20例原发性甲状腺淋巴瘤的临床分析
张秉栋,薛勇敢,刘洪一,王白石,贾宝庆
1解放军医学院,北京 100853;2解放军总医院 肿瘤外科,北京 100853
20例原发性甲状腺淋巴瘤的临床分析
张秉栋1,薛勇敢1,刘洪一2,王白石2,贾宝庆2
1解放军医学院,北京 100853;2解放军总医院 肿瘤外科,北京 100853
目的分析原发性甲状腺淋巴瘤的临床表现、诊断、治疗及预后。方法回顾1993年6月- 2013年6月解放军总医院收治的原发性甲状腺淋巴瘤20例,分析其临床表现、诊断经过、治疗方案及预后。按疾病分期及是否接受手术分组,分析不同病理类型患者的生存情况。结果1例入院当天因窒息死亡未做治疗,5例通过超声引导穿刺活检明确诊断后接受化疗或化疗+放疗,14例接受单纯手术、手术+化疗或手术+化疗+放疗。中位随访期为41(0 ~ 131)个月,随访仍未到达终点。3例黏膜相关淋巴组织淋巴瘤(mucosa-associated lymphoma tissue,MALT)患者长期存活;弥漫大B细胞淋巴瘤(diffuse large B-cell lymphoma,DLBCL)ⅠE期2年、5年生存率均为100%(5例),ⅡE期2年、5年生存率分别为72.9%(6例)和58.3%(5例),ⅠE期DLBCL患者预后优于ⅡE期患者(P=0.048)。DLBCL中接受手术患者2年、5年生存率均为74.1%(7例),未接受手术患者(不包括未治疗患者1例)2年、5年生存率分别为100%(4例)和75.0%(3例)。是否接受手术对DLBCL患者预后无显著影响(P=0.804)。结论MALT患者经过治疗可长期存活,ⅠE期DLBCL患者预后优于ⅡE期。手术对DLBCL患者预后无显著影响,外科手术的干预应慎重选择。
甲状腺肿瘤;淋巴瘤;外科手术
淋巴结外恶性淋巴瘤大多发生于扁桃体、胃肠道和纵隔等部位,发生于甲状腺的原发性甲状腺淋巴瘤(primary thyroid lymphoma,PTL)是一种少见疾病,占甲状腺恶性肿瘤的1% ~ 5%[1-3],结外淋巴瘤的2%[1],全部淋巴瘤的1% ~ 2.5%[4],每年每百万人中新发病例数为1 ~ 2例[5-6],多发生于老年人[7],男性比女性早发5 ~ 10年,男女比为1∶2 ~ 1∶14[8-11]。原发性甲状腺淋巴瘤患者常先就诊于外科,如何正确认识外科手术在PTL诊治中的地位是一个很重要的问题。由于该病病例数较少,文献尚未报道前瞻性或随机性研究,最佳的治疗方案存在争议。本研究回顾性分析了解放军总医院收治的原发性甲状腺淋巴瘤病例20例,以探讨原发性甲状腺淋巴瘤病例的诊断、治疗及预后。
资料和方法
1资料来源 我院1993年6月- 2013年6月收治的甲状腺淋巴瘤患者23例,3例因初诊时淋巴瘤已处于Ⅳ期无法判断原发部位被排除在外,剩余20例均为原发性甲状腺淋巴瘤。20例均通过甲状腺穿刺活检或术后病理确诊。
2Ann Arbor分期标准ⅠE PTL伴或者不伴周围软组织侵犯;ⅡE:PTL侵及同侧纵隔淋巴结;ⅢE:PTL侵及纵隔两侧淋巴结和(或)脾;ⅣE:PTLs播散至其他结外部位。
