青年冠心病危险因素的探讨
全勇俊,朱 航,苏小俊,王昊天,何 凯,张子云,孙金燕
青年冠心病危险因素的探讨
全勇俊1,朱 航2,苏小俊1,王昊天3,何 凯4,张子云5,孙金燕1
目的探讨青年冠心病的危险因素。方法选择2008-06至2013-03在解放军总医院门诊及住院期间收治的青年(年龄≤40岁)疑似冠心病患者855例,其中确诊为青年冠心病455例(冠心病组)和非冠心病400例(对照组)。详细采集病史,用高效液相色谱法检测血清同型半胱氨酸(homocysteine,Hcy)水平。采用单因素与多因素非条件Logistic 回归分析青年冠心病患者病因及危险因素。结果冠心病组和对照组在冠心病家族史、HDL-C、APOA1、血Hcy指标的差异均有统计学意义(P<0.01 或P<0.05)。多因素非条件Logistic 回归分析显示:冠心病家族史(OR=3.556,P=0.002)、Hcy(OR=1.380,P=0.001)是青年冠心病患者的独立危险因素。结论血浆Hcy水平和冠心病家族史是青年冠心病患者的危险因素。
冠心病;同型半胱氨酸;青年;危险因素
冠心病是脂代谢紊乱而引起的冠状动脉粥样硬化性病变,具有高发病率和高病死率,且发病趋势越来越年轻化。青年冠心病预后评估取决于对危险因素的干预和对病情的诊断。多项研究证实,同型半胱氨酸(homocysteine,Hcy)是心肺血管疾病的独立危险因素[1,2]。血浆Hcy水平与青年冠心病的关系,尚缺乏充分的研究。本研究将通过对大量青年冠心病患者有效指标的评估,旨在探讨Hcy及其他传统冠心病危险因素与青年冠心病的关系,为中国人群中青年冠心病的危险因素的评估及早期诊断提供依据。
1 对象与方法
1.1 对象 选择2011-06至2013-03在解放军总医院门诊及住院期间收治的,年龄≤40岁的疑似冠心病患者855例,排除不符合WHO缺血性心脏病标准或临床资料不完整的患者,排除患有脑梗死病史,严重的肝肾疾病、恶性肿瘤、自身免疫性疾病、应用叶酸或利尿药等影响Hcy水平药物的疾病者。其中,根据冠状动脉造影、心电图及血压等诊断为青年冠心病455例(青年冠心病组),非冠心病400例(对照组)。
1.2 病史采集 通过临床资料及问诊调查患者性别、年龄、高血压、糖尿病和冠心病病史及家族史、2型糖尿病病史等。
1.3 血浆标本收集方法 入选者采用Judkins法行冠状动脉造影后,Seldinger法穿刺抽取静脉血,加入抗凝药后, 于3000 r/min,离心10 min, 取血清于-80 ℃冰箱中保存待测。
1.4 血浆Hcy含量测定 血浆Hcy水平用高效液相色谱法(日本Shimadzu公司)进行检测。
1.5 相关观察指标 所有患者于入院后取隔夜空腹12 h 静脉血,按中华医学会检验学会推荐的方法测定总胆固醇(TC)、三酰甘油(TG)、高密度脂蛋白胆固醇(HDL-C)、低密度脂蛋白胆固醇(LDL-C)等指标。

2 结 果
2.1 单因素分析 青年冠心病组和对照组在性别、年龄、高血压病史、收缩压、2型糖尿病病史、TG、TC、LDL-C、APOB值等方面比较,差异均无统计学意义,但在冠心病家族史、HDL-C、APOA1、Hcy上比较,差异均有统计学意义(P<0.05,表1、2)。
2.2 多因素分析 多因素非条件Logistic 回归分析结果显示,冠心病家族史、Hcy是青年冠心病患者的独立危险因素(表3)。
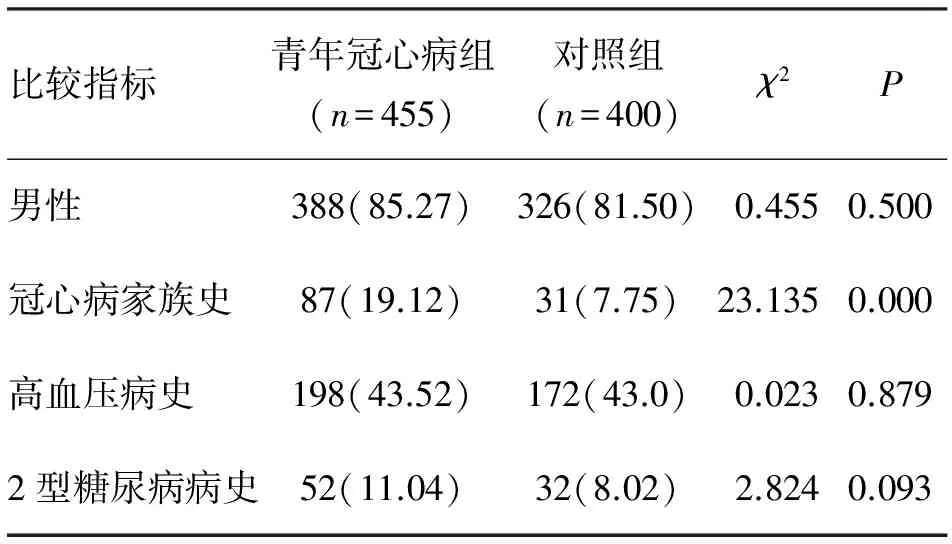
