Effect of rapid point pressure on therapeutic efficacy and pulmonary function in patients with chronic persistent bronchial asthma
Clinical Study
Effect of rapid point pressure on therapeutic efficacy and pulmonary function in patients with chronic persistent bronchial asthma
Objective: To observe the effect of rapid point pressure on clinical effect and pulmonary function of patients with chronic persistent bronchial asthma.
Point Therapy; Point Pressure Therapy; Asthma; Respiratory Function Tests
1 Clinical Data
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in traditional Chinese medicine (TCM)
This was based on the diagnosis for asthma in the Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[2]: recurrent wheezing, difficulty breathing or breathing with the mouth open and shoulder lifted in severe cases, an inability to lie flat, cyanosis of the lips and fingernails; inducing factors include a sudden weather change, improper diet, emotional disturbance and fatigue; warning signs include a scratchy nose, sneezing, coughing, and chest tightness; a family history or an allergic history; wheezing sound or moist rales; elevated eosinophil; presence of acidophil in sputum smear; and absence of noticeable changes by chest X-ray and possible presence of emphysema in patients with a long duration.
1.1.2 Diagnostic criteria in Western medicine
This was based on diagnostic criteria for asthma in the Prevention and Treatment Guidelines for Bronchial Asthma by the Asthma Working Group, Chinese Society of Respiratory Diseases, Chinese Medical Association[1]: recurrent episodes of wheezing, shortness of breath, chest tightness, and coughing that are often associated with contact with allergens, cold air, physical or chemical irritation, upper respiratory tract viral infection and exercise; scattered or diffuse wheezing sound with a prolonged expiratory phase; the above symptoms can alleviate spontaneously or through treatment; patients with atypical symptoms (no shortness of breath or other signs) shall meet at least one of the following items: positive results of bronchial provocation test or exercise test, 12% or more increase of forced expiratory volume in 1 second (FEV1), more than 200 mL of absolute value increase and more than 20% of daily aberration rate or diurnal fluctuation of peak expiratory flow (PEF); shortness of breath, chest tightness and coughing due to other medical causes shall be ruled out.
Patients with chronic persistent asthma experience shortness of breath, chest tightness, and coughing that vary in severity on a weekly basis for an extended period of time.
1.2 Inclusion criteria
Those who met the above diagnostic criteria in Chinese and Western medicine; aged between 18 and 55 without a smoking history; having no complications of pneumonia, pulmonary tuberculosis and a bad cold; having no severe cardiac insufficiency; having no complications of major diseases involving the vascular, liver, kidney and hematopoietic systems; having no mental disorders; and women who are neither pregnant nor breast feeding.
1.3 Exclusion criteria
Patients in persistent asthma or critical conditions; having complications of cardiac insufficiency; having complications of major diseases involving the vascular, liver, kidney and hematopoietic systems; having mental disorders; pregnant or breast feeding women; those who are allergic to drugs in this study; and those who fail to follow the treatment protocol or have incomplete data.
1.4 Statistical method
The Windows Excel datasheet software was used to record experimental data. The statistical analysis was done using the SPSS 17.0 version software. As for descriptive statistics, mean ± standard deviation (x ±s) was used to express normal distribution of numerical value; and the median and interquartile distances were calculated for skewed distribution. As for differences between observed number and baseline in different time frames before and after treatment of each patient, independent sample t-test was used for normal distribution coupled with equal analysis of variance; otherwise the rank sum test was used for inter-group comparison. If α=0.05 is employed in all tests of hypothesis, a P value of less than 0.05 indicates a statistical significance.
1.5 General materials
A total of 60 chronic persistent bronchial asthma patients treated in Shuguang Hospital, Shanghai University of Traditional Chinese Medicine between August 2012 and August 2013 were randomly allocated into a treatment group and a control group, 30 in each group. There were no between-group statistical significances in baseline data such as gender, age, severity and symptom scores (P>0.05), indicating that the two groups were comparable (Table 1).

Table 1. Between-group comparison of general materials
2 Treatment Methods
2.1 Treatment group
Patients in the treatment group received rapid point pressure therapy.