3方法 回顾性分析患者的病历资料,并对患者进行电话随访,了解存活状况、后续治疗情况及死亡原因。按疾病分期及是否接受手术治疗分组,分析不同病理类型患者的生存情况。总生存期(overall survival,OS)被定义为从诊断开始,至因任何原因引起死亡的时间。对于死亡之前就已经失访的受试者,将最后1次随访时间算作死亡时间。
4统计学方法 数据统计采用SPSS软件。采用乘积极限法(Kaplan-Meier法)计算生存率及Logrank检验。P<0.05为差异有统计学意义。
结 果
1一般资料 20例原发性甲状腺淋巴瘤,占我院同期甲状腺恶性肿瘤的0.33%(20/6 038)。男性8例,女性12例,确诊年龄38 ~ 77(64.6±12.77)岁。男性发病平均年龄(69.4±8.58)岁,女性发病平均年龄(61.4±14.4)岁。其中10例伴有桥本甲状腺炎,占原发性甲状腺淋巴瘤患者的50%,占同期桥本甲状腺炎患者的0.27%(10/3 753)。黏膜相关淋巴组织淋巴瘤(mucosa-associated lymphoma tissue,MALT)占原发性甲状腺淋巴瘤患者的15%,弥漫性大B细胞淋巴瘤(diffuse large B-cell lymphoma,DLBCL)为65%,其他类型占20%。诊断前病程0.5 ~ 24个月。
2症状 5例声音嘶哑(4例经纤维喉镜检查证实);5例有吞咽困难;6例出现憋气症状(CT显示气管受压移位),6例甲状腺肿或结节在1 ~ 3个月时迅速增大;1例出现饮水呛咳。具体情况见表1。
3辅助检查 B超显示3例为腺体双侧或单侧叶弥漫增大、低回声、不均质;7例提示在慢性淋巴细胞性甲状腺炎基础上出现腺体内低回声结节,回声不均匀;10例为腺体双侧或单侧叶形态失常伴多发低回声结节。20例行乳酸脱氢酶(LDH)检查均在正常范围。19例行甲状腺功能检查,1例为甲减,9例为亚临床甲减〔球蛋白抗体(TGAb)、TSH高于正常〕,9例甲状腺功能正常。
4病理及分型 5例行术前超声引导下穿刺活检。15例均行术后石蜡病理常规检查。20例中,13例诊断为DLBCL,3例诊断为MALT,4例分别诊断为DLBCL及边缘区B细胞淋巴瘤(marginal zone B-cell lymphoma,MZBL)伴大细胞转化型、MALT局部DLBCL转化、MALT型MZBL部分DLBCL、B细胞淋巴瘤(该例未分亚型)。
5治疗 20例中,1例入院当天因窒息死亡未做治疗,5例通过超声引导穿刺活检明确诊断后接受化疗或化疗+放疗,其余14例接受单纯手术、手术+化疗或手术+化疗+放疗。手术指征为:1)甲状腺超声检查提示恶性或不排除恶性;2)未行甲状腺肿物穿刺活检(甲状腺肿物穿刺活检并未作为常规检查,超声提示肿物为恶性或不排除恶性时建议采用以明确诊断)。所用化疗方案有:COPP(环磷酰胺+平阳霉素+长春新碱+泼尼松)、CHOP(环磷酰胺+阿霉素+长春新碱+泼尼松)、R-CHOP(美罗华+环磷酰胺+长春地辛+表柔比星+泼尼松)、COP(环磷酰胺+长春地辛+甲泼尼龙)、VP(长春新碱+泼尼松)、R-FC(美罗华+氟阿糖腺苷+环磷酰胺)。R-CHOP是应用最多的化疗方案。根据病情化疗2 ~ 6个疗程。放疗放射野为全颈、双侧锁骨上下区、上纵隔,放射剂量为20 ~ 50 Gy,分割10 ~ 25次完成。治疗期间通过PET-CT评估疗效,根据病情调整治疗方案。治疗方式及具体手术方式见表2和表3。
