van Vugt AB. Validation of the Emergency Severity Index (ESI)in self-referred patients in a European emergency department. Emerg Med J 2007; 24: 170–174.
16 Baumann MR, Strout TD. Triage of geriatric patients in the emergency department: validity and survival with the Emergency Severity Index. Ann Emerg Med 2007; 49: 234–240.
17 Duchesne JC, Barbeau JM, Islam TM, Wahl G, Greiffenstein P,McSwain NE, Jr. Damage control resuscitation: from emergency department to the operating room. Am Surg 2011; 77: 201–206.
18 Clarke JR, Trooskin SZ, Doshi PJ, Greenwald L, Mode CJ. Time to laparotomy for intra-abdominal bleeding from trauma does affect survival for delays up to 90 minutes. J Trauma 2002; 52: 420–425.
19 Abou-Nukta F, Bakhos C, Arroyo K, Koo Y, Martin J, Reinhold R, et al. Effects of delaying appendectomy for acute appendicitis for 12 to 24 hours. Arch Surg 2006; 141: 504–506.
20 Earley AS, Pryor JP, Kim PK, Hedrick JH, Kurichi JE, Minogue AC, et al. An acute care surgery model improves outcomes in patients with appendicitis. Ann Surg 2006; 244: 498–504.
21 Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust 2006; 184: 213–216.
22 Carr BG, Kaye AJ, Wiebe DJ, Gracias VH, Schwab CW, Reilly PM. Emergency department length of stay: a major risk factor for pneumonia in intubated blunt trauma patients. J Trauma 2007; 63: 9–12.
23 Ackroyd-Stolarz S, Guernsey J, MacKinnon N, Kovacs G. Is a prolonged stay in the emergency department associated with adverse events in older patients? Acad Emerg Med 2008; 15: S67.
24 Taylor C, Benger JR. Patient satisfaction in emergency medicine. Emerg Med J 2004; 21: 528–532.
25 Svenson JE, Spurlock CW. Insurance status and admission to hospital for head injuries: are we part of a two-tiered medical system? Am J Emerg Med 2001; 19: 19–24.
26 White FA, French D, Zwemer FL Jr, Fairbanks RJ. Care without coverage: is there a relationship between insurance and ED care? J Emerg Med 2007; 32: 159–165.
27 Ruger JP, Richter CJ, Lewis LM. Association between insurance status and admission rate for patients evaluated in the emergency department. Acad Emerg Med 2003; 10: 1285–1288.
28 Sox CM, Burstin HR, Edwards RA, O'Neil AC, Brennan TA. Hospital admissions through the emergency department: does insurance status matter? Am J Med 1998; 105: 506–512.
Received November 15, 2015
Accepted after revision March 26, 2016
DOI:10.5847/wjem.j.1920–8642.2016.02.005
 World journal of emergency medicine2016年2期
World journal of emergency medicine2016年2期
- World journal of emergency medicine的其它文章
- German critical incident reporting system database of prehospital emergency medicine: Analysis of reported communication and medication errors between 2005–2015
- Risk assessment of the emergency processes: Healthcare failure mode and effect analysis
- Pre-hospital assessment with ultrasound in emergencies: implementation in the fi eld
- Characterization of available automated external defi brillators in the market based on the product manuals in 2014
- Maternal and fetal outcomes in term premature rupture of membrane
- An incidental case of Wellens' syndrome in a community emergency department
