Randomized controlled trial of adjunctive EEG-biofeedback treatment of obsessive-compulsive disorder
Xiaopeng DENG, Gaohua WANG*, Lifang ZHOU, Xinfeng ZHANG, Mei YANG, Gangya HAN,Zheming TU, Bo LIU
•Original article•
Randomized controlled trial of adjunctive EEG-biofeedback treatment of obsessive-compulsive disorder
Xiaopeng DENG1, Gaohua WANG1*, Lifang ZHOU2, Xinfeng ZHANG2, Mei YANG2, Gangya HAN2,Zheming TU2, Bo LIU2
Obsessive compulsive disorder; EEG biofeedback; cognitive function, China
1. Background
Obsessive-compulsive disorder (OCD) is a mental illness characterized by obsessive thoughts and (or) compulsive behaviors. Wide variations in the clinical presentations of OCD complicate the treatment of the condition and can result in a chronic course and poor prognosis.There are several treatment strategies for OCD, most of which combine medications with psychotherapy,but the clinical outcomes are often unsatisfactory.[1]Electroencephalograph (EEG) biofeedback is an adjunctive treatment to medications and psychotherapy that has proven beneficial in the treatment of panic disorders and other conditions.[2]It uses real-time EEG to promote desired brain activities and to suppress undesired brain activities. In this study, we tested the effectiveness of EEG biofeedback as an adjunctive treatment for cognitive-behavioral psychotherapy and medication in the treatment of OCD.
2. Methods
2.1 Sample
The enrollment process for the study is shown in Figure 1. Potential participants were outpatients and inpatients seeking treatment at the Jingzhou Mental Health Center from May to December 2013 who met the following inclusion criteria∶ (a) 18 to 45 years of age; (b) junior high school education or above; (c) right-handed; (d) both the patient and the patient’s guardian provided written informed consent to participate in the study; (e) met the International Classification of Diseases, 10thedition(ICD-10)[3]diagnostic criteria for obsessive-compulsive disorder based on a clinical examination conducted by an attending-level psychiatrist and confirmed by the department head; (f) had a score of ≥18 on the Yale-Brown Obsessive Compulsive Scale (YBOCS)[4]; and (g)had not taken any psychiatric medication in the two weeks prior to enrollment. The patients were excluded if they met any of the following exclusion criteria∶ (a) had a history of diabetes, high blood pressure, heart disease,diseases of the nervous system, substance dependence,schizophrenia, major depression, or other mental illnesses; (b) pregnant, breast feeding or planning to get pregnant; (c) experienced a recent physical trauma,surgery or acute or chronic infection; (d) color blind; or(e) serious suicidal ideation or behavior.
After obtaining informed consent, 79 patients were randomized (using a random number table) into the study group (n=40) or the control group (n=39). There were 21 males and 19 females in the study group; 25(62.5%) were inpatients; their range of age was 18 to 43 with a mean (sd) age of 26.7(8.2) years; their duration of disease was 0.5 to 13 years (mean [sd]= 3.8 [3.7] years,median=2.0 years); their mean (sd) age of onset was 22.9 (5.0) years. There were 20 males and 19 females in the control group; 23 (58.9%) were inpatients; their range of age was 19 to 42 with a mean (sd) age of 26.6(7.8) years; the duration of disease was 0.6 to 12 years(mean [sd]= 3.7 [3.4] years, median=3.0 years); their mean (sd) age of onset was 23.0 (4.9) years. There were no statistically significant differences between the groups in gender, proportion of inpatients, age, duration of illness, or age of onset of illness.
2.2 Intervention
Before the treatment began, patients who were taking medications at the time of enrollment underwent a two-week ‘wash-out’ period. Among the 40 study group participants, 11 (27.5%) needed to participate in the 2-week washout phase, and among the 39 controlgroup participants, 9 (23.1%) required a washout period(χ2=0.15,p=0.698).
During the following eight weeks, patients in both groups took sertraline 50 to 200mg/d. Among the 37 participants in the study group who completed the study the mean (sd) dose was 168 (29) mg/d; among the 35 in the control group who completed the study the mean (sd) dose was 171 (30) mg/d. Patients did not take any other psychiatric medication during the 8-week trial.
The Biofeedback System Infinity 4000C, provided by Nanjing Vish Medical Technology Company, was used to treat the patients in the study group five times a week for eight weeks (a total of 40 times). Each session lasted 24 minutes. During the first session an operator explained the apparatus to the patient but after that patients had little contact with the operators (unless something unexpected occurred). At each session after being attached to the apparatus patients were given guided practice to help them master the techniques of relaxing and concentrating while observing their brainwaves. Based on the operation manual, patients were trained to increase specific types of brainwaves∶ α,sensorimotor rhythm (SMR), and θ brainwaves.[6,7]
2.3 Assessments
OCD symptoms were assessed using the YBOCS[4]at baseline and at the end of the 2nd, 4th, 6th, and 8thweek of treatment. Patients’ cognitive functioning,was assessed using the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS)[8]before the treatment and at the end of the 8thweek of treatment. Both the YBOCS and RBANS assessments were conducted by a psychiatrist with extensive experience in using the scales (from other research studies) who was blind to the group assignment of all patients.
