二硫代氨基吡咯烷对大鼠急性肺损伤保护作用
王大龙,冷玉芳
(1.山东省胜利油田中心医院麻醉科,东营 257000;2.兰州大学第一医院麻醉科,兰州 730000)
二硫代氨基吡咯烷对大鼠急性肺损伤保护作用
王大龙1,冷玉芳2
(1.山东省胜利油田中心医院麻醉科,东营 257000;2.兰州大学第一医院麻醉科,兰州 730000)
目的 探讨二硫代氨基吡咯烷(PDTC)对内毒素(LPS)诱导急性肺损伤(ALI)大鼠肺组织的保护作用及其机制。方法将72只Wistar大鼠随机分为对照组(C组),LPS组(L组),PDTC+LPS组(P组)。各组分为1,3,6,12 h亚组,每组6只。L组和P组制作内毒素性肺损伤模型。P组腹腔注射LPS前30 min尾静脉注射PDTC,120 mg·kg-1,L组和C组给予等体积0.9%氯化钠溶液。观察大鼠肺组织病理变化,肺组织湿/干质量比(W/D)变化,RT-PCR法检测大鼠肺组织细胞间黏附分子-1 mRNA(ICAM-1mRNA)的表达,放射免疫法检测大鼠血清肿瘤坏死因子α(TNF-α)、白细胞介素6(IL-6)含量变化。结果病理切片显示,与C组比较,L组肺组织结构破坏严重,W/D明显增大,ICAM-1mRNA在各时间点表达明显增强(P<0.05),血清TNF-α、IL-6含量在1,3,6 h增高(P<0.05)。与L组比较,P组肺组织结构破坏明显减轻,W/D减小(P<0.05),ICAM-1mRNA表达明显减少(P<0.05),血清TNF-α、IL-6含量1,3,6 h降低(P<0.05或P<0.01)。结论PDTC能明显抑制ICAM-1mRNA表达,降低TNF-α和IL-6含量,PDTC可能对ALI大鼠有保护作用。
二硫代氨基吡咯烷;核因子-κB;内毒素;损伤,肺,急性
急性肺损伤(acute lung injury,ALI)/急性呼吸窘迫综合征(acute respiratory distress syndrome,ARDS)是由严重感染、创伤和休克等多种病因所致的弥漫性肺实质损伤,其在分子水平上表现为众多促炎性细胞因子、粘附分子的过度表达,伴有多种炎症递质的产生。炎症递质的释放导致肺组织广泛损害,并累及诸多肺外器官[1]。研究证明,抗氧化药二硫代氨基吡咯烷(pyrrolidine dithiocarbamate,PDTC)能够通过抑制重要的核因子-κB(nuclear factor-kappa B,NF-κB)活化,减少致炎细胞因子表达与合成释放[2-3]。笔者在本实验中建立大鼠内毒素(lipopolysaccharides,LPS)性肺损伤模型,研究PDTC对LPS诱导ALI大鼠肺组织细胞间黏附分子1(intercellular adhesion molecule-1mRNA, ICAM-1mRNA)和血清肿瘤坏死因子-α(tumor necrosis factor-α,TNF-α)、白细胞介素6(interleukin-6,IL-6)含量的影响,以探讨PDTC肺损伤的保护作用及其机制。
1 材料与方法
1.1 动物与试剂 雄性Wistar大鼠(由兰州大学医学院实验动物中心提供)72只,LPS(EColi055:B5)和PDTC购自sigma公司(批号:P8765,纯度>99%),核酸提取试剂购自百泰克,RNA试剂盒购自Fermentas公司。