6预后 中位随访期为41(0 ~ 131)个月,随访仍未到达终点。随访期间死亡5例(表4),1例死于术后并发症,1例死于呼吸道压迫窒息,其余3例死于淋巴瘤的复发与扩散。失访2例。根据病理亚型分类,3例MALT分期均为ⅠE,全部存活,随访期分别为96个月、102个月、131个月。13例DLBCL ⅠE期2年、5年生存率均为100%,ⅡE期2年、5年生存率分别为72.9%和58.3%,ⅠE期DLBCL患者预后优于ⅡE期患者(P=0.048)(图1);13例DLBCL中接受手术患者2年、5年生存率均为74.1%,未接受手术患者(不包括未治疗患者1例)2年、5年生存率分别为100%和75.0%。是否接受手术对DLBCL患者预后无显著影响(P=0.804)(图2)。

表1 20例原发性甲状腺淋巴瘤患者一般情况Tab. 1 Characteristics of 20 patients with primary thyroid lymphoma
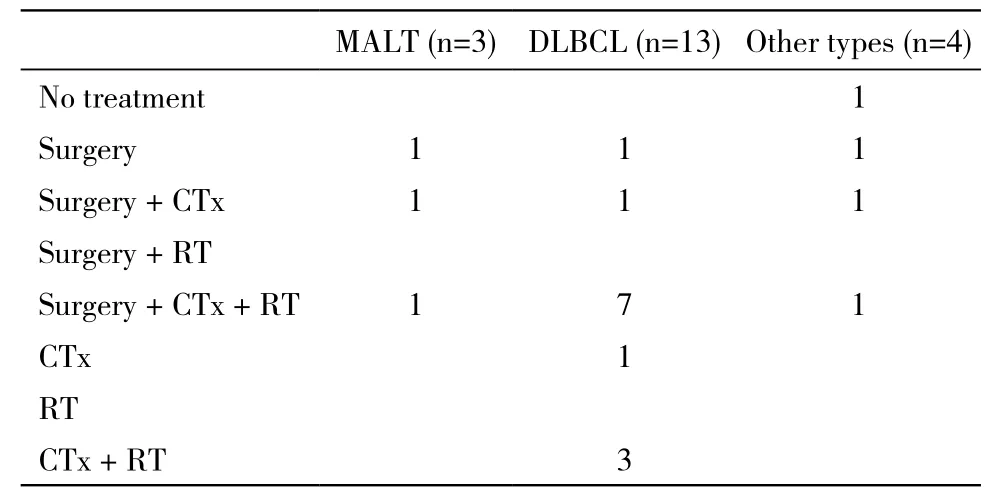
表2 20例原发性甲状腺淋巴瘤患者治疗情况Tab. 2 Treatment of 20 patients with primary thyroid lymphoma
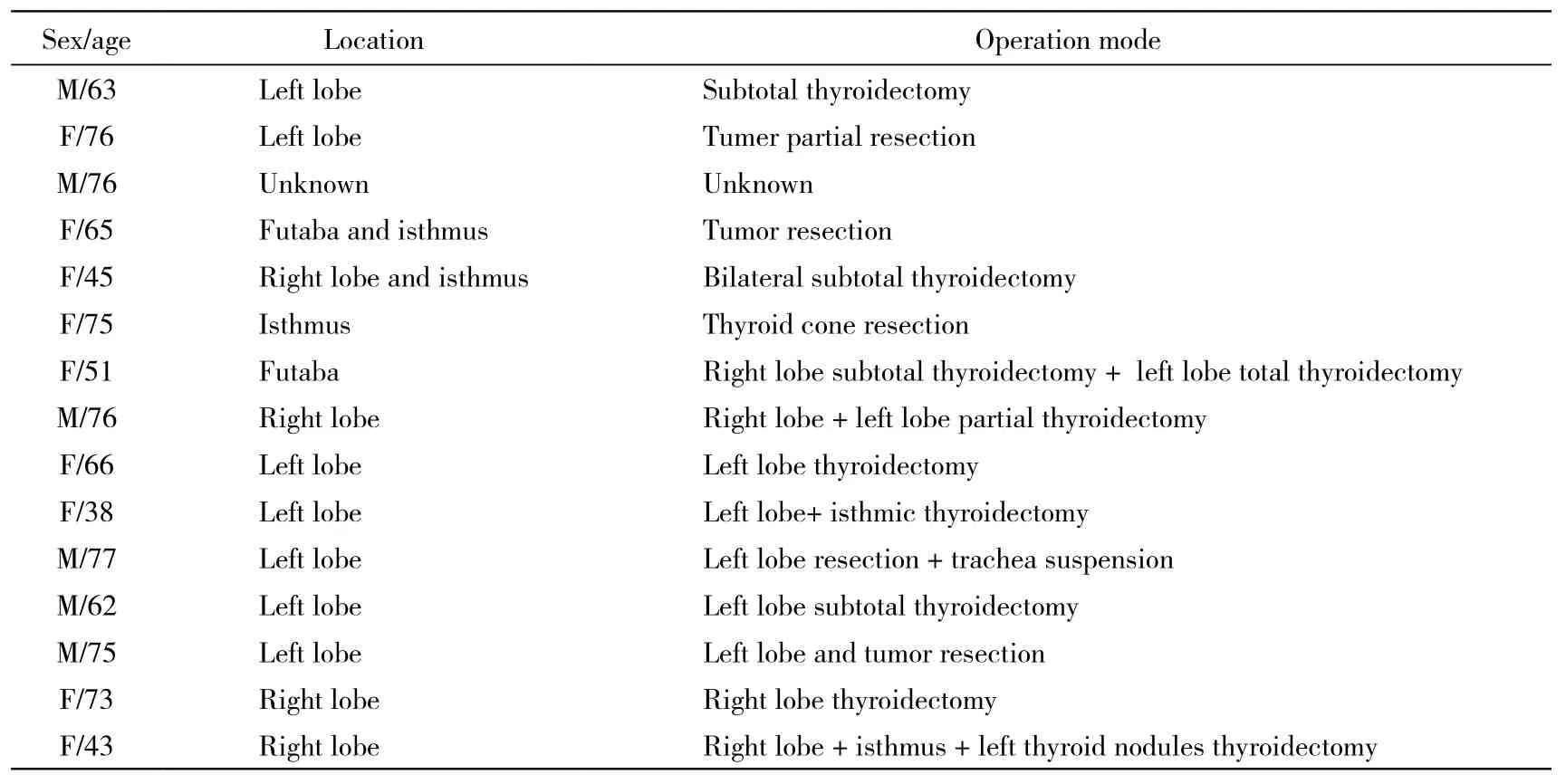
表3 15例原发性甲状腺淋巴瘤患者手术方式Tab. 3 Operative method of 15 patients with primary thyroid lymphoma

图 1 DLBCL型原发甲状腺淋巴瘤临床分期ⅠE期、ⅡE期患者生存曲线Fig. 1 Overall survival of DLBCL patients in stageⅠE or stageⅡE

图 2 DLBCL型原发甲状腺淋巴瘤手术组、未手术组生存曲线Fig. 2 Overall survival of DLBCL patients with or without surgery
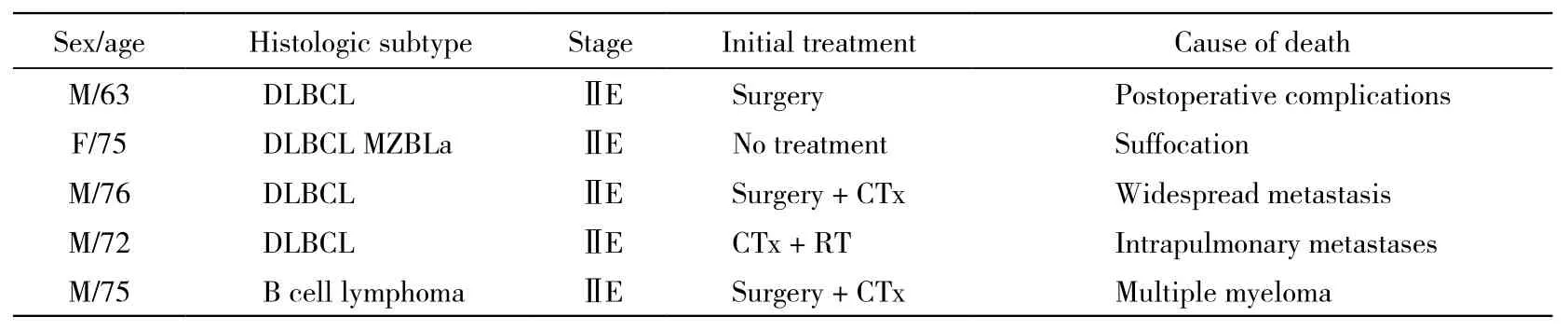
表4 5例治疗失败原发性甲状腺淋巴瘤患者情况Tab. 4 Details of 5 primary thyroid lymphoma patients with failure treatment
讨 论
原发性甲状腺淋巴瘤是一种少见疾病,本组资料的发病率较国外研究低[5-6],男女发病年龄无明显差异。因国内没有大样本的人口分布特征调查,故无法比较,患者常因突然增大的无痛甲状腺肿物就诊,其他症状包括呼吸困难、吞咽困难、肿物压迫造成的声音嘶哑,少数有呼吸困难及上腔静脉压迫梗阻。大多数病例都伴随着颈部淋巴结的肿大[12-13]。发热、盗汗、体质量减轻等症状较少发生[14]。大多数患者甲状腺功能正常[9,15]。大多数患者处于早期阶段(ⅠE和ⅡE期)。