YBOCS is the most widely used assessment scale for OCD. The Chinese version of the YBOCS is reliable and valid and has been widely used in clinical studies and research.[4]The instrument has two parts - a symptom checklist and a symptom severity measure. In the current study we only used the 10-item symptoms severity measure; the first five items assess the severity of obsessive thoughts and the second five items assess the severity of compulsive behaviors. Items are rated on a 0 to 4 Likert scale, thus the total score ranges from 0 to 40 and the two subscale scores range from 0 to 20,with higher scores representing more severe symptoms.In this study we define ‘improvement’ as a reduction of at least 50% in the baseline total YBOCS score.[9]
A previous study has found that the Chinese version of the RBANS is reliable and valid.[8,10]The battery includes 12 individual cognitive tasks assessing 5 cognitive domains∶ immediate memory/learning, visual spatial ability, language, attention, and delayed memory.[11,12]The sum of the 5 domain scores are combined into a total RBANS score, which provides an overall assessment of cognitive functioning.
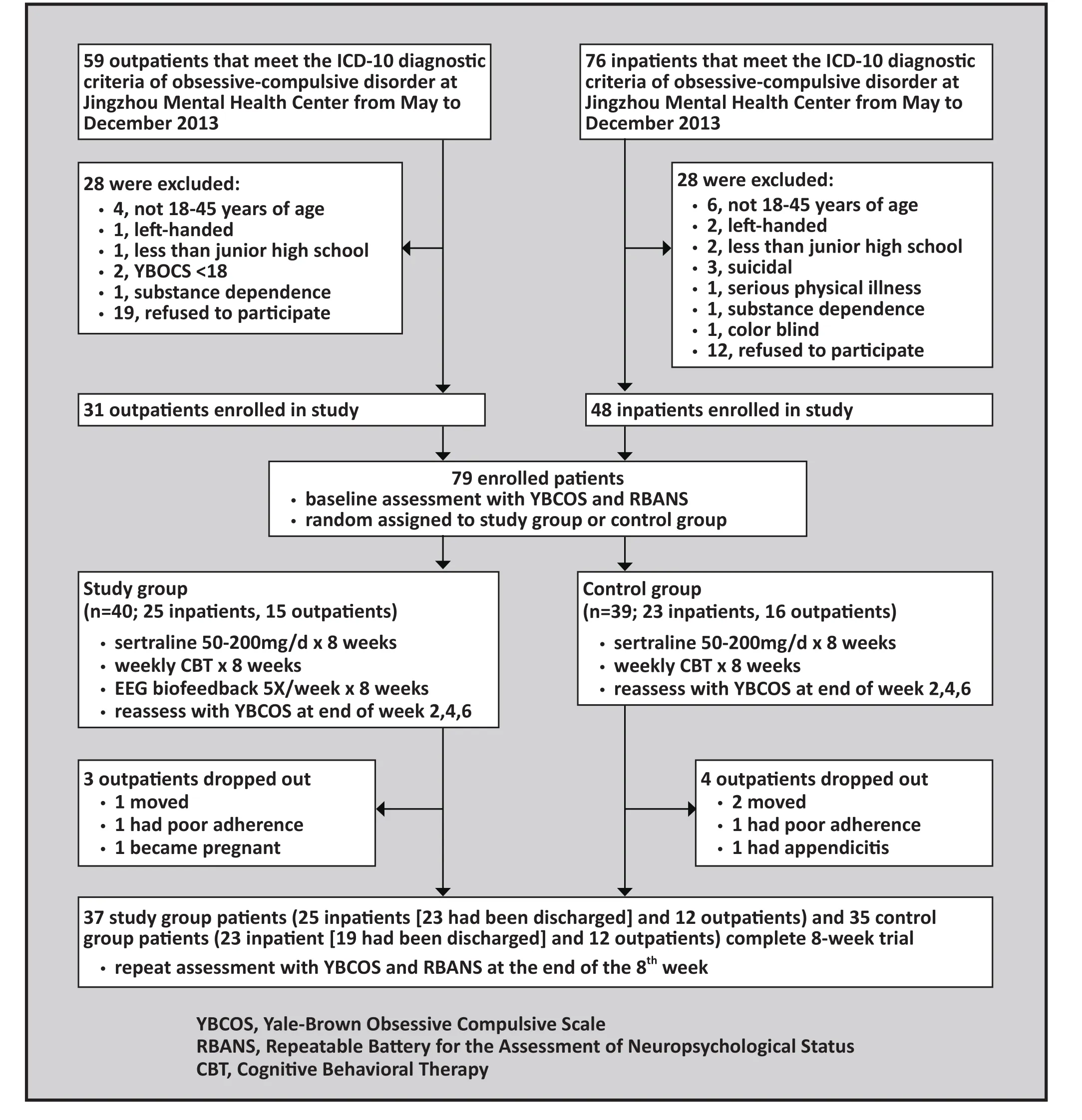
Figure 1. Flowchart for the study
2.4 Dropout criteria
Patients were considered dropouts if∶ (a) they did not comply with the treatment regimen after enrollment;(b) they stopped the treatment due to serious adverse events, serious complications or special physiological changes; (c) they had to stop treatment due to physical diseases during the study; (d) their symptoms worsened and a change of treatment plan was needed; or (e) they dropped out voluntarily.