Method: The patient was asked to take a prone lying position. The practitioner applied 10 min of Tanboplucking manipulation to three segments along the pathway on the leg [from Zhubin (KI 9) to Yingu (KI 10); from Yingu (KI 10) to Henggu (KI 11); from Weiyang (BL 39) to Kunlun (BL 60), Figure 1]; then applied 10 min of point pressure along the Governor Vessel (from top to bottom), especially the points between Baihui (GV 20) and Mingmen (GV 4); after this, applied 10 min of Tanbo-plucking manipulation to Dingchuan (EX-B 1) and the Bladder Meridian, especially from Fengmen (BL 12), Feishu (BL 13) to Shenshu (BL 23) and from Gaohuang (BL 43) to Geguan (BL 46). Finally, the patient was asked to change to a supine lying position, the practitioner applied 10 min of point pressure to 10 points on the ribs (the crossing points between the manubrium and intercostal space 1 through 5) and points along the Conception Vessel, especially Tiantu (CV 22), Danzhong (CV 17), Zhongwan (CV 12), Shenque (CV 8) and Qihai (CV 6).

Figure 1. Three segments on the leg
The first treatment lasted for 1 h and the rest treatments lasted for 40 min. The treatment was done once a day for 40 times. A 1-year follow-up was then performed.
2.2 Control group
Patients in the control group took oral Compound Methoxyphenamine Hydrochloride Capsules (Asmeton) manufactured by Daiichi Sankyo (Shanghai) Company Limited (batch number: 110950), 2 capsules for each dose, 3 times a day, for 7 consecutive days and 1-year follow up.
In case of no alleviation or aggravation, patients in both groups can temporarily use Ventolin inhale, 2 inhalations for each dose. The frequency of Ventolin inhalation was recorded on a daily basis.
3 Therapeutic Efficacy Observation
3.1 Measurements
3.1.1 Clinical signs and symptoms
The TCM symptoms scores (including coughing, expectoration, shortness of breath, chest tightness, and wheezing) and total symptom scores before treatment, 7 d after treatment, 40 d after treatment and after 1-year follow-up were all recorded for observation indexes. According to the Guiding Principles for Clinical Study of New Chinese Medicines[3], the signs and symptoms including coughing, expectoration, shortness of breath, chest tightness and wheezing were graded as absent, mild, moderate and severe and scored 0, 2, 4 and 6. The therapeutic efficacy indexes and total scores were then calculated by the scores of signs and symptoms.
3.1.2 Pulmonary functions
The pulmonary functions of patients were examined using the JAEGER-ML3500 instrument made in Germany. The PEV percentage of predicted value (FEV 1%), PEV to forced vital capacity ratio (FEV1/FVC), maximum midexpiratory flow rate (MMEF%), PEF rate (PEF%) and inspiratory capacity (IC%) before treatment and 40 d after treatment were all recorded as measurements.
3.2 Therapeutic efficacy criteria
This was based on the Guiding Principles for Clinical Study of New Chinese Medicines[3]. The therapeutic efficacy index was calculated using Nimodipine method according to the scores of signs and symptoms.
Therapeutic efficacy index = (Pre-treatment score— Post-treatment score) ÷ Pre-treatment score × 100%.
Clinical recovery: Therapeutic efficacy index ≥95%.
Marked effect: Therapeutic efficacy index ≥70% and≤94%.
Improvement: Therapeutic efficacy index ≥30% and≤69%.
Failure: Therapeutic efficacy index <30%.
3.3 Treatment results
3.3.1 Evaluation of overall therapeutic efficacy in the two groups
Among 60 cases in the two groups, there were no drop-outs. After 7 d of treatment, the total effective rate in the treatment group was 53.3%, versus 3.3% in the control group, showing a statistical significance (P<0.01) and a better effect in the treatment group. After 40 d of treatment, the total effective rate in the treatment group was 76.7%, versus 56.7% in the control group, showing no between-group statistical significance (P>0.05). After 1-year follow-up, the total effective rate in the treatment group was 26.7%, versus 16.7% in the control group, showing no between-group statistical significance (P > 0.05). This indicates that rapid point pressure therapy can obtain a better short-term effect than oral Asmeton and a similar long-term effect with Asmeton (Table 2).