1.2 造模与给药方法 72只Wistar大鼠,体质量200~250 g,随机分为3组:对照组(C组),LPS组(L组),PDTC+LPS组(P组)。根据腹腔注射LPS到取肺组织的时间分为1,3,6,12 h亚组,每组6只。L组和P组腹腔注射LPS8 mg·kg-1制作内毒素性肺损伤模型,C组腹腔注射同体积0.9%氯化钠溶液。P组在腹腔注射LPS前30 min,尾静脉注射PDTC120 mg·kg-1(稀释到60 mg·mL-1),L组和C组给予同体积0.9%氯化钠溶液。按分组规定的时间点,10%水合氯醛350 mg·kg-1腹腔注射麻醉,开胸心脏放血处死,采集标本。
1.3 观察指标
1.3.1 肺组织病理检查 取右肺上叶,4%多聚甲醛固定,石蜡包埋,苏木精-伊红(hematoxylin-eosinstaining,HE)染色后光镜下观察肺组织形态学变化。
1.3.2 肺组织湿/干重比值(wet/dry ratio of lung,W/D)监测 取左肺,滤纸拭去表面血液,称湿重后置于80℃烤箱烘烤48 h,使肺组织达恒重后称干重,计算W/D值。
1.3.3 ICAM-1mRNA监测 用PCR专用器械迅速取右肺下叶,经预冷的焦碳酸二乙酯(diethypyrocarbonate,DEPC)水冲洗表面的血液后立即置于液氮中速冻,-80℃冰箱保存,待测逆转录PCR(reverse transcription-PCR,RT-PCR)。用RNA提取试剂Trizol提取肺组织总RNA,反转录合成cDNA第一条链。取反转录产物2 μL进行PCR反应(94℃变性5 min,59℃复性30 s,72℃延伸1 min,35个循环)。扩增组织中ICAM-1的引物为:5′-AGGTATCCATCCATCCCACA-3′和5′-AGTGTCTCATTCCCACGGAG-3′,片段长度为388 bp;扩增内对照β-actin的引物为:β-actin引物5′-GTGGGCCGCTGTAGGCACCAA-3′和5′-CTCTTTGATGTCGCACGATTTC-3′,片段长度为540 bp。由上海赛百盛有限公司合成。PCR扩增产物用1%琼脂糖凝胶电泳,溴化乙锭染色显示,凝胶图像分析系统分析,以ICAM-1mRNA/β-actinmRNA电泳带的荧光强度比值作为ICAM-1mRNA的表达量指标。
1.3.4 TNF-α、IL-6含量监测 取血液37℃水浴0.5 h后离心(2 500×g,10 min),取上层血清-70℃冰箱保存备用。放免法测定TNF-α、IL-6含量。
1.4 统计学方法 用SPSS 18.0版统计软件分析,计量资料以均数±标准差(±s)表示,组内及组间比较采用t检验,以P<0.05为差异有统计学意义。
2 结果
2.1 两组形态学改变比较 光镜下可见C组肺泡结构完整,肺泡壁无水肿,无炎症细胞浸润;L组基本看不到完整肺泡结构,肺间质及肺泡毛细血管明显扩张、片状出血,支气管壁、肺泡间隔及毛细血管周围有大量炎症细胞浸润;P组肺泡结构轻微破坏,可见代偿增大的肺泡,无明显的水肿、淤血,炎症细胞浸润较L组少。
2.2 两组W/D值比较 与C组比较,P组和L组W/D值在模型建立后1,3,6,12 h均明显升高(P<0.05);与L组比较,P组W/D值在相同时间点均明显降低(P<0.05),见表1。
2.3 两组肺组织ICAM-1mRNA表达 与C组比较,L组和P组模型建立后相同时间点ICAM-1mRNA表达量均显著增加(P<0.05),12 h达到高峰;与L组相比, P组在各时间点ICAM-1mRNA表达量显著降低(P<0.05)。见表2。