2.5 Statistical methods
Data were double entered and analyzed using SPSS19.0.Continuous variables were analyzed using the repeated measures analysis of variance. Categorical variables were analyzed using chi-square tests. Correlations were estimated using the Pearson correlation coefficients.Significance level was set at 0.05 for all tests. All tests were two-tailed tests. The analytical sample consisted of all participants who completed the entire 8 weeks of treatment.
3. Results
Based on the subscale ratings of the YBOCS at baseline,participants were subclassified as ‘obsessive thought type’ (obsessive thought subscale score >5, compulsive behavior subscale score <5, and all compulsive item scores <2), ‘compulsive behavior type’ (compulsive behavior subscale score >5, obsessive thought subscale score ≤5, and all obsessive item scores <2), or ‘mixed type’ (obsessive thoughts and compulsive behavior subscale scores both >5). The study group included 13 patients classified as obsessive thought type, 3 as compulsive behavior type, and 24 as mixed type;the control group included 12 patients classified as obsessive thought type, 4 as compulsive behavior type,and 23 as mixed type. The proportions of the three subtypes were not significantly different between the two groups (χ2=0.19,df=2, p=0.909).
3.1 Completion of the trial and participation in the intervention
As shown in Figure 1, 72 of the 79 enrolled participants(91%) completed the 8-week trial. All 7 dropouts were participants who had been enrolled as outpatients.Three of the 40 participants (7.5%) in the study group and 4 of the 39 participants (10.3%) in the control group dropped out; the dropout rate was not significantly different between the two groups (χ2=0.19,p=0.666).Among the 48 participants who were inpatients at thetime of enrollment - all of whom completed the study- 44 (91.7%) had been discharged and were being followed-up as outpatients at the time of the 8-week assessment.
Attendance at the CBT group sessions was similar in the two groups∶ The 37 study-group patients and 35 control-group patients who completed the study attended a mean (sd) of 7.92 (0.27) and 7.80 (0.41)of the 8 CBT groups sessions, respectively (t=1.45,p=0.149).
In the study group, participation in the biofeedback sessions was also quite high∶ 24 of the 37 who completed the study attended all 40 sessions, 9 attended 39 sessions, 1 attended 38 sessions, 1 attended 37 sessions,and 2 attended 36 sessions. Thus the overall attendance rate at the biofeedback sessions was 98.5%.
3.2 Comparison of the YBOCS scores in the two groups
As shown in Table 1, there was no difference in the YBOCS scores between the two groups at baseline(p=0.975). There was robust time main effect(F=2239.64,p<0.001) indicating that the YBOCS scores dropped over time. The overall group main effect was non-significant (F=2.30,p=0.314), but a group by time interaction was found (F=5.48,p=0.001). Therefore,post-hoc comparisons were carried out. At each followup (i.e., the end of the 2nd, 4th, 6th, and 8thweeks), the YBOCS scores dropped in both groups (p<0.01). But by the end of the 6thand 8thweeks, the drop in the study group was significantly greater than the drop in the control group (p=0.008 and 0.003, respectively).
