马来西亚综合医院后囊破裂的诱发因素与相关性及结果分析
Thanigasalam Thevi, Maizura M Zin
(作者单位:马来西亚,马六甲 75400,马六甲医院,眼科)
马来西亚综合医院后囊破裂的诱发因素与相关性及结果分析
Thanigasalam Thevi, Maizura M Zin
(作者单位:马来西亚,马六甲 75400,马六甲医院,眼科)
摘要
关键词:后囊破裂原因;后囊破裂原因的相关性及结果;视力结果
Abstract
•AIM: To see the causative factors, associations and outcomes of posterior capsule rupture (PCR).
•METHODS: A retrospective cohort study was done of all patients with PCR from 2007 to 2014 in Melaka Hospital. Associations between ocular comorbidities, lens related complications, surgeon grade, type of cataract surgery, whether done alone or in combination, with the occurrences of PCR were studied. The final visual outcome of cases with PCR was studied.
•RESULTS: PCR was the commonest intraoperative complication (n=623, 4.8%) among 12 846 patients. Ocular comorbidities and status of the lens did not cause PCR. Experience and seniority of surgeons were significantly associated with PCR. Medical officers had more PCRs than gazetting specialists (P=0.0000), who inturn had more PCRs than specialists (P=0.000). Each type of cataract surgery done was also significantly associated with PCR-phacoemulsification (phaco), phaco convert to extracapsular cataract extraction (ECCE) and intracapsular cataract extraction (ICCE) (P=0.000), lens aspiration (P=0.020), and ECCE (P=0.003). Specialists got good outcomes compared to trainees without PCR occurring (P=0.001) and also with PCR occurring (P=0.013). However, no difference was observed in the occurrence of PCR in complicated cases between specialists and trainees. Vision was compromised mainly by astigmatism following PCR. Impaired vision (P=0.000) and poor vision (P=0.000) were more than good vision. Poor vision was more in PCR compared to other complications.(P=0.000).
•CONCLUSION: PCR occurs in all types of cataract surgeries and is the main intraoperative complication causing poor vision. Good outcomes were significantly more when specialists got PCR compared to trainees. Junior surgeons should practice in wet labs and be given more cases.
KEYWORDS:•posterior capsule rupture-causes; associations and outcomes posterior capsule rupture-causes; visual outcomes
Citation:Thevi T, Maizura MZ. Posterior capsule rupture-causes, associations and outcomes: eight year analysis in a Malaysian General Hospital.GuojiYankeZazhi(IntEyeSci) 2016;16(4):600-606
INTRODUCTION
Cataract is the commonest cause of reversible blindness and cataract surgery is the commonest intraocular surgery performed. The National Eye Survey conducted in 1998 found that cataract was the leading cause of blindness (39%)[1]. The aim of doing cataract surgery is to restore vision. As in every surgery done, including cataract surgeries, complications are unavoidable and posterior capsule ruptures (PCR) are the commonest intraoperative complications.
The objective of this study was to study the risk factors that caused and were associated with the occurrence of PCR and the outcome of patients who had PCR during cataract surgery in a Malaysian General Hospital setting. The study was done in Melaka General Hospital, a government hospital serving the population of Melaka state. Melaka has a population of 474000 as of 2014[2]. The ophthalmology clinic and ward facilities treat general ophthalmology cases and there is an in-house vitro-retinal surgeon for vitro-retinal services. There are a few private hospitals with ophthalmology services but due to the free cost for civil servants and cheaper cost for others, more people seek treatment in the government hospital. Cataract surgeries are done by specialists, gazetting specialists and medical officers. A specialist is one who has passed the postgraduate ophthalmology exam and has been assessed to work independently. A gazetting specialist is one who has passed the postgraduate exam but is under supervision of a senior specialist. A medical officer has a degree in medicine and is permitted to do cataract surgery under supervision of a senior specialist. Cataract surgeries are done on 4 out of the 5 working days.
In this study, several factors were studied to see if they were associated with the occurrence of PCR. It was done to see if ocular comorbidities, lens related complications, grade of surgeon operating and type of cataract surgery done and whether cataract surgery done in combination with other surgeries were associated with PCR. Finally, whether the occurrence of PCR affected obtaining good vision was studied. The reasons for not obtaining good visual acuity were noted.
SUBJECTS AND METHODS
A retrospective cohort study was conducted in Melaka Hospital to study the outcome of patients who had PCR as a complication during cataract surgery. The study was done in Melaka General Hospital, a Government Hospital serving the population of Melaka state. Melaka has a population of 474000 as of 2014[2]. The ophthalmology clinic and ward facilities treat general ophthalmology cases and there is an in-house vitreo-retinal surgeon for vitreo-retinal services. There are a few private hospitals with ophthalmology services but due to the free cost for civil servants and cheaper cost for others, more people seek treatment in the government hospital. Cataract surgeries are done by specialists, gazetting specialists and medical officers. A specialist is one who has passed the postgraduate ophthalmology exam and has been assessed to work independently. A gazetting specialist is one who has passed the postgraduate exam but is under supervision of a senior specialist. A medical officer has a degree in medicine and is permitted to do cataract surgery under supervision of a senior specialist. Cataract surgeries are done on 4 out of the 5 working days.