表1 青年冠心病组和对照组患者的计数资料比较 (n;%)


比较指标青年CHD组(n=455)对照组(n=400)tP年龄(岁)36.5±0.334.6±3.6 0.2010.841收缩压(mmHg)94±592±7 0.1320.895TG(mmol/L)2.09±1.521.63±0.690.0430.482TC(mmol/L)4.93±1.214.82±2.061.3250.185LDL⁃C(mmol/L)2.72±1.232.55±1.311.8450.065HDL⁃C(mmol/L)0.90±0.241.21±1.472.3010.022APOA1(mmol/L)1.04±0.521.24±0.812.0000.045APOB(mmol/L)217±98 220±1071.1150.265Hcy(μmol/L)19.23±8.43 15.72±6.32 5.2840.000

表3 青年冠心病危险因素的非条件Logistic 回归分析
3 讨 论
近期研究表明,青年冠心病患者由于其特殊人群、不同的生活及饮食习惯,在临床表现及冠脉病变上有着自身特点[3-5]。因此,不能仅依据传统冠心病的危险因素及指标来评估青年冠心病,需要更加精确的符合青年冠心病特点的评估手段。本次研究目的是通过采集大量青年冠心病患者,在大样本(>400例)的情况下探讨青年冠心病患者与血浆Hcy水平及其他危险因素的关系,更加准确地评估青年冠心病危险因素。
本研究发现,青年冠心病组与对照组的比较中,冠心病家族史、HDL-C、APOA1、HCY差异均具有统计学意义(P<0.05)。进一步对青年冠心病危险因素进行多因素非条件Logistic 回归分析发现,冠心病家族史、Hcy又是青年冠心病患者的独立危险因素。
青年冠心病患者血浆Hcy水平可能与青年患者的遗传因素有关[7,8],基因多态性主要是参与Hcy代谢的酶的突变或缺陷,主要包括3种:亚甲基四氢叶酸还原酶(MTHFR)基因多态性[9-13]、蛋氨酸合成酶基因多态性[14,15],以及CBS基因多态性[16,17]。另外,随着生活水平的提高,青年人的生活习惯也影响着血Hcy水平。研究表明,长期嗜酒可引起肝细胞的蛋氨酸合成酶活性下降,造成高Hcy血症[18]。吸烟、饮食中摄入过多蛋氨酸、饮用高糖咖啡饮品等,均可导致血浆Hcy浓度升高,而且几种因素联合作用明显大于各因素的单独作用[19,21]。研究发现,不受冠心病已知危险因素的影响,Hcy水平每增加5 μmol/L,发生冠心病的危险性将增高约20%[22]。高Hcy血症可通过血管内皮及平滑肌细胞、炎性作用、凝血因子及血小板等多因素共同作用,在短期内发展成动脉粥样硬化。
本研究结果示,Hcy是青年冠心病独立的危险因素,可作为青年冠心病发病的预测分子。根据青年的血浆Hcy水平及对遗传因素对冠心病早期发病风险进行分层,有助于对青年冠心病的早期干预。随着生活条件的提升,高脂饮食,长期吸烟嗜酒等常见的不良习惯也影响着青年冠心病的发病率。通过预防这些不良因素可有效控制青年冠心病发病率。
[1] Wan J, Deng Y, Guo J,etal. Hyperhomocysteinemia inhibited cardiac stem cell homing into the peri-infarcted area post myocardial infarction in rats [J]. Exp Mol Pathol, 2011, 91(1): 411-418.