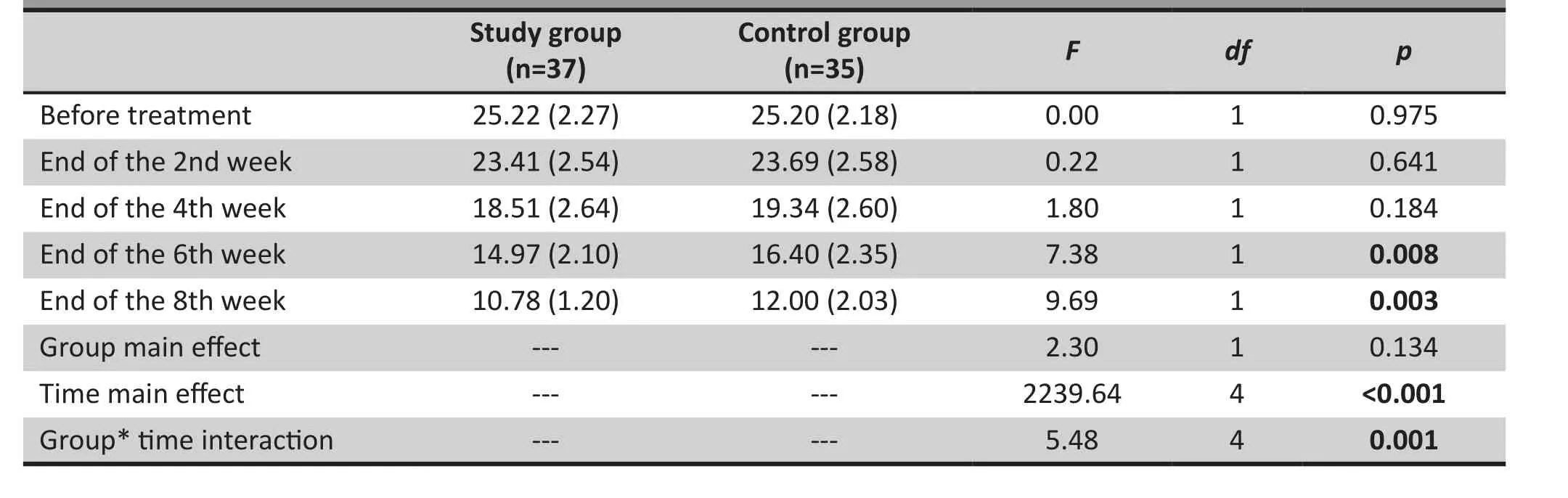
Table 1. Repeated measures analysis of variance comparison of the mean (sd) YBOCS total scores between the two groups before and atfer treatment
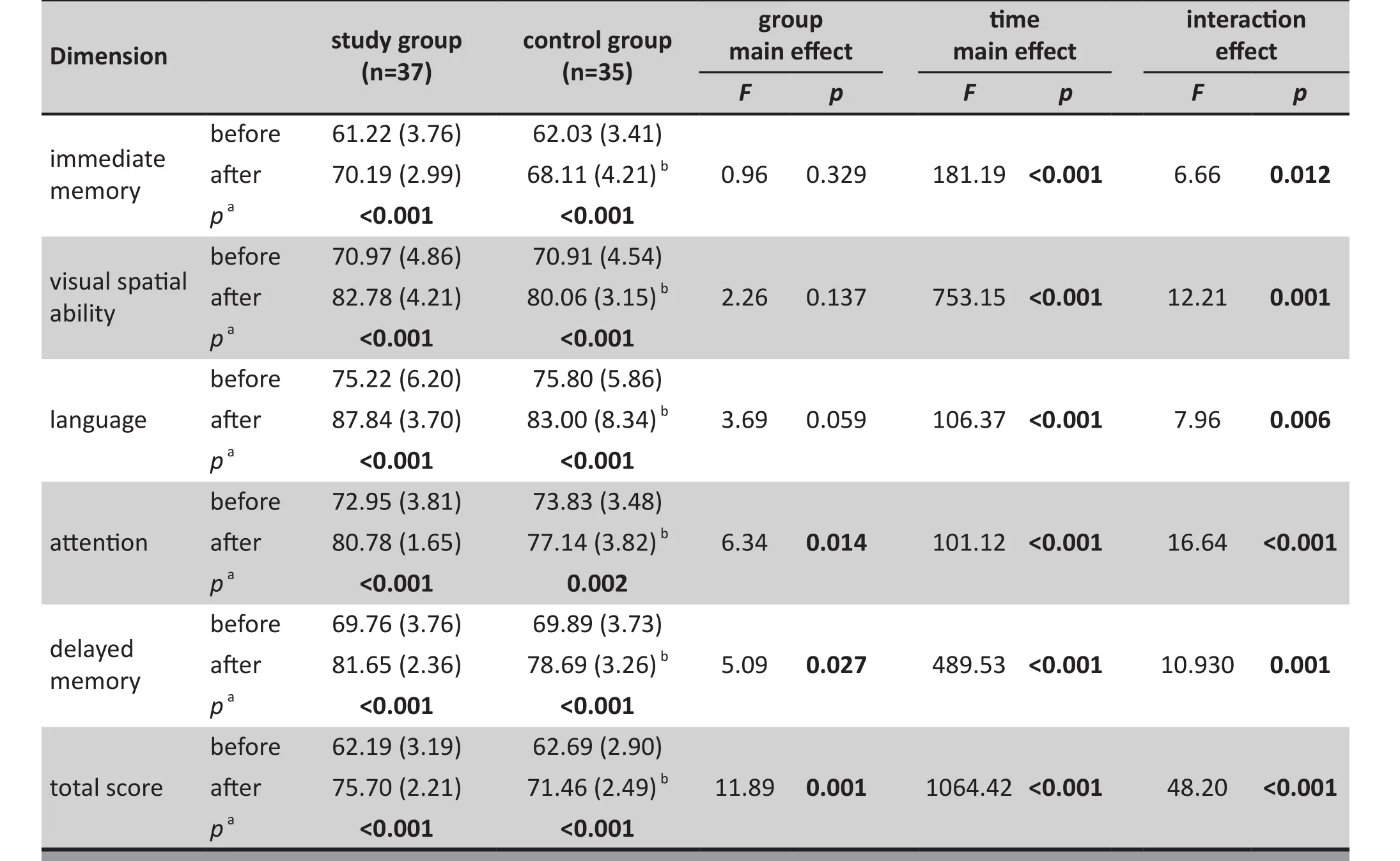
Table 2. Comparison of the five dimension scores and total score of the RBANS between the two groups before and atfer treatment (mean [sd])
3.3 Comparison of the treatment effects between the two groups
Based on the criteria of a 50% drop from the baseline YBOCS score, at the end of the 8-week trial the treatment was effective in 32 of the 37 (86.5%)participants in the study group who completed the trial and in 22 of the 35 (62.9%) participants in the control group who completed the trial. The difference in effectiveness between the two groups was statistically significant (χ2=5.36,p=0.021).
3.4 Comparison of the RBANS scores of the two groups before and atfer the treatment
As shown in Table 2, after 8 weeks of treatment, the group main effect was not statistically significant for three of the RBANS domains (immediate memory, visual spatial memory, and language) but it was statistically significant for the total RBANS scores and for the dimensions scores for attention and delayed memory.The time main effect and the group by time interactions were statistically significant for all five RBANS domains and for the total RBANS score. Post-hoc comparisons indicated statistically significant between-group differences in all five domains and in the total score;the improvement in scores for the study group were all greater than those for the control group.
3.5 Correlation analysis of the improvement of symptoms and cognitive functions of the two groups
At the end of 8thweek, changes in the YBOCS score were significantly correlated with changes in the RBANS total score in the study group (r=0.433,p=0.007) but this correlation was much weaker (and non-significant) in the control group (r=0.17,p=0.327).
4. Discussion
4.1 Main findings