3.3.2 Between-group comparison of TCM symptom scores after 7 d of treatment
Since the symptom score and total symptom scores before treatment, 7 d after treatment, 40 d after treatment and after 1-year follow-up in both groups showed normal distribution, mean ± standard deviation (x ±s) was used for descriptive statistics and t-test was used for comparison.
After 7 d of treatment, the symptom score and total symptom scores were significantly improved in the treatment group (both P<0.01), indicating substantial alleviation of symptoms. As for the control group, except for statistical significances in wheezing score and total symptom scores (P<0.01, P<0.05), there were no statistical significances in scores of other symptoms (P>0.05).
Regarding the between-group comparison of differences in symptom score and total symptom scores before and after treatment, there were between-group statistical significances in coughing and expectoration (P<0.05), chest tightness, wheezing and total symptom scores (P<0.01), indicating a better effect for coughing, expectoration, chest tightness, wheezing and overall symptom alleviation in the treatment group than those in the control group (Table 3).

Table 2. Between-group comparison of therapeutic efficacy (case)

Table 3. Between-group comparison of TCM symptom scores after 7 d of treatment (x ±s, point)
3.3.3 Between-group comparison of TCM symptom scores after 40 d of treatment
After 40 d of treatment, symptom score and total symptom scores were significantly improved in the treatment group (P < 0.01), indicating a substantial alleviation of symptoms. As for the control group, except for chest tightness, there were statistical significances in shortness of breath, wheezing and total symptom scores (P<0.01) as well as in coughing and expectoration (P < 0.05), indicating a substantial alleviation of symptoms except for chest tightness.
There were no between-group statistical significance in differences of symptom score and total symptom scores before and after treatment (P>0.05), indicating that patients in the two groups shared similar alleviation of symptoms after 40 d of treatment (Table 4).
3.3.4 Between-group comparison of TCM symptom scores after 1-year follow-up