[2] 朱 航,薛 浩,王广义,等. 血清同型半胱氨酸水平与急性肺栓塞患者早期死亡的相关性[J]. 中华心血管病杂志,2013, 41(9): 756-760.
[3] Che J, Li G, Shao Y,etal. An analysis of the risk factors for premature coronary artery disease in young and middle-age Chinese patients with hypertension [J]. Exp Clin Cardiol, 2013, 18 (2): 89-92.
[4] Cameron S J, Block R C, Richeson J F. Severe coronary disease in an adult considered at low cardiovascular disease risk with a healthy lifestyle [J]. J Clin Lipidol, 2013, 7(5): 526-530.
[5] Huang Y, Hu Y, Mai W,etal. Plasma oxidized low-density lipoprotein is an independent risk factor in young patients with coronary artery disease [J]. Dis Markers, 2011, 31 (5): 295-301.
[6] Forges T, Monnier-Barbarino P, Alberto J M,etal. Impact of folate and homocysteine metabolism on human reproductive health [J]. Hum Reprod Update, 2007, 13 (3): 225-238.
[7] Zidan H E, Rezk N A, Mohammed D. MTHFR C677T and A1298C gene polymorphisms and their relation to homocysteine level in Egyptian children with congenital heart diseases [J]. Gene, 2013, 529 (1): 119-124.
[8] Gupta S K, Kotwal J, Kotwal A,etal. Role of homocysteine & MTHFR C677T gene polymorphism as risk factors for coronary artery disease in young Indians [J]. Indian J Med Res, 2012, 135(4): 506-512.
[9] Arai H, Yamamoto A, Matsuzawa Y,etal. Polymorphisms of apolipoproteine and methylenetetrahydrofolate reductase in the Japanese population [J]. J Atheroscler Thromb, 2007, 14 (4): 167-171.
[10] Terruzzi I, Senesi P, Montesano A,etal. Genetic polymorphisms of the enzymes involved in DNA methylation and synthesis in elite athletes [J]. Physiol Genomics, 2011, 43(16): 965-973.
[11] Bahadir A, Eroz R, Dikici S. Investigation of MTHFR C677T gene polymorphism, biochemical and clinical parameters in Turkish migraine patients: association with allodynia and fatigue [J]. Cell Mol Neurobiol, 2013, 33(8): 1055-1063.
[12] Ubeda N, Reyes L, González-Medina A,etal. Physiologic changes in homocysteine metabolism in pregnancy: a longitudinal study in Spain [J]. Nutrition, 2011, 27(9): 925-930.
[13] Lefaucheur R, Triquenot-Bagan A, Quillard M,etal. Stroke and iridodonesis revealing a homocystinuria caused by a compound heterozygous mutation of cystathionine beta-synthase [J]. Rev Neurol, 2008, 164 (8-9): 728-732.