This randomized controlled trial with a blind evaluation of the outcome provided clear evidence that adjunctive treatment with EEG biofeedback can improve the treatment effect of standard treatment with medication and psychotherapy for OCD. Over an 8-week treatment trial the greater improvement in OCD symptoms in the group that had adjunctive treatment with biofeedback became statistically significant by the end of the 6thweek. We also found that patients who received adjunctive treatment with EEG-based biofeedback show significantly greater improvement in cognitive functioning after 8 weeks of treatment, an improvement that was strongly correlated with the improvement in OCD symptoms.
These findings are consistent with previous reports by both Western[13]and Chinese[14]researchers who also find that EEG biofeedback is effective in improving the symptoms of OCD. Patients with OCD have elevated levels of anxiety, which can induce psychological and physical changes such as tension, changes in brain waves, and elevated heart rate and blood pressure.EEG biofeedback is a technique that helps individuals understand these physical changes (which they are usually not aware of before the training). It also helps them learn how to regulate these psychological and physical changes. As they master these relaxation skills there is a corresponding improvement in the symptoms of OCD. However, the etiology of OCD remains unclear,[15]so further research will be needed to clarify the exact mechanisms via which biofeedback augments the treatment effects of medication and psychotherapy.
Cognitive functioning is closely associated with the clinical presentation of OCD and with the shortterm and long-term prognosis for OCD.[16,17]Despite recent increased research interest in the cognitive functioning of individuals with OCD, few studies have assessed the effects of biofeedback on cognitive functioning in OCD patients. One exception is a study by Liu and colleagues[18]who reported that providing EEG biofeedback training to patients with OCD can improve their cognitive functioning as assessed by the Cancellation Test, the Clinical Memory Scale, and the Wisconsin Card Sorting Test.[19,20]In the current study we expanded on these results; our use of the RBANS,a multi-dimensional assessment tool of cognitive functioning, provided evidence about the benefit of biofeedback in OCD for two additional cognitive domains not considered in previous studies - visual spatial ability and language. Furthermore, we also found that the improvement in cognitive function associated with EEG biofeedback was closely correlated with improvement in OCD symptoms.