As for the treatment group, the 1-year follow-up has shown statistical significances in scores of shortness of breath, coughing and expectoration and total symptom scores (both P<0.01) as well as wheezing (P<0.05), indicating a substantial alleviation of symptoms except for chest tightness in the treatment group. As for the control group, the 1-year follow-up has shown statistical significances in total symptom scores (P < 0.01), shortness of breath, coughing and wheezing (P<0.05), indicating a substantial alleviation of symptoms except for expectoration and chest tightness in the control group.
There were no between-group statistical significances in differences of symptom score and total symptom scores before and after treatment (both P>0.05), indicating that patients in the two groups shared similar alleviation of symptoms after 1-year follow-up (Table 5).
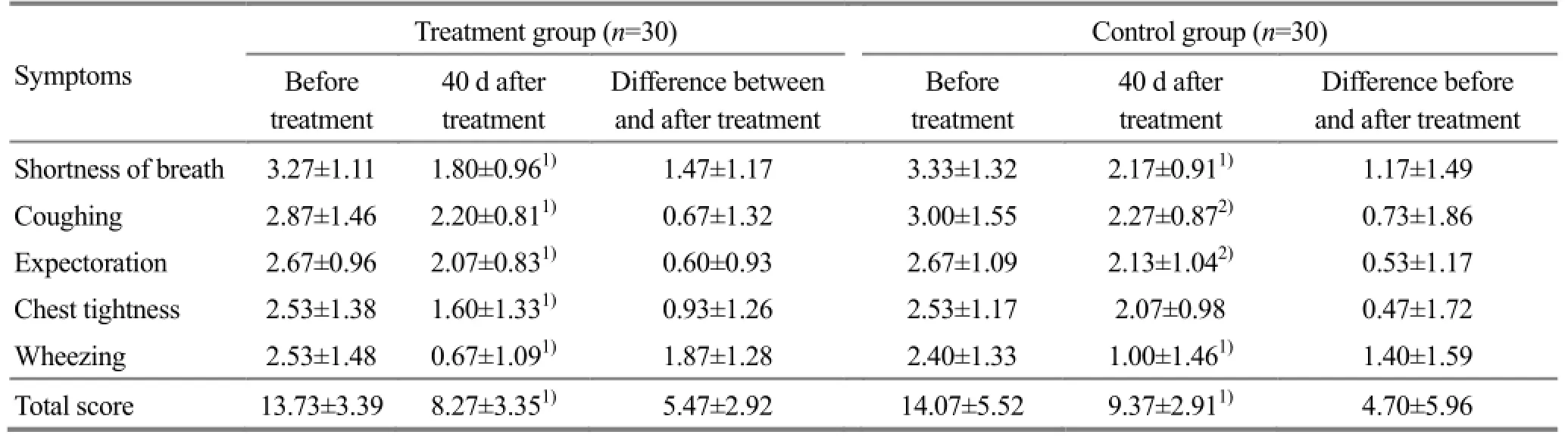
Table 4. Between-group comparison of TCM symptom scores 40 days after treatment (x ±s, point)
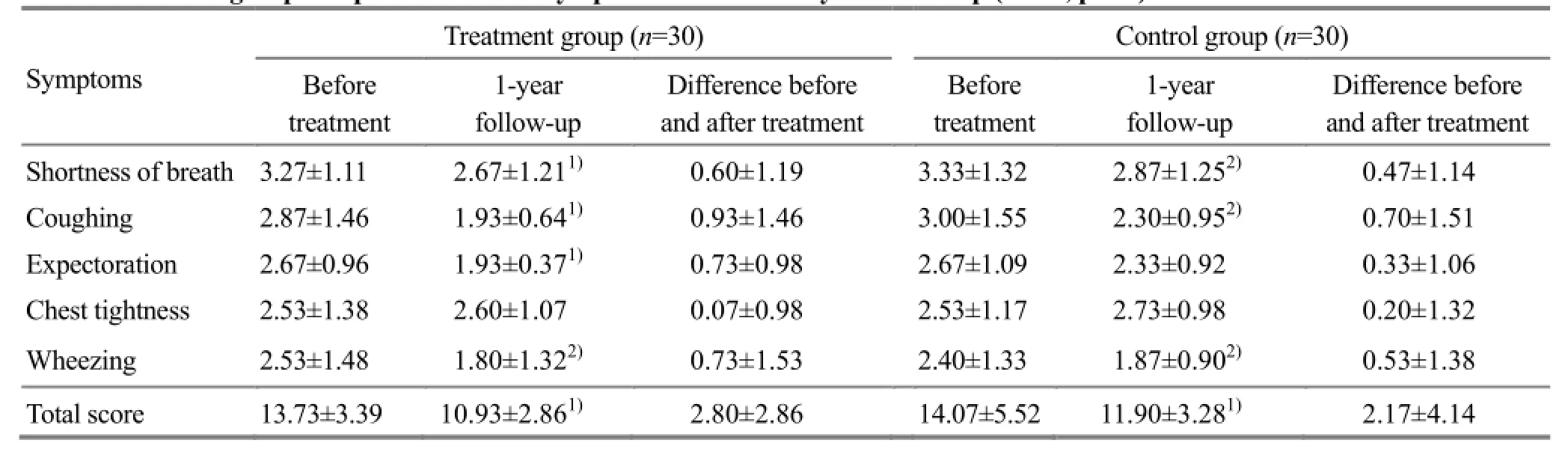
Table 5. Between-group comparison of TCM symptom scores after 1-year follow-up (x ±s, point)
3.3.5 Between-group comparison of total TCM symptom scores in different time frames before and after treatment
Before treatment, there were no between-group statistical significances in total TCM symptom scores (P > 0.05). There were between-group statistical significances 7 d after treatment, 40 d after treatment and after 1-year follow-up (P<0.05). In addition, the total TCM symptom scores in the treatment group were lower than that in the control group in all time frames, especially the scores after 7 d of treatment that showeda between-group statistical significance (P<0.01). After 40 d of treatment, the total TCM symptom scores in both groups were further lower; however, there were no between-group statistical significances. The 1-year follow-up has shown an increase of TCM symptom scores in both groups; however, there were no between-group statistical significances. This indicates that clinical symptoms were alleviated in both groups, the short-term effect in the treatment group was better than that in the control group; however, there were no between-group statistical significances in long-term effect (Figure 2).