原发性甲状腺淋巴瘤的发病机制仍不清楚,有学者认为,自身免疫性疾病引发的慢性抗原刺激导致慢性淋巴组织增生,进而出现变异、克隆增殖,最终发展为淋巴瘤,桥本甲状腺炎(Hashimoto′s thyroiditis,HT)为原发性甲状腺淋巴瘤的高危因素[1,7,16-17]。患桥本甲状腺炎的患者患PTL的风险增高40 ~ 80倍,通常被初诊为桥本甲状腺炎20 ~30年后发展为PTL[9,18-19]。尽管80% PTL患者患有桥本甲状腺炎,但只有0.6%的HT患者会发展为PTL[20]。本组资料50%患者伴发桥本甲状腺炎。
根据2004年WHO淋巴瘤分类,PTL可分为:1)非霍奇金淋巴瘤:包括弥漫性大B细胞淋巴瘤,结外边缘区B细胞淋巴瘤/低度恶性黏膜相关淋巴组织淋巴瘤(mucosa-associated lymphoma tissue,MALToma)、MZBL伴大细胞转化型/DLBCL和MZBL混合型淋巴瘤/高度恶性MALToma、滤泡性淋巴瘤(follicular lymphoma,FL)、髓外浆细胞瘤、外周NK/T细胞淋巴瘤;2)霍奇金淋巴瘤:根据恶性程度,可将PTLs进一步分为:①低度恶性组/惰性淋巴瘤,如MALT型MZBL、FL和髓外浆细胞瘤;②高度恶性组/侵袭性淋巴瘤,如MZBL伴大细胞转化型淋巴瘤和DLBCL。发生率最高的两种PTL的病理类型为DLBCL和MALToma,所占比例分别为70%和30%[8,21]。本组资料不同病理亚型的病例与国外研究相仿。
本组原发性甲状腺淋巴瘤的诊断方法:1)超声检查为鉴别甲状腺良恶性结节的首选影像学方法。但原发性甲状腺淋巴瘤发病率低,超声声像图改变特征不特异,容易出现误诊与漏诊。本组研究中,超声检查所示多为腺体双侧或单侧叶形态失常伴多发低回声结节、腺体双侧或单侧叶弥漫增大、低回声、不均质,建议穿刺活检,并未给出明确诊断导向。2)甲状腺CT,本组中仅有2例确诊前行甲状腺CT检查,且仅提示不除外恶性病变。3)细针穿刺细胞学是原发性甲状腺淋巴瘤初诊的重要方法,但其无法进行病理亚型分类,其准确性波动范围很大(25% ~ 90%)[14,22-23]。4)PET-CT检查可提高原发性甲状腺淋巴瘤诊断率,有效区分原发性甲状腺淋巴瘤与桥本甲状腺炎[24],然而高昂的费用限制了其应用,本组中,PET-CT仅用作患者接受治疗后病情进展或缓解的检查手段,其对复发病灶的敏感性高于CT[25]。5)组织活检是PTL组织学诊断的金标准[26],本组中,5例通过超声引导穿刺活检确诊,并通过免疫组化进行了详细分类;15例通过手术病理标本检测得到确诊。6)免疫组化是原发性甲状腺淋巴瘤诊断的重要手段,且可进一步明确恶性淋巴瘤的组织类型,利于术后指导放疗、化疗;本组中,5例组织穿刺活检均通过免疫组化得到确诊,15例手术中仅有5例术中冷冻提示淋巴瘤,所有病例均通过术后石蜡病理及免疫组化得到确诊。
由于本病少见,其治疗方式缺乏前瞻随机研究,现有研究参考其他结外淋巴瘤的治疗方式及效果,基于组织病理分型制订治疗方案[27-28]。像其他淋巴瘤一样,PTL对化疗和放疗敏感。DLBCL由于其具有侵袭性的病程特点,其治疗的标准模式是R-CHOP+放疗。结合文献[29],MALT淋巴瘤侵袭性弱,预后相对较好,适合单一方式治疗模式,可采用手术、放疗或二者联合。由于发病人数较少,缺乏治疗经验,本组2例MALT淋巴瘤均采用化疗,化疗方案为CHOP,但化疗周期数减少为2次。