2.4 两组血清TNF-α、IL-6含量 与C组相比,L组和P组血清TNF-α水平在1,3,6 h均显著升高(P<0.01),1 h达高峰,随着时间延长而降低;与L组比较,P组在1,3,6 h TNF-α表达量均显著低于L组(P<0.05或P<0.01)。与C组比较,L组和P组血清IL-6水平在1,3,6 h均显著升高(P<0.01),3 h达高峰;与L组比较,P组1,3 h IL-6表达量均显著低于L组(P<0.05),见表3。
表1 3组大鼠肺组织W/D比值Tab.1 W/D ratio in lung tissue of three groups of rats ±s
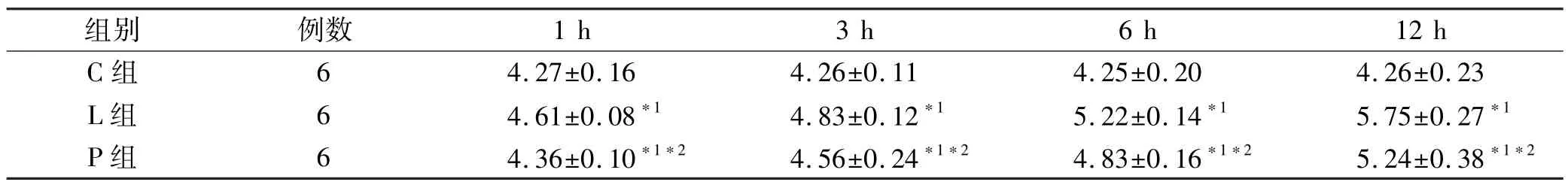
表1 3组大鼠肺组织W/D比值Tab.1 W/D ratio in lung tissue of three groups of rats ±s
与C组比较,*1P<0.05;与L组比较,*2P<0.05Compared with group C,*1P<0.05;Compared with group L,*2P<0.05
组别例数1 h3 h6 h12 h C组64.27±0.164.26±0.114.25±0.204.26±0.23 L组64.61±0.08*14.83±0.12*15.22±0.14*15.75±0.27*1P组64.36±0.10*1*24.56±0.24*1*24.83±0.16*1*25.24±0.38*1*2
表2 3组大鼠肺组织ICAM-mRNA表达量Tab.2 ICAM-mRNA expression in lung tissue of three groups of rats ±s
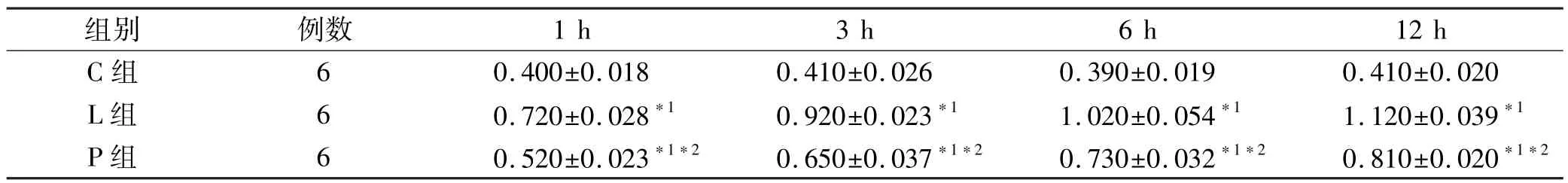
表2 3组大鼠肺组织ICAM-mRNA表达量Tab.2 ICAM-mRNA expression in lung tissue of three groups of rats ±s
与C组比较,*1P<0.05;与L组比较,*2P<0.05Compared with group C,*1P<0.05;Compared with group L,*2P<0.05
组别例数1 h3 h6 h12 h C组60.400±0.0180.410±0.0260.390±0.0190.410±0.020 L组60.720±0.028*10.920±0.023*11.020±0.054*11.120±0.039*1P组60.520±0.023*1*20.650±0.037*1*20.730±0.032*1*20.810±0.020*1*2
表3 3组大鼠血清TNF-α与IL-6含量Tab.3 Serum content of TNF-α and IL-6 in three groups of rats ±s
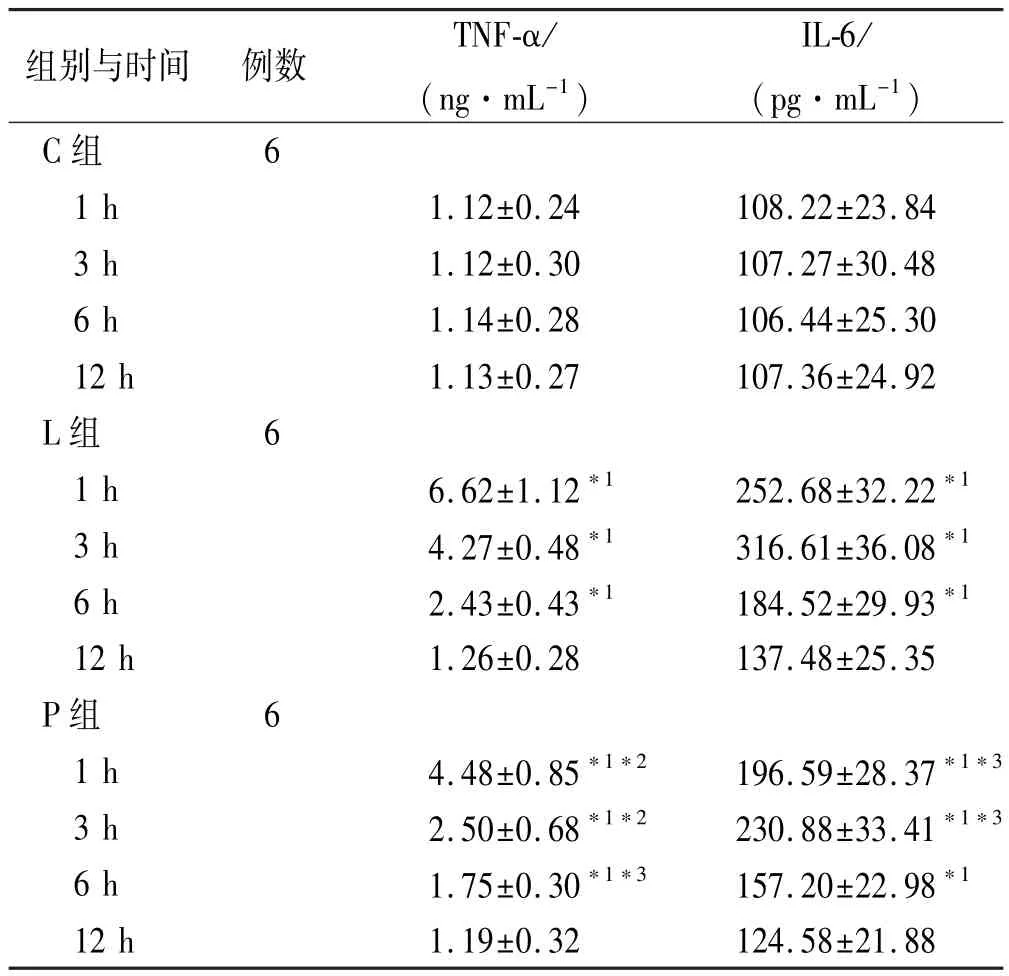
表3 3组大鼠血清TNF-α与IL-6含量Tab.3 Serum content of TNF-α and IL-6 in three groups of rats ±s
与C组比较,*1P<0.01;与L组比较,*2P<0.01,*3P<0.05Compared with group C,*1P<0.01;compared with group L,*2P<0.01,*3P<0.05