3.3.6 Between-group comparison of pulmonary functions before and after treatment
Since pulmonary function parameters of patients in both groups and differences before and after treatment showed normal distribution, mean ± standard deviation (x ±s) was used for descriptive statistics and t-test was used for comparison. Before treatment, there were no between-group statistical significances in pulmonary function parameters (P>0.05), indicating that the two groups were comparable. After 40 d of treatment, there were statistical significances in FEV1% and IC% (P<0.05) in the treatment group. As for the control group, there were no statistical significances in five pulmonary function parameters before and after treatment (P>0.05). In addition, there were no between-group statistical significances in differences of five pulmonary function parameters between before and after treatment (P>0.05). This indicates that there were significant pulmonary function changes in both groups 40 d after treatment, probably because patients in remissive states of asthma basically have normal pulmonary functions (Table 6).

Figure 2. Between-group comparison of total TCM symptom scores in different time frames
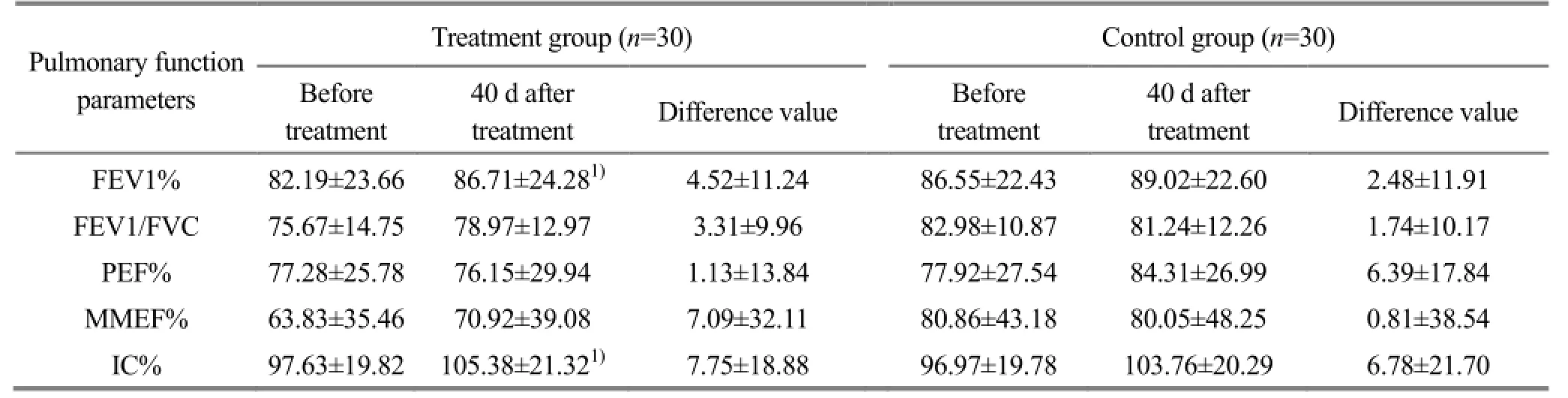
Table 6. Between-group comparison of pulmonary function parameters 40 d after treatment (x ±s)
4 Discussion
Bronchial asthma can greatly endanger people’s health. Over the recent years, its incidence tends to increase with the aggravation of environmental pollution. Due to compromised defense ability of the body and respiratory tract, asthma patients are susceptible to recurrent respiratory tract infection. This can affect patients’ quality of life and increase family and social economic burden. Numerous studies have been conducted on asthma. In TCM, a variety of therapies can be used for asthma, such as cupping after bloodletting[4], auricular point sticking[5], point application[6]and point injection[7]. All these methods have some effects, however, they all have limitations in the control of recurrent episodes. Currently, there are no breakthroughs, especially no recognized protocol to prevent asthmatic recurrence.