Table 1Types of intraoperative complications

IntraoperativecomplicationsNumberofeyesPercentagePosteriorcapsulerupture6234.8%Vitreousloss4113.2%Zonulardehiscence1461.1%Dropnucleus170.1%Suprachoroidalhemorrhage50.0%Centralcornealoedema20.0%
Data was obtained from the National Eye Database (NED). Permission to conduct the study was granted by the Malaysian Research Ethics Committee (MREC). The study was registered with the National Malaysian Research Registry (NMRR) and National Institute of Health (NIH). The study covered a period of 8y from 2007 to 2014. Informed consent does not apply here as there was no contact with patients. This was a secondary data analysis. Data was already released by the director and coordinator of National Eye Database for cataract surgery. (these individuals have been acknowledged).
All ocular comorbidities such as pterygium involving the cornea, corneal opacities, glaucoma, chronic uveitis and pseudoexfoliation were noted. Lens related complications such as phacomorphic, phacolytic and subluxated lenses were recorded. The associations between ocular comorbidities and lens related complications were studied. The status of the surgeon whether a specialist, gazetting specialist or medical officer were noted to see if the grade of the surgeon was associated with the occurrence of PCR. The various types of cataract surgeries done and the associations with PCR were studied. The types of surgeries done were phacoemulsification (phaco), extracapsular cataract extraction (ECCE), intracapsular cataract extraction (ICCE), lens aspiration and phaco convert to ECCE. Phaco convert to ECCE are cases where at some stage of phaco, a problem was detected and the case was converted to ECCE. An example of this would be-the suspicion of a PCR during sculpting or a lens which appeared unstable during the capsulorhexis. Sometimes when a nucleus is found to be too dense during sculpting, the phaco is abandoned and ECCE is done instead, this is also listed as phaco convert to ECCE.
Presence of vitreous loss following PCR is managed by anterior vitrectomy in the same sitting. Posterior chamber intraocular lenses (PCIOL) are placed if there is adequate posterior capsule to support it. Otherwise anterior chamber intraocular lenses (ACIOL) are placed. In cases where ACIOLs are contraindicated-such as those who have glaucoma where the conjunctiva needs to be preserved, then scleral fixated intraocular lenses (IOLs) are placed.
Table 2Association of posterior capsule rupture with ocular comorbidities
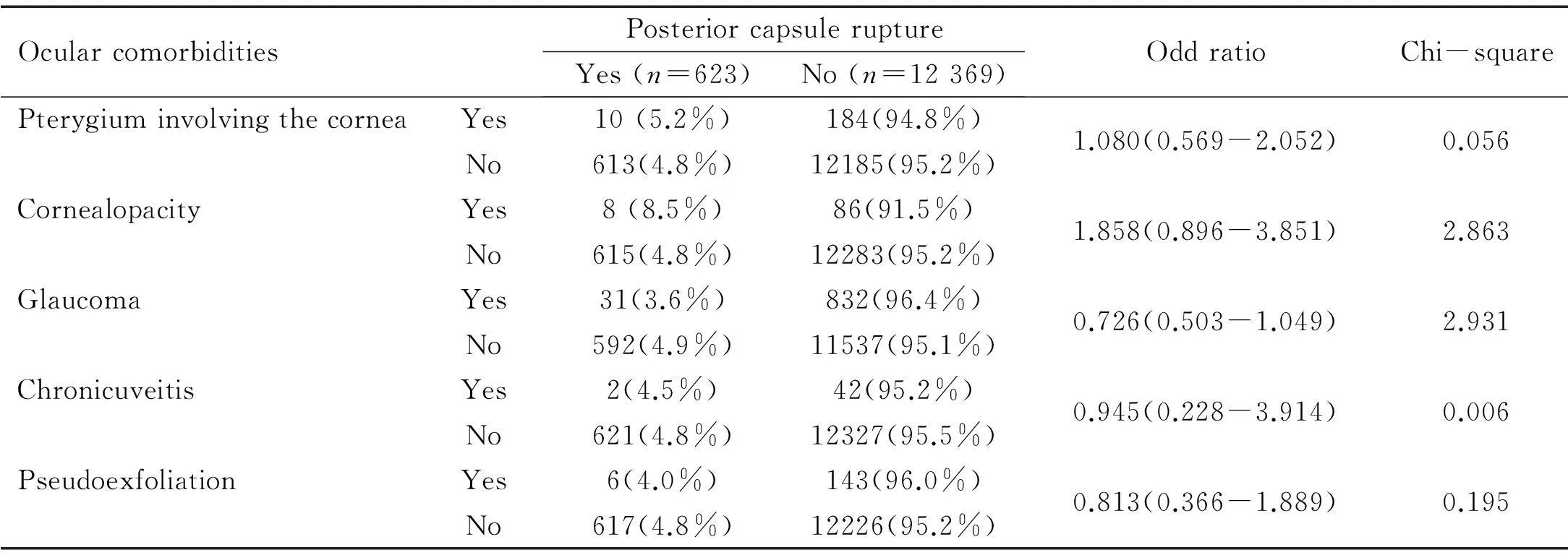
OcularcomorbiditiesPosteriorcapsuleruptureYes(n=623)No(n=12369)OddratioChi-squarePPterygiuminvolvingthecorneaYes10(5.2%)184(94.8%)1.080(0.569-2.052)0.0560.813No613(4.8%)12185(95.2%)CornealopacityYes8(8.5%)86(91.5%)1.858(0.896-3.851)2.8630.091No615(4.8%)12283(95.2%)GlaucomaYes31(3.6%)832(96.4%)0.726(0.503-1.049)2.9310.087No592(4.9%)11537(95.1%)ChronicuveitisYes2(4.5%)42(95.2%)0.945(0.228-3.914)0.0060.646No621(4.8%)12327(95.5%)PseudoexfoliationYes6(4.0%)143(96.0%)0.813(0.366-1.889)0.1950.659No617(4.8%)12226(95.2%)
Chi-square,P< 0.05 considered significant.