4.2 Limitations
Several limitations should be borne in mind when interpreting findings from this study. First, there was no placebo control of the EEG biofeedback therapy (e.g.,mock EEG training) so it is possible that the improved OCD symptoms and cognitive functioning was due to the ‘placebo effect’ of the 40 additional contacts with clinicians individuals in the study group experienced over the 8-week trial (i.e., unrelated to the EEG biofeedback training). Second, the two-week ‘washout’period for patients who were being medicated at the time of enrollment in the study may have aggravated OCD symptoms and cognitive dysfunction due to withdrawal from medications, though this potential effect would have been similar in the two groups. Third,the small sample size precluded stratified analysis by types of OCD or other factors. Fourth, the inclusion of both inpatients and outpatients in the study and the change of some participants from inpatient to outpatient status during the study (i.e., differences in the settings in which they are living and being evaluated in) was a confounding variable that was not adequately controlled for. Fifth, it would have been better to conduct an ‘intention to treat’ analysis by carrying the final results of the 7 dropout patients forward,but, given the small number of dropouts, this would not significantly affect the overall findings. And finally,due to the lack of Chinese norms, we cannot compare the RBANS cognitive functioning scores of the OCD participants to those of the general Chinese population.Future studies are needed to address these issues and to determine whether the short-term benefits of biofeedback training persist over the long-term, after the training has stopped.
4.3 Implications
This study had a reasonably sized sample (n=79), and used a randomized controlled design, a blind evaluation of outcome, and standardized assessment measures.Given the methodological strength of the study, the unequivocal result that 8 weeks of adjunctive treatment with EEG biofeedback enhances the improvement in OCD symptoms and cognitive functioning of OCD patients being treated with medication and psychotherapy is quite robust. But the intervention is quite intensive - requiring daily sessions for the patients- so additional work is needed to determine whether or not the benefit persists after stopping the training sessions and, if not, the frequency of booster sessions that are needed to maintain the beneficial effects.
Funding
This study was supported by the Jingzhou Science and Technology Development Plan (Grant No. 2013AE39).
Conflict of interest
The authors report no conflict of interest related to this manuscript.
Ethical review
The study was approved by the research review committee of the Jingzhou Mental Health Center.
Informed consent
Written informed consent was obtained from all participants and their family members.
1. Wang XM, Xiao ZP. [The treatment and progress of OCD].Zhonghua Xing Wei Yi Xue Yu Nao Ke Xue Za Zhi. 2009; 18(11)∶1054-1056. Chinese. doi∶ http∶//doi.med.wanfangdata.com.cn/10.3760/cma.j.issn.1674-6554.2009.11.036
2. Zhen YP. [Clinical Practice of Biofeedback]. Beijing∶ Higher Education Press. 2003; 15-30. Chinese
3. Fan XD (translation). [ICD-10 Classification of Mental and Behavioral Disorders, Clinical Descriptions and Diagnostic Criteria]. Beijing∶ People’s Health Publishing House. 1993;pp∶ 116-118. Chinese
4. Xu Y, Zhang HY. [The reliability and validy of the Chinese version of Yale-Brown obsessive-compulsive scale].Shanghai Arch Psychiatry.2006; 18(6)∶ 321-323. Chinese. doi∶ http∶//dx.doi.org/10.3969/j.issn.1002-0829.2006.06.001
5. Jiao QY, Wang BL, Kong LL, Wang WF. [Analysis of Duloxetine combined cognitive behavioral therapy in patients with somatoform disorders].Jing Shen Yi Xue Za Zhi. 2003;26(3)∶ 169. Chinese. doi∶ http∶//dx.doi.org/10.3969/j.issn.1009-7201.2013.03.003
6. Feng YK. [Clinical Electroencephalography]. Beijing∶ People’s Health Publishing House. 1980; 11-19. Chinese
7. Li O, Feng XM, Zhou ZQ, Guo ZX, Wang C. [Clinical studies of biofeedback therapy on anxiety disorder after brain stroke].Zhongguo Liao Yang Yi Xue. 2012; 21(3)∶ 252-253. Chinese.