组别与时间例数TNF-α/(ng·mL-1) IL-6/(pg·mL-1) C组6 1 h1.12±0.24108.22±23.84 3 h1.12±0.30107.27±30.48 6 h1.14±0.28106.44±25.30 12 h1.13±0.27107.36±24.92 L组6 1 h6.62±1.12*1252.68±32.22*13 h4.27±0.48*1316.61±36.08*16 h2.43±0.43*1184.52±29.93*112 h1.26±0.28137.48±25.35 P组6 1 h4.48±0.85*1*2196.59±28.37*1*33 h2.50±0.68*1*2230.88±33.41*1*36 h1.75±0.30*1*3157.20±22.98*112 h1.19±0.32124.58±21.88
3 讨论
腹腔注射LPS是建立大鼠ALI模型的经典方法,本实验中大鼠注射LPS 1 h后,呼吸加快,四肢、口唇紫绀,个别大鼠发出喘鸣音,口鼻内涌出粉红色泡沫,拒食,竖毛,轻度腹泻,W/D增加。光镜下肺泡结构基本消失,肺间质及肺泡毛细血管明显扩张、片状出血,支气管壁、肺泡间隔及毛细血管周围有大量炎症细胞浸润,说明ALI模型建立成功[4]。LPS主要与巨噬细胞Toll受体结合,启动胞内信号传递链,促进κIBα亚型的降解并活化NF-κB的DNA结合能力,启动基因转录,表达和释放多种细胞因子,发挥其毒性作用[5-7]。
本实验中L组在注射内毒素后,肺组织ICAM-1mRNA,血清中TNF-α、IL-6含量均有增高(P<0.05或P<0.01),提示ICAM-1、TNF-α和IL-6作为炎症因子在LPS诱导的ALI发病过程中起重要作用。ICAM-1通过介导细胞与细胞间,细胞与细胞外基质间的粘附作用,使大量的多形核白细胞(polymorphonuclear, PMN)黏附于肺血管内皮细胞、在肺内扣押并释放生物活性递质[8]。TNF-α能诱导肺内上皮细胞活化、白细胞迁移和毛细血管渗漏,积聚的水肿液进一步阻碍肺泡内细胞的灌流和氧气的交换,引起肺损伤。TNF-α的含量改变可反映其他炎症因子的改变情况[7,9]。IL-6是一种迟发性细胞因子,可以诱导活化的B细胞增殖和分化,激活T细胞,在诱导和维持炎症反应中起重要作用。在急性炎性反应中,IL-6的水平与病情严重程度密切相关[10]。TNF-α在模型建立后1 h达到峰值,随后降低,提示TNF-α可能是导致ALI和ARDS的始动因素。IL-6在3 h达到高峰,可能与炎症的持续和进一步发展有关。
PDTC是一种抗氧化药,近年来的研究证明它对NF-κB的活性有很强的抑制作用,被认为是NF-κB的特异性抑制药,它的金属鳌合特性和二硫基基团清道夫作用能够选择性的抑制NF-κB活化[2-3,11]:①直接抑制NF-κBP65亚单位;②抑制NF-κB抑制药κIB的降解;③减少NF-κB的核移位。ICAM-1、TNF-α和IL-6的基因启动子上都含有NF-κB结合位点,NF-κB的激活,促进其表达;它们又可反过来进一步活化NF-κB,使炎症不断放大。在大鼠注射LPS以后活化了NF-κB,促使肺血管内皮细胞上三类基因的表达明显上调,促进白细胞粘附、扣押于肺泡区域,导致肺实质细胞损伤及持续细胞因子释放,使毛细血管渗漏,积聚的水肿液进一步阻碍肺泡内细胞的灌流和氧气的交换,引起肺损伤加重肺组织损伤[12-13]。本实验应用PDTC后的结果显示,P组肺泡结构破坏轻微,可看到代偿增大的肺泡,无明显的水肿、淤血,仅有少量炎症细胞浸润, W/D值增大,同时ICAM-1mRNA表达显著减轻,血清TNF-α、IL-6含量减少。表明PDTC通过减少肺组织ICAM-1mRNA表达,减轻PMN在肺组织内的聚集和激活,减少炎症因子TNF-α、IL-6的表达抑制肺损伤时的炎症反应,产生肺保护作用[14]。但是在本实验中未对不同剂量的PDTC进行比较,将来作为进一步研究的目标。