对PTL的手术治疗仍存在争议,没有大型临床中心的数据。随着诊断技术的发展,外科手术在PTL诊断治疗的中应用正在逐渐减少[8,30]。本研究未发现手术组与未手术组总生存率存在显著差异,按病理亚型分类,DLBCL患者手术组与未手术组总生存率也未发现显著差异,但由于样本量较小,需要多中心大样本的研究支持。国外学者研究表明,原发性甲状腺淋巴瘤扩大的根治性手术联合放疗相对于手术活检联合放疗没有总生存率的优势(88% vs 85%)[31]。本组选择手术治疗的原因均为术前无明确诊断,术前经超声引导穿刺活检得到明确诊断的病例均转血液内科接受化疗。目前大多数学者认为,手术的作用主要是缓解压迫及明确诊断[32-34]。然而有研究对此提出了异议,气道梗阻患者可能通过使用糖皮质激素和化疗得到迅速缓解而无需外科手术干预。Myatt[35]报道了1例甲状腺淋巴瘤继发呼吸道梗阻,使用大剂量糖皮质激素后得到缓解的案例。另外临时气管支架结合放疗、化疗亦可作为外科手术干预的替代手段[36-39]。本组中1例因“发现颈前无痛性肿物4个月余,呼吸困难半个月”入院,经超声引导穿刺活检诊断为左叶甲状腺弥漫性大B细胞淋巴瘤,急诊行COP方案(环磷酰胺+长春地辛+甲泼尼龙)化疗,症状明显缓解,4 d后转血液科治疗,术后随访42个月无瘤生存。因此,PTL手术治疗的选择应慎重。
本组中,6例出现憋气症状(CT相示气管受压移位),1例入院后夜间因呼吸道梗阻窒息死亡。因此该疾病需加强患者的监护及呼吸道的管理,避免出现窒息。
对PTL的诊疗建议:对于因突然增大的无痛甲状腺肿物伴或不伴呼吸困难、吞咽困难、肿物压迫造成声音嘶哑的患者,应行超声检查。如超声显示腺体双侧或单侧叶弥漫增大、低回声、不均质或体双侧或单侧叶形态失常伴多发低回声结节,应行超声引导穿刺活检以明确诊断,如仍无法诊断可行外科手术干预明确诊断。由于慢性淋巴细胞性甲状腺炎的病例较普通人群PTL的发病率高40 ~ 80倍,因此对于这类甲状腺炎的病例,应积极处理其出现的甲状腺结节或甲状腺肿大。对于确诊患者应加强监护及呼吸道的管理,避免出现窒息。气道梗阻可试行使用糖皮质激素和化疗使其迅速缓解而无需外科手术干预,对于呼吸困难明显、气道受压梗阻严重者,必要时应行气管切开。明确诊断后根据病理类型选择相应治疗方案,DLBCL由于其具有侵袭性的病程特点,其治疗模式是多种手段联合,通常采用R-CHOP+放疗;MALT淋巴瘤适合单一方式治疗模式,可采用包括手术、放疗或二者联合,也可行短疗程化疗。外科手术干预应慎重选择。本病还需多中心临床研究,以满足对原发性甲状腺淋巴瘤研究的需要。
1 Derringer GA, Thompson LD, Frommelt RA, et al. Malignant lymphoma of the thyroid gland: a clinicopathologic study of 108 cases[J]. Am J Surg Pathol, 2000, 24(5): 623-639.