8. Zhang BH, Tan YL, Zhang WF, Eang ZR, Yang GG, Shi C, et al. [Repeatable battery for the assessment of neuropsychological status as a screening test in Chinese].Zhongguo Xin Li Wei Sheng Za Zhi. 2008; 22(12)∶866-867. Chinese. doi∶ http∶//dx.doi.org/10.3321/j.issn∶1000-6729.2008.12.001
9. Wang ZS, Cui MH, Song XL, Lin XY. [Curative effect analysis of comprehensive psychotherapy in the treatment of refractory obsessive compulsive disorder].Bingzhou Yi Xue Yuan Xue Bao. 2014; 2(37)∶ 19-20. Chinese
10. Wang JH, Li CB, Cheng Y, Yi ZH, Long B, Wang JJ.[Reliability and validity of repeatable battery for the assessment of neuropsychological status (RBANS)].Shanghai Arch Psychiatry. 2009; 21(5)∶ 265-268. Chinese.doi∶ http∶//doi.med.wanfangdata.com.cn/10.3969/j.issn.1002-0829.2009.05.003
11. Zhou CY, Sha WW, Zhang XB, Geng DQ, Dong XX, Fang CL.[Evaluation of cognitive functions and its influencing factors in refractory obsessive-compulsive disorder].Lin Chuang Jing Shen Yi Xue Za Zhi. 2011; 21(6)∶ 391. Chinese
12. Zhao J, Hu WH, Zhu F, Long B, Wang JJ, Yi ZH. [A comparative study of the effect of rTMS on cognitive function in patients with chronic schizophrenia].Jing Shen Yi Xue. 2013; 26(2)∶104. Chinese
13. Lazarov A, Dar R, Oded Y. Are obsessive compulsive tendencies related to reliance on external proxies for internal states Evidence from biofeedback-aided relaxation studies.Behav Res Ther. 2010; 48∶ 516-523. doi∶ http∶//dx.doi.org/10.1016/j.brat.2010.02.007
14. Ye C, An CX, Wang XY. [Impact of the biofeedback technology on OCD psychological and physiological parameters].Zhongguo Jian Kang Xin Li Xue Za Zhi. 2010; 18(5)∶ 513-515.Chinese
15. Cai HD. [OCD brain dysfunction].Xin Li Ke Xue Jin Zhan. 2006;14(3)∶ 401-407. Chinese
16. Mantella RC, Butters MA, Dew MA, Mulsant BH, Begley A,Tracey B, et al. Cognitive impairment in late-life generalized anxiety disorder.Am J Geriatr Psychiatry. 2007; 15(8)∶673-679. doi∶ http∶//dx.doi.org/10.1097/JGP.0b013e31803111f2
17. Addington J, Girard TA, Christeneen BK, Addington D. Social cognition mediates illness related and cognitive influences social function in patients with schizophrenia·spectrum disorders.J Psychiatry Neurosci. 2010; 35(1)∶ 49-54. doi∶http∶//dx.doi.org/10.1503/jpn.080039
18. Liu GJ, Chen XS, Chen MY. [The study of eeg biofeedback treatment improving cognitive function in obsessive compulsive disorder].Xian Dai Zhen Duan Yu Zhi Liao. 2012;23(1)∶ 15-16. Chinese. doi∶ http∶//doi.med.wanfangdata.com.cn/10.3969/j.issn.1001-8174.2012.01.006
19. Zhou YF, Zhang YL, Hu JZ, Liu M, Zhao XF, Li HZ. [A preliminary study of cognitive dysfunction in obsessivecompulsive disorder].Zhongguo Lin Chuang Xin Li Xue Za Zhi.2005; 13(3)∶ 337-339. Chinese. doi∶ http∶//doi.med.wanfangdata.com.cn/10.3969/j.issn.1005-3611.2005.03.029
20. Zhang JR, Liu M, Liang HX. [A study of cognitive feature in first-episode patients with obsessive-compulsive disorder].Jing Shen Yi Xie Za Zhi. 2009; 22(2)∶ 98-99.Chinese. doi∶ http∶//doi.med.wanfangdata.com.cn/10.3969/j.issn.1009-7201.2009.02.006
(received∶ 2014-05-19; accepted∶ 2014-07-07)

Xiaopeng Deng graduated from China Three Gorges University, in Hubei in 2003. He is currently pursuing his Master’s degree at Wuhan University. He is an attending psychiatrist at Hubei Jingzhou Mental Health Center and Director of the Medical department. He is interested in biological psychiatry and social psychiatry.