In TCM, the root cause of bronchial asthma is deficiency of the lung, spleen and kidney; however, it often has excessive manifestations of phlegm, turbidity and stasis. Since the lung dominates qi and the kidney absorbs qi, the lung and kidney work together to maintain normal breathing. Kidney essence or kidney yang deficiency can affect the function of the kidney in absorbing qi. This can further affect the function of the lung in dominating qi and result in coughing. Evidently, kidney deficiency is the root of asthma. The spleen is the source of phlegm generation. Spleen deficiency can cause internal phlegm dampness to obstruct qi activitiesof the lung, spleen and kidney, leading to qi stagnation and blood stasis. Consequently, the treatment principle is to treat symptoms of the lung from the spleen and kidney. Since patients with chronic asthma have hypofunction of the pituitary gland-adrenal cortex axis, adrenal cortical hormone can alleviate shortness of breath in asthmatic episodes.
Rapid point pressure therapy in this study was developed by Mr. Jiang Ke-ding, who accidently found that unblocking three meridian segments [i.e., from Zhubin (KI 9) to Yingu (KI 10), from Yingu (KI 10) to Henggu (KI 11) and from Weiyang (BL 39) to Kunlun (BL 60)]can resolve kidney deficiency in a timely manner. In TCM, the kidney is the congenital base, root of life and origin of constitution, kidney deficiency can therefore result in health problems. Because kidney deficiency is the underlying cause of asthma, we intend to use this method in this study to observe its clinical effect on chronic persistent bronchial asthma.
Rapid point pressure therapy can resolve kidney deficiency in a timely manner by unblocking three meridian segments on the leg. Since the Governor Vessel governs yang qi of the entire body and is known as the sea of yang meridians[8], yang qi deficiency of the Governor Vessel can cause hypofunctions of the Zang-fu organs and insufficient generation of qi, blood and body fluids; and failure of yang to warm and transport can cause water retention, phlegm turbidity and blood stagnation. Qi of the body is closely associated with the kidney, spleen and lung. In addition, these three meridians are all yin meridians and Conception Vessel is the sea of yin meridians. As a result, qi-regulating points are mostly distributed in the Conception Vessel, such as Danzhong (CV 17), Zhongwan (CV 12) and Qihai (CV 6)[9]. Rapid point pressure therapy on the Conception and Governor Vessels can warm yang and supplement qi. Located near the Governor Vessel, back-Shu points are indicated for problems of corresponding zang-fu organs. In this study, Feishu (BL 13), Pishu (BL 20) and Shenshu (BL 23) were selected to benefit the lung, fortify the spleen and benefit the kidney. This can further strengthen the immune system[10-12]. Dingchuan (EX-B 1) can connect qi of the Bladder Meridian with the Governor Vessel, alleviate shortness of breath and stop coughing[13-15]. Points on ten ribs can open the airway. When used in combination, the aforementioned points can resolve phlegm, alleviate shortness of breath, supplement qi and treat both the root cause and external manifestations[16-17].
The findings of this study have suggested that rapid point pressure can significantly alleviate symptoms of chronic persistent bronchial asthma, improve FEV1% and IC% and is therefore worthwhile for further study and promotion.
Conflict of Interest
There was no conflict of interest in this article.
Acknowledgments
This work was supported by the 3-year Action Plan for Shanghai Development of Traditional Chinese Medicine (No. ZYSNXD-CC-ZDYJ055).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Received: 10 August 2014/Accepted: 25 September 2014
[1]Asthma Working Group, Chinese Society of Respiratory Diseases, Chinese Medical Association. Prevention and treatment guidelines for bronchial asthma (definition, treatment and management protocol of bronchial asthma). Zhonghua Jiehe He Huxi Zazhi, 2008, 31(3): 177-185.
[2]State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Nanjing: Nanjing University Press, 1994: 77.
[3]Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medico-Pharmaceutical Science & Technology Publishing House, 2002: 56-58.
[4]Geng LM, Yu XY. Mechanism of effect of collateral-pricking with ventouse on bronchial asthma at chronic persistent period. Zhonguo Quanke Yixue, 2011, 14(3A): 801-803.
[5]Luo S, Li JX, Ling MH. Clinical effect observation on treating chronic persistent asthma by auricular point sticking. CJCM, 2013, 5(7): 43-45.