Table 3Output of logistic regression model summary

VariableBSEWalddfPExp(B)95%CIforEXP(B)LowerUpperSubluxated/Dislocated-0.0340.7290.00210.9630.9660.2314.037Phacolytic1.6960.6536.75110.0095.4501.51719.587Phacomorphic0.8380.6131.86810.1722.3110.6957.684Constant-2.9950.0415256.71810.0000.050
Finally, the outcome of patients with PCR was studied. The outcome was taken as the best corrected visual acuity based on refraction done by hospital based optometrists. Best corrected vision was recorded at 12wk postoperatively which was the period of follow-up following the cataract surgeries with PCRs. The best corrected outcome was divided into good vision (6/6-6/12) (logMAR 0.00-0.30), impaired vision (6/18-6/36) and poor vision (6/60 and worse) (logMAR 1.00 and worse). Whether patients were able to obtain good visual acuity in the event of a PCR during cataract surgery was studied. The reasons why the patient did not obtain good visual acuity following a PCR were studied.
Statistical AnalysisThe data was analyzed with Statistical Package for Social Sciences (SPSS) program version 20 (USA). The global Chi-square and Fisher’s exact test were used to determine the possible relation between two categorical variables. The logistic regression test was performed to determine the strongest factors between the categorical data.P<0.05 was considered significant.
RESULTS
A total of 12 846 patients underwent cataract surgery during the study period but only 797 (6.20%) patients had intraoperative complications during surgery. PCR was the commonest intraoperative complication among the 6 types of complications seen in our study (Table 1).
All 623 (4.8%) patients who had PCR during surgery were included in this study. Some data was missing and hence; those were omitted in various sections of analysis. Glaucoma was the commonest ocular comorbidity cases causing PCR during surgery with 31 (3.6%) cases and the least was chronic uveitis with 2 (4.5%) cases. Table 2 shows that there was no association between PCR and all the ocular comorbidities factors included in this study. Presence of ocular comorbidities did not affect significantly the occurrence of PCR complication during surgery.
Table 3 shows the binary logistic regression analysis for PCR among patient with lens related complications. All 12 846 patients were included in the analysis. Phacolytic lenses caused PCR during surgery withP=0.009 while other lens status like phacomorphic, phacolytic and subluxated lenses did not cause PCR. Phacolytic lens was 5.450 times more likely to cause PCR compared to other lens status.
The associations between PCR and the grade of surgeon operating were analyzed.medical officers got more PCRs (149, 9.9%) compared to specialists (415, 3.9%). Gazetting specialists also got more PCRs (58, 7.6%) compared to specialists (415, 3.9%). Medical officers got significantly more PCRs compared to specialists (P<0.001). Similarly, gazetting specialists also got significantly more PCRs compared to specialists (P<0.001) as shown in Table 4. The less the experience, the more the PCRs.
Table 5 shows that phaco converted to PCR has the highest rate of PCR with 38.4% cases, followed by ICCE (20.5%), lens aspiration (8.7%), ECCE (6.1%), and phaco (3.8%). There was a significant association between ECCE, ICCE, lens aspiration, phaco and phaco converted to ECCE with the occurrence of PCR sinceP<0.05. PCIOLs were placed in 439 (81.1%) of cases that had adequate support. ACIOLs were placed in 95 cases (17.6%).
with inadequate posterior capsule support. Only 7 cases had scleral fixated IOLs (Table 6). In 65 cases the IOLs were planned but were implanted at a later date. Only in 7 cases,Table 4Comparison between surgeon status and posterior capsule rapture

SurgeonstatusPosteriorcapsuleraptureYesNoOddratioChi-squarePn=564n=11654Medicalofficer149(9.9%)1349(90.1%)0.365(0.300-0.443)110.177<0.001Specialist415(3.9%)10305(96.1%)n=473n=11006Gazettingspecialist58(7.6%)701(92.4%)0.487(0.336-0.647)25.504<0.001Specialist415(3.9%)10305(96.1%)
P<0.05 considered significant.
Table 5Comparison between surgery type and posterior capsule rupture

SurgerytypePosteriorcapsuleruptureYes(n=623)No(n=12369)OddratioChi-squarePECCEYes122(6.1%)1878(93.9%)1.360(1.109-1.668)8.8150.003No501(4.6%)10491(95.4%)ICCEYes16(20.5%)62(79.5%)5.232(3.002-9.120)42.463<0.001No607(4.7%)12307(95.3%)LensaspirationYes14(8.7%)147(91.3%)1.911(1.098-3.327)5.4320.020No609(4.7%)12222(95.3%)PhacoconvertedtoPCRYes71(38.4%)114(61.6%)13.827(10.158-18.821)463.63<0.001No552(4.3%)12255(95.7%)PhacoYes395(3.8%)10102(96.2%)0.389(0.328-0.460)127.583<0.001No228(9.1%)2267(90.9%)
Chi-square,P<0.05 considered significant.