2 Belal AA, Allam A, Kandil A, et al. Primary thyroid lymphoma:a retrospective analysis of prognostic factors and treatment outcome for localized intermediate and high grade lymphoma[J]. Am J Clin Oncol, 2001, 24(3):299-305.
3 Kharrat S, Sethom A, Chelly I, et al. Primary thyroid lymphoma[J]. Semin Oncol, 2011, 89(7): 648-649.
4 Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas[J]. Cancer, 1972, 29(1):252-260.
5 Green LD, Mack L, Pasieka JL. Anaplastic thyroid cancer and primary thyroid lymphoma: a review of these rare thyroid malignancies[J]. J Surg Oncol, 2006, 94(8): 725-736.
6 Fujita A, Tomita N, Fujita H, et al. Features of primary extranodal lymphoma in Kanagawa, a human T-cell leukemia virus type 1 nonendemic area in Japan[J]. Med Oncol, 2009, 26(1): 49-54.
7 Ha CS, Shadle KM, Medeiros LJ, et al. Localized non-Hodgkin lymphoma involving the thyroid gland[J]. Cancer, 2001, 91(4):629-635.
8 Graff-Baker A, Roman SA, Thomas DC, et al. Prognosis of primary thyroid lymphoma: demographic, clinical, and pathologic predictors of survival in 1,408 cases[J]. Surgery, 2009, 146(6):1105-1115.
9 Pedersen RK, Pedersen NT. Primary non-Hodgkin’s lymphoma of the thyroid gland: a population based study[J]. Histopathology,1996, 28(1):25-32.
10 Austin JR, El-Naggar AK, Goepfert H. Thyroid cancers. II. Medullary, anaplastic, lymphoma, sarcoma, squamous cell[J]. Otolaryngol Clin North Am, 1996, 29(4):611-627.