脑电生物反馈辅助治疗强迫症的随机对照试验
邓小鹏,王高华,周丽芳,张新风,杨媚,韩刚亚,涂哲明,刘波
∶强迫症;脑电生物反馈;认知功能;中国
Background:Current interventions for obsessive-compulsive disorder (OCD) are often of limited benefit.Aim:To evaluate the effect of adjunctive treatment with EEG biofeedback training on the symptoms and cognitive functioning of individuals with OCD.Methods:A total of 79 individuals with OCD were randomly assigned to the study group (n=40) or the control group (n=39). The control group was treated using a combination of sertraline (50 to 200 mg/d)and weekly cognitive behavioral therapy sessions by trained therapists for 8 weeks; the study group was treated using the same regimen plus EEG biofeedback sessions 5 times per week. The Yale Brown Obsessive Compulsive Scale (YBOCS) was administered by a psychiatrist who was blind to patients’ treatment status before treatment and at the end of the 2nd, 4th, 6thand 8thweek for treatment; the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) was administered before and after the 8-week trial.Results:Three individuals dropped out of the study group and four dropped out of the control group(χ2=0.186,p=0.712). At the end of the study, treatment was considered effective in 32 of the 37 (86.5%)participants in the study group and in 22 of the 35 (62.9%) participants in the control group (χ2=5.36,p=0.021). Repeated measures analysis of variance showed that the improvement in OCD symptoms was greater in the study group than the control group by the 6thweek of treatment. At the end of the trial all 5 cognitive dimensions assessed by the RBANS were significantly better in study groups subjects than in control group subjects and the changes in the YBOCS score were significantly correlated with changes in the RBANS overall score in the study group (r=0.43,p=0.007), but not in the control group (r=0.171,p=0.327).Conclusions:This methodologically rigorous study demonstrates that 8 weeks of adjunctive treatment with EEG biofeedback training can significantly improve the clinical symptoms and cognitive functioning of OCD patients being treated with medication and psychotherapy. Further work is needed to assess the long-term effects of biofeedback training and the need for booster sessions after an initial period of training.
[Shanghai Arch Psychiatry. 2014;26(5)∶ 272-279. doi∶ http∶//dx.doi.org/10.11919/j.issn.1002-0829.214067]
1Renmin Hospital of Wuhan University, Wuhan, Hubei Province, China
2Jingzhou Mental Health Center, Jingzhou, Hubei Province, China
*correspondence∶ jzxlys@163.com
A full-text Chinese translation of this article will be available at www.shanghaiarchivesofpsychiatry.org on November 25, 2014.
50 min cognitive-behavior therapy (CBT) sessions once a week for 8 weeks. CBT was conducted by four psychiatrists who graduated from a 3-year course in CBT and had more than 10 years of experience providing CBT. The specific procedures included∶ (a) establishing rapport with patients; (b)comprehensively understanding the patients’ specific psychological symptoms and requesting that they take daily notes about their ‘automatic thoughts’, emotional reactions and duration of symptoms; (c) analyzing symptoms with patients; and (d) helping the patients overcome maladaptive beliefs by engaging in objective and reasonable thinking.[5]
背景∶ 目前对强迫症(OCD)的干预措施往往疗效有限。目的评价脑电生物反馈训练作为强迫症患者症状和认知功能辅助治疗的效果。方法∶ 共79名强迫症患者随机分为研究组(n=40)和对照组(n=39)。对照组服用舍曲林(50~200mg/d)合并每周一次、连续8周的认知行为治疗;研究组采用相同的方案再加上脑电生物反馈训练,每周5次。由一位单盲于患者治疗状态的精神科医师分别在治疗前和治疗第2周末、第4周末、第6周末和第8周末采用耶鲁-布朗强迫量表(YBOCS)对患者进行评估;采用重复性神经心理状态成套测验(RBANS)在试验前和8周后对患者进行评估。结果∶研究组有3例脱落,对照组有4例脱落(χ2=0.186,p=0.712)。在研究结束时,研究组37例中32例治疗有效(86.5%),对照组35例中22例治疗有效(62.9%)(χ2=5.36,p=0.021)。重复测量方差分析表明治疗6周时研究组强迫症症状的改善显著大于对照组。试验结束时,研究组患者的RBANS量表所有5个维度的认知评估均显著好于对照组,并且研究组YBOCS评分的变化与RBANS总分的变化显著相关(r=0.43,p=0.007),但在对照组中不相关(r=0.171,p=0.327)。结论∶该项方法严谨的研究表明,强迫症患者在接受药物和心理治疗的同时辅以8周的脑电生物反馈训练可显著改善临床症状和认知功能。今后需要进一步开展工作以评估生物反馈训练的长期效果和初始阶段训练后强化训练的必要性。
本文全文中文版从2014年11月25日起在www.shanghaiarchivesofpsychaitry.org可供免费阅览下载
- 上海精神医学的其它文章
- Rank regression: an alternative regression approach for data with outliers
- Internal consistency and test-retest reliability of the Chinese version of the 5-item Duke University Religion Index
- Case report on Tourette syndrome treated successfully with aripiprazole
- Should major depressive disorder with mixed features be classified as a bipolar disorder?
- Case control study of association between the ANK3 rs10761482 polymorphism and schizophrenia in persons of Uyghur nationality living in Xinjiang China
- Cross-sectional study of the association of cognitive function and hippocampal volume among healthy elderly adults