[6]Li LP. Clinical observation on point application in preventing and treating bronchial asthma. Shanghai Zhenjiu Zazhi, 2013, 32(2): 96-98.
[7]Xu J, Zheng S, Fang W. Role of combining spreading moxibustion and point injection in reducing ECP and LPO levels and improving lung function. J Acupunct Tuina Sci, 2014, 12(1): 12-16.
[8]Ye Z, Chen LD. Research survey on needling the Governor Vessel for post-stroke cognitive dysfunction. Yatai Chuantong Yiyao, 2013, 9(4): 73-74.
[9]Dai SQ, Yang QL. Differentiation and analysis of qi-regulating points in the Conception Vessel. Beijing Zhongyi, 2003, 22(3): 46-48.
[10]Huang TJ, Luo XH. The progress of experimental researches on the acupuncture treatment of bronchial asthma. Chin J Nat Med, 2000, 2(4): 235-240.
[11]Xie YL. Development of researches and clinical application on treatment of bronchial asthma withacupuncture. Liaoning Zhongyiyao Daxue Xuebao, 2011, 13(1): 201-204.
[12]He J, Bi WQ, Zhuang LX, Wang WH, Zhuang X, Huang LY. Clinical study on vesiculation moxibustion in preventing and treating asthma due to cold deficiency. Shanghai Zhenjiu Zazhi, 2014, 33(1): 34-37.
[13]Hui P, Song TY, Fan FC, Li YJ, Wang XP, Chen ZN, Liang YS, Liu WZ, Peng JQ. Clinical study on Chuankezhi point injection in treatment of acute attack of bronchial asthma with cold syndrome and deficiency of kidney-yang and its effects on IFN-γ and IL-4. Hunan Zhongyiyao Daxue Xuebao, 2013, 33(3): 78-80.
[14]Chen LF, Fang JQ, Jia LH, Jin XQ, Jiang ZX. Effect of BCG-PSN acupoint injection on IgE content and asthma control test score of bronchial asthma. Zhongyi Zazhi, 2013, 54(14): 1207-1210.
[15]Gu W, Zhou CX, Yan Y. Immune regulation of Th/Th2 imbalance in allergic asthma guinea pigs by acupoint application. CJTCMP, 2013, 28(6): 1689-1691.
[16]Liu ZB, Niu XM. Study progress on tuina for bronchial asthma. Shaanxi Zhongyi Xueyuan Xuebao, 2008, 31(3): 67-69.
[17]Wang TY. Shi CX. Clinical observation on acupoint massage for bronchial asthma. Jiaotong Yixue, 1997, 11(2): 251.
Translator: Han Chou-ping (韩丑萍)
点穴快速疗法对支气管哮喘慢性持续期患者临床疗效及肺功能的影响
Shi Miao-yan (史苗颜)1, Shu Zi-tong (舒子童)2, Zhang Wei (张炜)1, Tian Jun (田君)1
1 Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai 200021, China
2 Department of Internal Medicine, Chang’an Hospital, Zhongxiang City, Hubei 431900, China
目的:观察快速点穴治疗支气管哮喘慢性持续期的疗效及其对肺功能的影响。方法:将 60例支气管哮喘慢性持续期患者随机分为两组,每组 30 例。治疗组用快速点穴疗法,首次点穴治疗 1 h, 以后每次治疗 40 min,每日 1 次,连续治疗 40 次。对照组口服复方甲氧那明胶囊(Compound Methoxyphenamine Hydrochloride Capsules),每次 2 粒,每日 3 次。连续治疗 7 d。两组均随访 1 年。结果:治疗后,治疗组各症状积分及症状总积分改善值均明显优于对照组(P<0.05);两组各个时间点总有效率比较,治疗组均高于对照组,且在治疗 7 d 后的总有效率与对照组有统计学差异(P<0.01)。治疗 40 d 后两组肺功能指标比较,治疗组第一秒用力呼气容积占预计值比值(forced expiratory volume in 1 second percentage of predicted value,FEV1%)、深吸气量(inspiratory capacity,IC%)均与治疗前有统计学差异(P<0.05),第一秒用力呼气容积占用力肺活量的比值(forced expiratory volume in 1 second to forced vital capacity ratio,FEV1/FVC)、呼吸峰流速(peak expiratory flow rate,PEF%)及最大呼气中段流率(maximum midexpiratory flow rate,MMEF%)差异均无统计学意义(P>0.05);对照组肺功能各项指标与治疗前均无统计学差异(P>0.05);两组肺功能指标治疗前后差值均无统计学差异(P>0.05)。结论:快速点穴可改善患者中医证候,对肺功能中的 FEV1%、IC%有改善。
穴位疗法; 点穴疗法; 哮喘; 呼吸功能测试
R244.1