Table 6Type of IOL for posterior capsule rupture

TypeofIOLFrequency(n)Percentage(%)AnteriorchamberIOL9517.6PosteriorchamberIOL43981.1ScleralfixatedPCIOL71.3Total541100.0
PCIOL: Posterior chamber intraocular lenses.
the patients had been planned for IOL but they were not implanted due to various reasons including the fact that the prognosis was poor.
Following PCR, 341(3.7%) patients had good vision while 109(8.3%) had impaired vision. From Table 7, it is seen that a greater percentage, (49, 10.2%) of patients had poor vision after having PCR during surgery. There was a significant difference (P<0.001) between good vision and impaired vision among patients with PCR. It means patients were more likely to get impaired vision rather than good vision after the occurrence of PCR during surgery. More patients also got poor vision compare to good vision following PCR (P<0.001).
Table 8, shows that 49 (9.8%) patients had poor vision after having PCR during surgery while 430 (4.1%) patients had poor vision following other types of intraoperative complications. Since (P<0.001) it can be concluded that PCR during surgery results in poor vision compared to the other intraoperative complications.
Specialists got good visual outcomes (84.3%) compared to trainees (81.2%) and this was significant (P=0.001). Poor vision was also significantly more among specialists (4.4%) compared to trainees (4.3%)(Table 9).
Following PCR, good visual outcome was significantly more among specialists (70.7%) than trainees (63.2%) (P=0.013). Poor vision was also significantly more among specialists (11%) compared to trainees (7.4%). (Table 10).There was no association of PCR during complicated cataract surgery between specialists and trainees. (Table 11).Following PCR, 33 (5.3%) patients did not obtain good visual acuity due to preexisting ocular comorbidity, followed by high astigmatism 25 (4%) and cystoid macular edema (CME) with 7 (1.1%) patients as seen in Table 12. Lesser causes of not obtaining good visual acuity were, posterior capsular opacity (PCO) 5 (0.8%), cornea decompensation 3 (0.5%), retinal detachment (RD) 2 (0.3%), infective endophthalmitis 1 (0.2%) and IOL decentration/ dislocation 1(0.2%) patient.
DISCUSSION
PCR was the commonest intraocular complication (n=63, 4.8%) which occurred during cataract surgery among the 797 patients who had intraoperative complications out of 12 846 patients who underwent cataract surgery. The presence of ocular comorbidities such as pterygium involving the cornea, corneal opacities, glaucoma, chronic uveitis or pseudoexfoliation did not affect the occurrence of intraoperative complications. Glaucoma was the commonest ocular comorbidity associated with PCR (n=31, 3.6%). ATable 7Comparison of visual outcome in posterior capsule rupture

BestcorrectedvisionPosteriorcapsuleruptureYesNoOddratioChi-squarePn=450n=10065Goodvision341(3.7%)8868(96.3%)2.368(1.893-2.963)60.197<0.001Impairedvision109(8.3%)1197(91.7%)n=390n=9298Goodvision341(3.7%)8868(96.3%)2.963(2.163-4.059)50.202<0.001Poorvision49(10.2%)430(89.8%)
Chi-square,P<0.05 considered significant.
Table 8Comparison between posterior capsule rupture with other intraoperative complications for poor vision

ComplicationsPoorvisionYes(n=479)No(n=10515)OddratioChi-squarePPCR49(9.8%)450(90.2%)2.549(1.869-3.476)37.433<0.001Othercomplications430(4.1%)10065(95.9%)
Chi-square,P<0.05 considered significant.
Table 9Comparison of cataract surgery outcomes between trainees and specialists
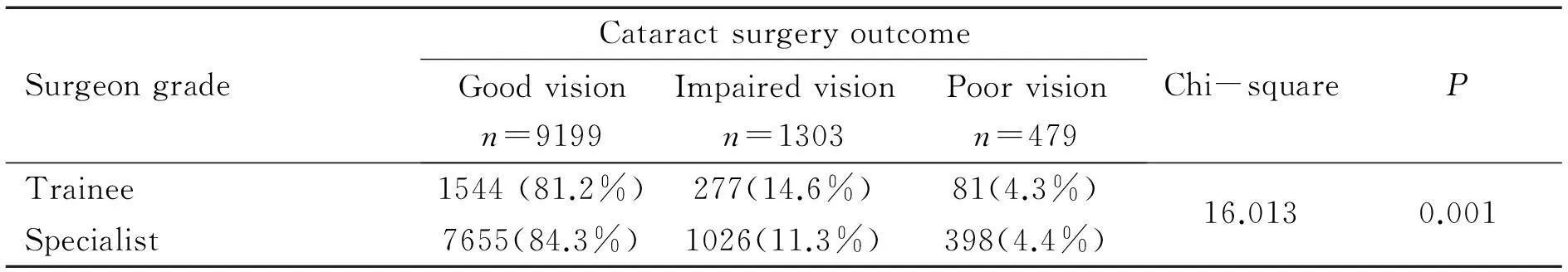
SurgeongradeCataractsurgeryoutcomeGoodvisionn=9199Impairedvisionn=1303Poorvisionn=479Chi-squarePTrainee1544(81.2%)277(14.6%)81(4.3%)16.0130.001Specialist7655(84.3%)1026(11.3%)398(4.4%)
Chi-square,P<0.05 considered significant.