11 Tupchong L, Hughes F, Harmer CL. Primary lymphoma of the thyroid: clinical features, prognostic factors, and results of treatment[J]. Int J Radiat Oncol Biol Phys, 1986, 12(10):1813-1821.
12 Sasai K, Yamabe H, Haga H, et al. Non-Hodgkin’s lymphoma of the thyroid. a clinical study of twenty-two cases[J]. Acta Oncol,1996, 35(4): 457-462.
13 Ruggiero FP, Frauenhoffer E, Stack BC Jr. Thyroid lymphoma: a single institution’s experience[J]. Otolaryngol Head Neck Surg,2005, 133(6):888-896.
14 Katna R, Shet T, Sengar M, et al. Clinicopathologic study and outcome analysis of thyroid lymphomas: experience from a tertiary cancer center[J]. Head Neck, 2013, 35(2): 165-171.
15 Thieblemont C, Mayer A, Dumontet C, et al. Primary thyroid lymphoma is a heterogeneous disease[J]. J Clin Endocrinol Metab,2002, 87(1):105-111.
16 Tsang RW, Gospodarowicz MK, Sutcliffe SB, et al. Non-Hodgkin’s lymphoma of the thyroid gland: prognostic factors and treatment outcome. The Princess Margaret Hospital Lymphoma Group[J]. Int J Radiat Oncol Biol Phys, 1993, 27(3):599-604.
17 Harrington KJ, Michalaki VJ, Vini L, et al. Management of non-Hodgkin’s lymphoma of the thyroid: the royal marsden hospital experience[J]. Br J Radiol, 2005, 78(929): 405-410.
18 Holm LE, Blomgren H, Löwhagen T. Cancer risks in patients with chronic lymphocytic thyroiditis[J]. N Engl J Med, 1985, 312(10):601-604.
19 Pasieka JL. Hashimoto’s disease and thyroid lymphoma: role of the surgeon[J]. World J Surg, 2000, 24(8):966-970.
20 Watanabe N, Noh JY, Narimatsu H, et al. Clinicopathological features of 171 cases of primary thyroid lymphoma: a long-term study involving 24553 patients with Hashimoto’s disease[J]. Br J Haematol, 2011, 153(2): 236-243.
21 Rawal A, Finn WG, Schnitzer B, et al. Site-specific morphologic differences in extranodal marginal zone B-cell lymphomas[J]. Arch Pathol Lab Med, 2007, 131(11):1673-1678.
22 Gupta N, Nijhawan R, Srinivasan R, et al. Fine needle aspiration cytology of primary thyroid lymphoma: a report of ten cases[J]. Cytojournal, 2005, 2:21.
23 Nguyen GK, Lee MW, Ginsberg J, et al. Fine-needle aspiration of the thyroid: an overview[J]. Cytojournal, 2005, 2(1):12.
24 Nakadate M, Yoshida K, Ishii A, et al. Is 18F-FDG PET/CT useful for distinguishing between primary thyroid lymphoma and chronic thyroiditis?[J]. Clin Nucl Med, 2013, 38(9): 709-714.
25 Baba S, Abe K, Isoda T, et al. Impact of FDG-PET/CT in the management of lymphoma[J]. Ann Nucl Med, 2011, 25(10):701-716.
26 Takano T, Asah S, Matsuzuka F, et al. Aspiration biopsy-nucleic acid diagnosis of thyroid malignant lymphoma by vectorette PCR:Experience of eight cases[J]. Leuk Res,2008,32(1): 151-154.
27 Alzouebi M, Goepel JR, Horsman JM, et al. Primary thyroid lymphoma: the 40 year experience of a UK lymphoma treatment centre[J]. Int J Oncol, 2012, 40(6): 2075-2080.
28 Onal C, Li YX, Miller RC, et al. Treatment results and prognostic factors in primary thyroid lymphoma patients: a rare cancer network study[J]. Ann Oncol, 2011, 22(1):156-164.
29 Cha H, Kim JW, Suh CO, et al. Patterns of care and treatment outcomes for primary thyroid lymphoma: a single institution study[J]. Radiat Oncol J, 2013, 31(4):177-184.
30 Meyer-Rochow GY, Sywak MS, Reeve TS, et al. Surgical trends in the management of thyroid lymphoma[J]. Eur J Surg Oncol, 2008,34(5):576-580.
31 Pyke CM, Grant CS, Habermann TM, et al. Non-Hodgkin’s lymphoma of the thyroid: is more than biopsy necessary?[J]. World J Surg, 1992, 16(4): 604-609.