[14] Hosseini M. Role of polymorphism of methyltetrahydrofolate-homocysteine methyltransferase (MTR) A2756G and breast cancer risk [J]. Pol J Pathol, 2013, 64 (3):191-195.
[15] Belkahla R, Omezzine A, Kchok K,etal. Effect of polymorphisms on key enzymes in homocysteine metabolism, on plasma homocysteine level and on coronary artery-disease risk in a Tunisian population [J]. Ann Cardiol Angeiol, 2008, 57 (4): 219-224.
[16] Nienaber-Rousseau C, Ellis S M, Moss S J,etal. Gene-environment and gene-gene interactions of specific MTHFR, MTR and CBS gene variants in relation to homocysteine in black South Africans [J]. Gene, 2013, 530 (1): 113-118.
[17] Van Meurs J B, Pare G, Schwartz S M,etal. Common genetic loci influencing plasma homocysteine concentrations and their effect on risk of coronary artery disease [J]. Am J Clin Nutr, 2013, 98 (3): 668-676.
[18] Franco Brochado M J, Domenici F A, Candolo Martinelli A D,etal. Methylenetetrahydrofolate reductase gene polymorphism and serum homocysteine levels in nonalcoholic fatty liver disease [J]. Ann Nutr Metab, 2013, 63 (3): 193-199.
[19] Chuang C H, Lee Y Y, Sheu B F,etal. Homocysteine and C-reactive protein as useful surrogate markers for evaluating CKD risk in adults [J]. Kidney Blood Press Res, 2013, 37 (4-5): 402-413.
[20] Bigio R S, Verly E Jr, de Castro M A,etal. Are plasma homocysteine concentrations in Brazilian adolescents influenced by the intake of the main food sources of natural folate ? [J]. Ann Nutr Metab, 2013, 62 (4): 331-338.
[22] Linda L, Rongwei F, Kevin R,etal. Homocysteine level and coronary heart disease incidence [J]. Mayo Clin Proc, 2008, 83 (11): 1203-1212.
(2013-12-24收稿 2014-03-25修回)
(责任编辑 武建虎)
Astudyonriskfactorsinyoungpatientswithcoronaryheartdisease
QUAN Yongjun1, ZHU Hang2, SU Xiaojun1, WANG Haotian3, HE kai4, ZHANG Ziyun5, and SUN Jinyan1.
1. Medical College of Nankai University, Tianjin 300071, China; 2. Department of Cardiology, Chinese PLA General Hospital, Beijing 100853, China; 3. Medical Center of Tsinghua University, Beijing 100084, China; 4. Department of Cardiology, People’s Hospital of Chongqing Municipality,Chongqing 400053, China; 5. Department of Cardiology, Henan Honli Hospital, Changyuan 453400, China
ObjectiveTo study the risk factors in young patients with coronary heart disease.MethodsA total of 855 patients (age≤40 years) hospitalized in this department between June 2011 and March 2013 were included in this study. Patients with definite diagnosis were as young coronary heart disease group (n=455) and other patients were as control group (n=400). Their serum homocysteine was measured by high performance liquid chromatography. The single factor analysis and multivariate logistic regression analysis were used for risk factors of young coronary heart disease.ResultsThe serum Hcy, family history of coronary heart disease in young coronary heart disease group were all higher than those in control group(P<0.01 orP<0.05). The logistic regression analysis demonstrated that Hcy(OR=1.380,P=0.001)and history of coronary heart disease(OR=3.556,P=0.002)were all independent risk factors for young coronary heart disease patients.ConclusionsHigh serum homocysteine and family history of CHD are independent risk factors for young CHD patients.
coronary heart disease; homocystein; young; risk factors
全勇俊,硕士研究生,E-mail:qyongjun@yeah.net
1.300071天津,南开大学医学院;2. 100853北京,解放军总医院心内科;3. 100084北京,清华大学医学中心;4.400053,重庆市第十三人民医院心内科;5.453400长垣,河南宏力医院心血管内科
朱 航,E-mail: zhuhang301@126.com
R541.4