Table 10Comparison of outcomes after posterior capsule rupture between trainees and specialists
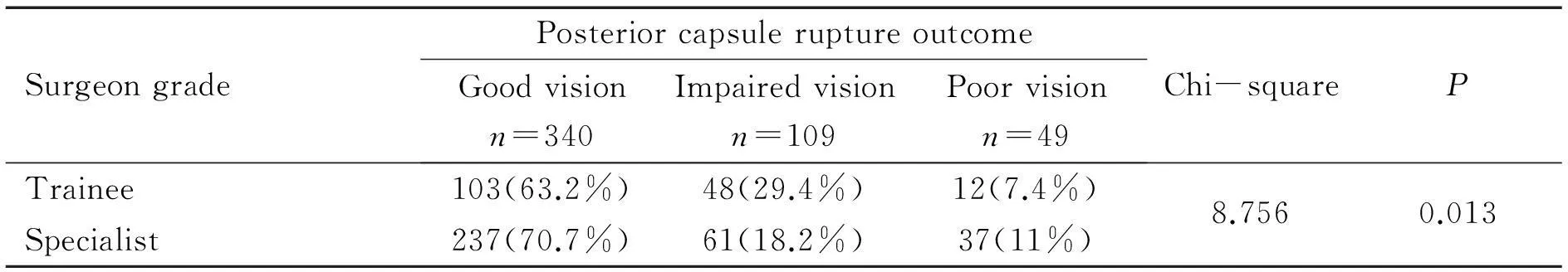
SurgeongradePosteriorcapsuleruptureoutcomeGoodvisionn=340Impairedvisionn=109Poorvisionn=49Chi-squarePTrainee103(63.2%)48(29.4%)12(7.4%)8.7560.013Specialist237(70.7%)61(18.2%)37(11%)
Chi-square,P<0.05 considered significant.
Table 11Association between complicated surgery and surgeon status for posterior capsule rupture
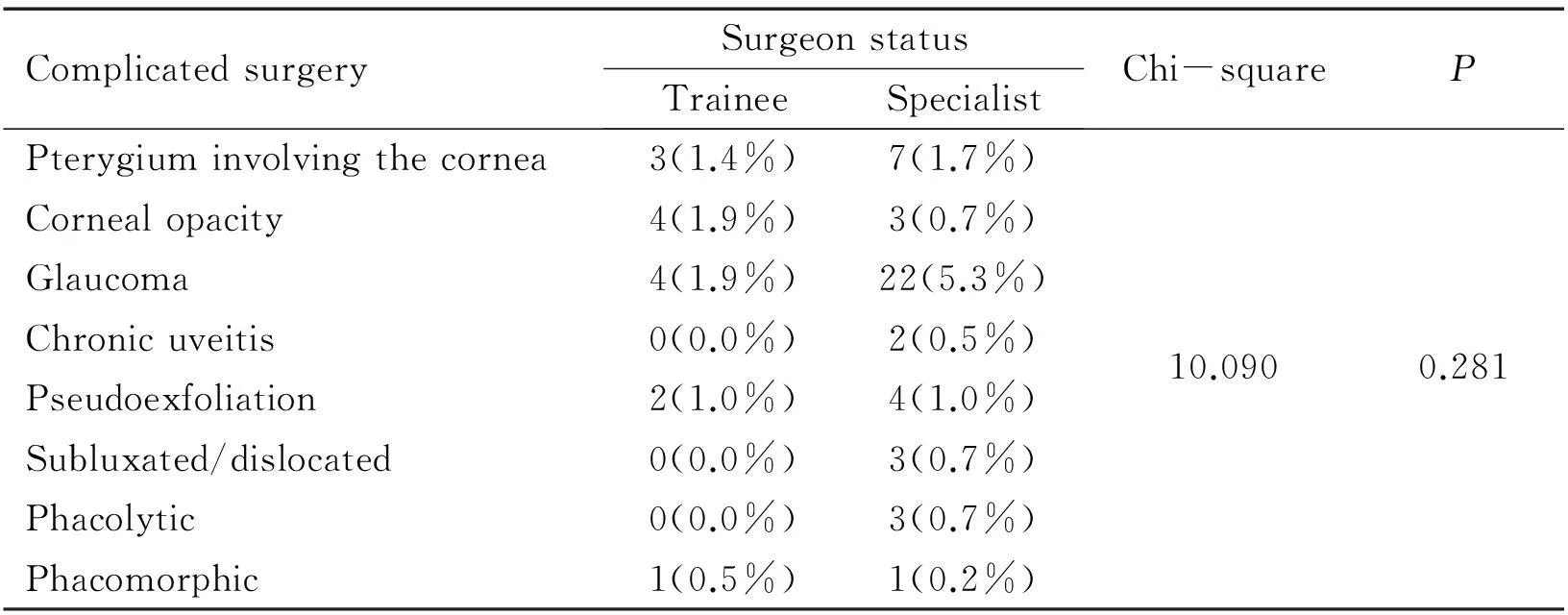
ComplicatedsurgerySurgeonstatusTraineeSpecialistChi-squarePPterygiuminvolvingthecornea3(1.4%)7(1.7%)Cornealopacity4(1.9%)3(0.7%)Glaucoma4(1.9%)22(5.3%)Chronicuveitis0(0.0%)2(0.5%)10.0900.281Pseudoexfoliation2(1.0%)4(1.0%)Subluxated/dislocated0(0.0%)3(0.7%)Phacolytic0(0.0%)3(0.7%)Phacomorphic1(0.5%)1(0.2%)
Chi-square,P<0.05 considered significant.
multicenter audit from the Cataract National Dataset also found that patients with glaucoma had a higher risk for PCR during cataract surgery[3]. Although pseudoexfoliation has often been thought to be associated with PCR, in this study and another study done by Thanigasalametal[4]pseudoexfoliation has not been found to cause PCR. Tulrabaetal[5]found that glaucoma patients had a higher incidence of PCR with vitreous loss (P=0.03).