ABronchial asthma is a chronic inflammatory disorder of the airways in which many cells (including eosinophil, mastocytes, T lymphocytes, neutrophils, smooth muscle cell and epithelial cells of the airways, etc) and cellular elements play a role. The chronic inflammation is associated with airway hyper-responsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness and coughing[1]. This condition can greatly endanger people’s health and is now attracting more attention in research. At present, there are no specific long-acting therapies for chronic persistent bronchial asthma. Although the rapid point pressure therapy developed by Mr. Jiang Ke-ding has shown to be effective in clinical practice, it still needs rigorous clinical trials. We conducted this trial to verify its clinical efficacy and explore the underlying mechanism. The results are now summarized as follows.
Author: Shi Miao-yan, master of medicine, associate chief physician
Zhang Wei, master of medicine, chief physician. E-mail: zhangw1190@sina.com
Shi MY, Shu ZT, Zhang W, et al. Effect of rapid point pressure on therapeutic efficacy and pulmonary function in patients with chronic persistent bronchial asthma. J Acupunct Tuina Sci, 2015, 13 (1): 36-43
10.1007/s11726-015-0820-3
Methods: A total of 60 confirmed chronic persistent bronchial asthma cases were randomly allocated into two groups, 30 in each group. Cases in the treatment group were treated with rapid point pressure, 1 h for the initial treatment, and 40 min for the ensuing treatments. The treatment was done once a day for 40 d. Cases in the control group were treated with Compound Methoxyphenamine Hydrochloride Capsules, 2 capsules for each dose, 3 times a day. The treatment lasted for 7 consecutive days. A 1-year follow-up was made for both groups.
Results: After treatment, the scores of each symptom and total symptom scores for the traditional Chinese medicine (TCM) symptoms in the treatment group were significantly higher than those in the control group (P<0.05); the total effective rates in the treatment group were higher than those in the control group in each time frame; and there was a between-group statistical significance in total effective rate after 7 d of treatment (P<0.01). After 40-day treatments, there were statistical significances in the forced expiratory volume in 1 s percentage of predicted value (FEV 1%) and inspiratory capacity (IC%) in the treatment group (P<0.05); however, there were no statistical significances (P>0.05) in forced expiratory volume in 1 second to forced vital capacity ratio (FEV1/FVC), peak expiratory flow rate (PEF%) and maximum midexpiratory flow rate (MMEF%); and there were no statistical significances in pulmonary function parameters in the control group. In addition, as for pulmonary function parameters, there were no intra-group statistical significances in differences before and after treatment (P>0.05).
Conclusion: Rapid point pressure can alleviate patients’ TCM symptoms and improve their FEV% and IC%.
 Journal of Acupuncture and Tuina Science2015年1期
Journal of Acupuncture and Tuina Science2015年1期
- Journal of Acupuncture and Tuina Science的其它文章
- 复式针刺补泻对臀大肌挛缩术后髋关节和膝关节屈伸角度的影响
- 电针对脑缺血再灌注模型大鼠血清白介素的影响
- 隔药灸天枢和气海对慢性炎性内脏痛大鼠痛行为和痛情绪的影响
- Clinical observation on warm needling in canicular days for knee osteoarthritis
- Observation on clinical effect of electroacupuncture plus pricking-cupping bloodletting therapy for herpes zoster
- Observation on clinical effect of acupuncture plus Zi Shen Tiao Gan Decoction for perimenopausal insomnia