综上所述,PDTC预先给药对LPS诱导的大鼠ALI有一定的保护作用,与减少肺组织ICAM-1mRNA表达,抑制TNF-α、IL-6的表达有关。
[1] BLACKWELL T S,CHRISTMAN J W.The role of nuclear factor-kappa B in cytokine gene regulation[J].Am J Respir Cell Mol Biol,1997,17(1):3-9.
[2] KABAY B,TEKE Z,AYTEKIN F O,et al.Pyrrolidine dithiocarbamate reduces lung injury caused by mesenteric ischemia/reperfusion in a rat model[J].World J Surg,2007, 31(8):1707-1715.
[3] LA ROSA G,CARDALI S,GENOVESE T,et al.Inhibition of the nuclear factor-kappa B activation with pyrrolidine dithiocarbamate attenuating inflammation and oxidative stress after experimental spinal cord trauma in rats[J].J Neurosurg Spine,2004,1(3):311-321.
[4] TSENG T L,CHEN M F,TSAI M J,et al.Oroxylin-A rescues LPS-induced acute lung injury via regulation of NF-kappaB signaling pathway in rodents[J].Plos ONE,2012,7 (10):e47403.
[5] EDELMAN D A,JIANG Y,TYBURSKI J G,et al.Cytokine production in lipopolysaccharide-exposed rat lung pericytes [J].J Trauma,2007,62(1):89-93.
[6] ZHOU X,GAO X P,FAN J,et al.LPS activation of Toll-like receptor 4 signals CD11b/CD18 expression in neutrophils [J].Am J Physiol Lung Cell Mol Physiol,2005,288(4): 655-662.
[7] ZHOU Z,CONNELL M C,MACEWAN D J.TNFR1-induced NF-kappa B,but not ERK,p38MAPK or JNK activation,mediates TNF-induced ICAM-1 and VCAM-1 expression on endothelial cells[J].Cell Signal,2007,19(6): 1238-1248.