Lens related complications such as phacomorphic, phacolytic and subluxated lenses were not significantly associated with PCR although phacolytic lenses were 5.450 times more likely to get a PCR. We did not find any literature correlating the lens status with PCR.
Table 12Reasons for not obtaining good visual acuity
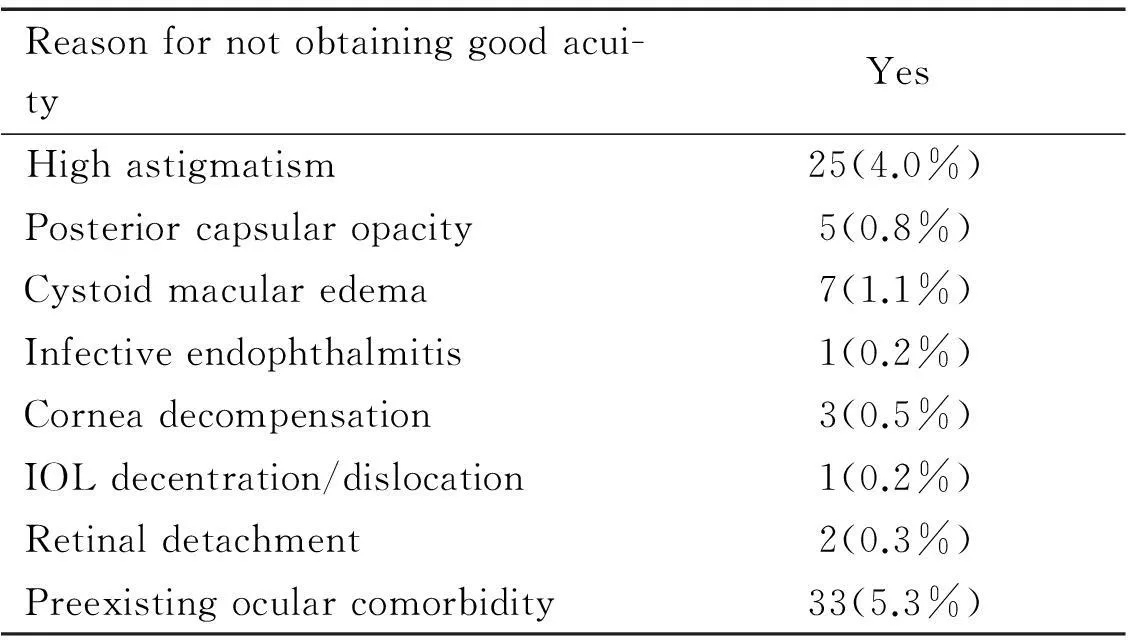
Reasonfornotobtaininggoodacui-tyYesHighastigmatism25(4.0%)Posteriorcapsularopacity5(0.8%)Cystoidmacularedema7(1.1%)Infectiveendophthalmitis1(0.2%)Corneadecompensation3(0.5%)IOLdecentration/dislocation1(0.2%)Retinaldetachment2(0.3%)Preexistingocularcomorbidity33(5.3%)
The less the experience of the surgeon, the more likely they got PCR and this was a significant finding. Medical officers were more likely to get complications compared to gazetting specialists (P=0.000) who in turn were more likely to get complications compared to specialists (P=0.000). The multicenter audit of the Cataract National Dataset also found that PCR was higher among less experienced surgeons[6]. Chenetal[7]did an audit in a Hawaiian Hospital and found that surgeon volume (number of cases) was inversely related to PCR. In a 5-year analysis of 48 377 phaco cases, Tietal[8]found that faculty PCR rates were less than resident PCR rates (P<0.01). In this study, the details of when the PCR occurred were not available. Knowing the point of occurrence and why it occurred may facilitate preventing this complication. Thanigasalametal[9]found that PCR occurred more during segment removal in the hands of specialists, but more during cortical removal in the hands of consultants.
Each type of surgical technique was associated with a significant amount of PCR when compared with the other types of cataract surgeries. The risk of getting a PCR with phaco, phaco converted to ECCE, or ICCE each, compared to other types of cataract surgeries was significant (P=0.000). Lens aspiration was significantly associated with PCR compared with other types of cataract surgeries (P=0.020). ECCE was also associated with significant rate of PCR compared to the other techniques (P=0.003). The highest rate of PCR complication was seen in phaco (38.4%), followed by ICCE (20.5%), lens aspiration (8.7%), ECCE (6.1%) and the least was with cases where phaco was converted to ECCE (3.8%). In a national population survey of 2 717 203 eyes undergoing cataract surgery over 4y in France, there was a higher proportion of PCR in ECCE compared to phaco (P<0.0001)[10]. In a comparison of phaco and ECCE in eyes with pseudoexfoliation syndrome, small pupil and slight to moderate phacodonesis, Katsimprisetal[11]found that PCR occurred more in the ECCE group compared to phaco. Thevietal[12]also found significantly more PCR in ECCE compared to phaco (P=0.044).