32 Motta G, Cea M, Carbone F, et al. Current standards and future strategies in immunochemotherapy of non-Hodgkin’s lymphoma[J]. J BUON, 2011, 16(1):9-15.
33 Kaneko S, Yamaguchi N. Epidemiological analysis of site relationships of synchronous and metachronous multiple primary cancers in the National Cancer Center, Japan, 1962-1996[J]. Jpn J Clin Oncol, 1999, 29(2): 96-105.
34 Sippel RS, Gauger PG, Angelos P, et al. Palliative thyroidectomy for malignant lymphoma of the thyroid[J]. Ann Surg Oncol, 2002, 9(9):907-911.
35 Myatt HM. Acute airway obstruction due to primary thyroid lymphoma[J]. Rev Laryngol Otol Rhinol (Bord), 1996, 117(3):237-239.
36 Hopkins C, Stearns M, Watkinson AF. Palliative tracheal stenting in invasive papillary thyroid carcinoma[J]. J Laryngol Otol, 2001,115(11):935-937.
37 Noppen M, Poppe K, D’Haese J, et al. Interventional bronchoscopy for treatment of tracheal obstruction secondary to benign or malignant thyroid disease[J]. Chest, 2004, 125(2):723-730.
38 Tsutsui H, Kubota M, Yamada M, et al. Airway stenting for the treatment of laryngotracheal stenosis secondary to thyroid cancer[J]. Respirology, 2008, 13(5): 632-638.
39 Lee J, Won JH, Kim HC, et al. Emergency dilation by selfexpandable tracheal stent for upper airway obstruction in a patient with a giant primary thyroid lymphoma[J]. Thyroid, 2009, 19(2):193-195.
Primary thyroid lymphoma: A clinical analysis of 20 cases
ZHANG Bingdong1, XUE Yonggan1, LIU Hongyi2, WANG Baishi2, JIA Baoqing21
Chinese PLA Medical School, Beijing 100853, China;2Department of Surgical Oncology, Chinese PLA General Hospital, Beijing 100853, China
JIA Baoqing. Email: baoqingjia@126.com
ObjectiveTo analyze the clinical presentation, pathological type, diagnosis, treatment and prognosis of primary thyroid lymphoma (PTL).MethodsClinical data about 20 cases with primary thyroid lymphoma admitted to Chinese PLA General Hospital from June 1993 to June 2013, including clinical manifestation, diagnosis procedure, treatment project and prognosis, were reviewed. According to the stage of primary thyroid lymphoma and whether accepted operation, patients with different pathological types were divided into different groups and their overall survival was analyzed.ResultsOne case died of suffocation without treatment, 5 cases underwent chemotherapy or chemotherapy + radiotherapy after ultrasound guided puncture biopsy for diagnosis, 14 cases underwent operation, operation + chemotherapy or operation + chemotherapy + radiotherapy. The median follow-up time of all patients was 41 months (0 - 131 months), but the follow-up had not reached the end yet. Three MALT patients got long-term survival. The 2-year and 5-year survival rates ofⅠE stage DLBCL were 100% (5 cases) and 100% (5 cases) respectively. The 2-year and 5-year survival rates of ⅡE stage DLBCL were 72.9% (6 cases) and 58.3% (5 cases) respectively. The prognosis of DLBCL patients with stage ⅠE was better than ⅡE (P=0.048). The 2-year and 5-year survival rates of DLBCL patients underwent surgery were 74.1% (7 cases) and 74.1% (7 cases) respectively. The 2-year and 5-year survival rates of DLBCL patients without surgery were 100% (4 cases) and 75.0% (3 cases), which showed no significant difference between two groups (P=0.804).ConclusionMALT patients with treatment can get a long-term survival. The prognosis of stage ⅠE patients with DLBCL is better than that of stage ⅡE patients. Operation has no significant effect on the prognosis of patients with DLBCL. Surgical operation intervention should be chosen carefully.
thyroid neoplasms; lymphoma; surgical procedures, operative
R 543
A
2095-5227(2015)05-0419-06
10.3969/j.issn.2095-5227.2015.05.004
时间:2015-03-03 09:48
http://www.cnki.net/kcms/detail/11.3275.R.20150303.0948.001.html
2014-12-02
国家自然科学基金项目(81171901)
Supported by the National Natural Science Foundation of China(81171901)
张秉栋,男,在读硕士。研究方向 :胃肠肿瘤的外科治疗。Email: 513045961@qq.com
贾宝庆,男,博士,主任医师,硕士生导师。Email: bao qingjia@126.com