[8] ZHANG J S,TAN Y R,XIANG Y,et al.Regulatory peptides modulate adhesion of polymorphonuclear leukocytes to bronchial epithelial cells through regulation of interleukins, ICAM-1 and NF-kappaB/IkappaB[J].Acta Biochim Biophys Sin(Shanghai),2006,38(2):119-128.
[9] TANG X,METZGER D,LEEMAN S,et al.LPS-induced TNF-alpha factor(LITAF)-deficient mice express reduced LPS-induced cytokine:Evidence for LITAF-dependent LPS signaling pathways[J].Proc Natl Acad Sci USA,2006,103 (37):13777-13782.
[10] SHANLEY T P,FOREBACK J L,REMICK D G,et al.Regulatory effects of interleukin-6 in immunoglobulin G immune-complex-induced lung injury[J].Am J Pathol,1997, 151(1):193-203.
[11] 唐庆,范恒,胡慧,等.氧化苦参碱对结肠炎模型大鼠结肠黏膜NOD2与TNF-α的影响[J].医药导报,2012,31 (2):138-141.
[12] SAWA Y,UEKI T,HATA M,et al.LPS-induced IL-6,IL-8, VCAM-1,and ICAM-1 expression in human lymphatic endothelium[J].J Histochem Cytochem,2008,56(2):97-109.
[13] YUSUF-MAKAGIANSAR H,YAKIVLEVA T V,TEJO B A, et al.Sequence recognition of alpha-LFA-1-derived peptides by ICAM-1 cell receptors:inhibitors of T-cell adhesion[J]. Chem Biol Drug Des,2007,70(3):237-246.
[14] ZHAI J X,ZHANG Z X,FENG Y J,et al.PDTC attenuate LPS-induced kidney injury in systemic lupus erythematosusprone MRL/lpr mice[J].Mol Biol Rep,2012,39(6): 6763-6771.
DOI 10.3870/yydb.2014.03.009
Protective Effect of PDTC on Acute Lung Injury Induced by LPS in Rats
WANG Da-long1,LENG Yu-fang2
(1.Department of Anesthesiology,Shengli Oilfield Center Hospital,Dongying 257000,China;2.Department of Anesthesiology,the First Hospital of Lanzhou University,Lanzhou 730000, China)
Objective To explore the protective effect of pyrrolidine dithiocarbamate(PDTC)on acute lung injury induced by LPS.MethodsA total of 72 Wistar rats were randomly divided into the control(C),LPS model control(L),and PDTC+LPS(P)treatment groups.Rats in each group were further divided into 1,3,6,12 h subgroups(n=6 each)based on the time between intraperitoneal injection of endotoxin.To produce the endotoxin-induced lung injury model,group L and group P were intraperitoneally injected with LPS 8 mg·kg-1,group C injected with the same volume of normal saline.And group P was injected with PDTC 120 mg·kg-1from the tail vein and half an hour later,LPS was intraperitoneally injected in group P,and the same volume of normal saline was injected to groups C and L.The pathological changes in lung tissue,wet/dry weight(W/D)of lung,ICAM-1mRNA expression in lung and TNF-α and IL-6 in serum were detected.ResultsIn groups P and L,the structure of lungs was seriously injured,the wet/dry weight ratio(W/D)of the lungs was significantly increased,the expression of ICAM-1mRNA was enhanced,and the content of serum TNF-α,IL-6 was elevated.Compared with group L,the injury of lung structure was deceased,lung wet/dry weight ratio(W/D)was significantly declined(P<0.05),the ICAM-1mRNA expression was alleviated(P<0.05),and the serum level of TNF-α and IL-6 was lowered(P<0.05 orP<0.01)in group P.ConclusionPDTC could inhibit the expression of ICAM-1mRNA and reduce TNF-α and IL-6 secretion,which plays a protective role in LPS-induced acute lung injury of rats.
Pyrrolidine dithiocarbamate;Nuclear factor-kappa B;LPS;Injury,lung,acute
R453.9;R965
A
1004-0781(2014)03-0307-04
2013-03-20
2013-04-15
王大龙(1982-),男,山东泰安人,主治医师,硕士,从事临床麻醉学研究。电话:0546-8770301,E-mail:16719077@qq.com。
冷玉芳(1964-),女,甘肃兰州人,主任医师,博士,从事临床麻醉学研究。电话:0931-8625200-6626,E-mail:lengyf@lzu.edu.cn。