When done in combination, only filtering surgery done with cataract surgery (P=0.012) and miscellaneous combined surgeries (P=0.001) were significantly associated with the occurrence of PCR. Cataract surgeries done along with pterygium excision, penetrating keratoplasty, vitreo-retinal surgery or any other form of combined surgery was not associated with PCR. We could not find any studies that reported the significance of PCR in combined surgery. A few studies have only reported the incidence of PCR in specific combined surgeries. Mochzukietal[13]found that only 1.7% (2 eyes) out of 117 eyes undergoing phaco combined with pars plana vitrectomy (PPV) had PCR intraoperatively. PCR occurred in 5% (2 eyes) out of 38 eyes that underwent PPV for macula hole surgery in a study by Theocharisetal[14]. Skorpiketal[15]reported only 3 cases of PCR in 26 eyes that underwent combined trabeculectomy with cataract surgery.
The vision was compromised by the occurrence of PCR. More patients with PCR got impaired vision (8.3%) compared to good vision (3.7%) and this was significant (P=0.000). Also, more patient got poor vision (10.2%) compared to good vision (3.7%) and this was also statistically significant (P=0.000). The aim of cataract surgery was to give the patient good vision, and it was not achieved when the patient got a PCR complication. Tietal[8]in their 5-year audit also found that eyes without PCR had significantly better vision than eyes with PCR (P<0.01). Wilczyńskietal[16]also found that those with PCR were 5 times more likely to get vision worse than 0.5 compared to those without PCR (P<0.001). Ionidesetal[17]found that eyes with PCR were 3.8 times more likely to get vision of worse that 6/12.
We did not study if the type of intraocular lens inserted following PCR affected the outcome of vision. However, Johansenetal[18]found that those with anterior chamber intraocular lenses had worse vision than those with posterior chamber intraocular lenses.
PCR was significantly associated with poor visual outcome compared to the occurrence of other types of intraoperative complications (P=0.000). Although there are a number of studies about intraoperative complications, we did not find any study comparing each complications with visual outcome. The outcomes of cataract surgeries were significant according to the grade of surgeon, whether there were PCRs or not. Good outcomes were significantly more among specialists (84.3%) compared to trainees (81.2%) (P=0.001). Dayetal[19]in the analysis of the Royal College of ophthalmologists’ database did not find an association of outcomes based on the grade of surgeon. In the presence of PCR, specialists also significantly got better outcomes (70.7%) compared to trainees (63.2%) (P=63.2%). It is interesting to note that even for poor vision following PCR, the specialists had more cases of poor outcomes (11%) compared to trainees (7.4%). Ionidesetal[17]could not find a statistically significant difference between grade of surgeon and the visual outcome following PCR.
No difference was found in the occurrence of PCR among complicated cataracts whether operated byspecialists or by trainees (P=0.281).The commonest reasons for not obtaining good visual acuity following PCR were pre-existing ocular comorbidity (33, 5.3%) and high astigmatism (4.0%). Other causes were CME 7(1.1%) and PCO 5 (0.8%). Lesser causes of not obtaining good visual acuity were cornea decompensation 3 (0.3%), RD 2 (0.3%), infective endophthalmitis 1 (0.2%) and IOL decentration/ dislocation 1(0.2%).Similar to our study, Trinavaratetal[20]found that preexisting ocular disease had worse visual acuity. We found that high astigmatism was the commonest cause for not getting good vision, and they found that incisions requiring more than 2 sutures did not obtain good vision.
We did not use triamcinolone to stain the vitreous following PCR. In the study of 17 patients in the triamcinolone group and 34 patients in the no-triamcinolone group, Kasbekaretal[21]found that 3 patients in the no triamcinolone group developed CME. It is therefore, a good idea to do a complete vitrectomy with triamcinolone in order to prevent CME.
PCR is the commonest intraoperative complication and is the commonest intraoperative complication which causes poor vision. No technique is superior to the other as it occurs significantly in all types of cataract surgeries. For combination surgeries, it is better to do filtering surgeries and miscellaneous surgeries after trauma as separate procedures from cataract surgery, as PCR occurs significantly when combined with filtering and miscellaneous surgeries such as anterior chamber washout, and post cornea-scleral T&S suture removal.
REFERENCES
1 Zainal M, Ismail SM, Ropilah AR, Elias H, Arumugam G, Alias D, Fathilah J, Lim TO, Ding LM, Goh PP. Prevalence of blindness and low vision in Malaysian population: results from the National Eye Survey 1996.BrJOphthalmol2002;86(9):951-956
2 Evi; an Amazon Company. The population of Malacca City in 2014 was around 474 000. Available at: https://www.evi.com/q/melaka_population_2014. Accessed at Aug. 17th, 2015
3 Narendran N, Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM, Asaria RH, Galloway P, Sparrow JM. The Cataract National Dataset electronic multicentre audit of 55 567 operations: risk stratification for posteriorcapsule rupture and vitreous loss.Eye(Lond) 2009;23(1):31-37
4 Thanigasalam T, Sahoo S, Kyaw Soe HH. Posterior Capsule Rupture during Phacoemulsification among Patients with Pseudoexfoliation-Is There A Correlation?MalaysJMedSci2014;21(4):51-53
5 Turalba A, Payal AR, Gonzalez-Gonzalez LA, Cakiner-Egilmez T, Chomsky AS, Vollman DE, Baze EF, Lawrence M, Daly MK. Cataract Surgery Outcomes in Glaucomatous Eyes: Results From the Veterans Affairs Ophthalmic Surgery Outcomes Data Project.AmJOphthalmol2015;160(4): 693-701
6 Johnston RL, Taylor H, Smith R, Sparrow JM. The Cataract National Dataset electronic multi-centre audit of 55 567 operations: variation in posterior capsule rupture rates between surgeons.Eye(Lond) 2010;24(5):888-893
7 Chen M, Lamattina KC, Patrianakos T, Dwarakanathan S. Complication rate of posterior capsule rupture with vitreous loss during phacoemulsification at a Hawaiian cataract surgical center: a clinical audit.ClinOphthalmol2014;8:375-378
8 Ti SE, Yang YN, Lang SS, Chee SP. A 5-year audit of cataract surgery outcomes after posterior capsule rupture and risk factors affecting visual acuity.AmJOphthalmol2014;157(1): 180-185
9 Thanigasalam T, Sahoo S, Ali MM. Posterior capsule rupture with/without vitreous loss during phacoemulsification in a hospital in malaysia.AsiaPacJOphthalmol(Phila) 2015;4(3):166-170
10 Daien V, Le Pape A, Heve D, Carriere I, Villain M. Incidence and characteristics of cataract surgery in france from 2009 to 2012: a national population study.Ophthalmology2015;122(8):1633-1638
11 Katsimpris JM, Petropoulos IK, Apostolakis K, Feretis D. Comparing phacoemulsification and extracapsular cataract extraction in eyes with pseudoexfoliation syndrome, small pupil, and phacodonesis.KlinMonblAugenheilkd2004;221(5):328-333
12 Thevi T, Reddy SC, Shantakumar C. Outcome of phacoemulsification and extracapsular cataract extraction: A study in a district hospital in Malaysia.MalaysFamPhysician2014;9(2):41-47
13 Mochizuki Y, Kubota T, Hata Y, Miyazaki M, Suyama Y, Enaida H, Ueno A, Ishibashi T. Surgical results of combined pars plana vitrectomy, phacoemulsification and intraocular lens implantation.EurJOphthalmol2006;16:279-286
14 Theocharis IP, Alexandridou A, Gili NJ, Tomic Z. Combined phacoemulsification and pars plana vitrectomy for macula hole treatment.ActaOphthalmolScand2005;83(2):172-175
15 Skorpik C, Gnad HD, Paroussis P, Menapace R. Trabeculectomy and intraocular lens implantation: a combined procedure.JCataractRefractSurg1987;13(1):39-42
16 Wilczynski M, Wilczynska O, Synder A, Omulecki W. Incidence and functional outcome of phacoemulsification complicated by posterior capsular rupture.KlinOczna2009;111(1-3):26-29
17 Ionides A, Minassian D, Tuft S. Visual outcome following posterior capsule rupture during cataract surgery.BrJOphthalmol2001;85(2): 222-224
18 Johansen J, Theodorsen FP, Corydon L. Visual outcome following complicated extracapsular cataract extraction.JCataractRefractSurg1992;18(6):577-581
19 Day AC, Donachie PH, Sparrow JM, Johnston RL; Royal College of Ophthalmologists’ National Ophthalmology Database. The Royal College of Ophthalmologists' National Ophthalmology Database study of cataract surgery: report 1, visual outcomes and complications.Eye(Lond) 2015;29(4):552-560
20 Trinavarat A, Neerucha V. Visual outcome after cataract surgery complicated by posterior capsule rupture.JMedAssocThai2012;95 Suppl 4:S30-35
21 Kasbekar S, Prasad S, Kumar BV. Clinical outcomes of triamcinolone-assisted anterior vitrectomy after phacoemulsification complicated by posterior capsule rupture.JCataractRefractSurg2013;39(3):414-418
DOI:10.3980/j.issn.1672-5123.2016.4.03
通讯作者:Thanigasalam Thevi. 111thevi@gmail.com
目的:观察后囊破裂的诱发因素、相关性及结果。
方法:回顾性研究。研究对象为2007~2014年我院出现后囊破裂患者。研究后囊破裂与眼部合并症、晶状体相关并发症、手术水平、手术类型、独立手术或联合手术的相关性,及患者最终视力情况。
结果:在12 846名患者中,后囊破裂是最常见的术中并发症(n=623, 4.8%)。眼部合并症和晶状体状态不会引起后囊破裂。手术者的经验和资历与后囊破裂发生的相关性显著。基层医务人员手术时出现后囊破裂比知名专家多(P=0.0000),而知名专家手术时出现后囊破裂情况反而比一般专家多(P=0.000)。白内障手术中出现后囊破裂与下列手术方式显著相关:超声乳化术、超乳转囊外摘除术及囊内摘除术(P=0.000),晶状体吸出术(P=0.020)和白内障囊外摘除术(P=0.003)。术中发生(P=0.013)与未发生(P=0.001)后囊破裂时,专家均比学员的手术结果好。尽管如此,在复杂病例中,专家与学员术中出现后囊破裂无显著差异。后囊破裂致视力损害的主要原因是散光。视力丧失(P=0.000)和低视力(P=0.000)出现较多。相对于其它并发症,后囊破裂更易致低视力。
结论:后囊破裂会发生在所有类型的白内障手术中,且是引起术后低视力的主要术中并发症。专家在处理后囊破裂的手术结果优于学员。因而初级外科医生应加强手术练习。
引用:Thevi T, Maizura MZ. 马来西亚综合医院后囊破裂的诱发因素与相关性及结果分析.国际眼科杂志2016;16(4):600-606