Isolated Pancreatic Tuberculosis in Non-immunocompromised Patient Treated by Whipple’s Procedure: a Case Report
Shao-long Sun, Feng Gao, Dong-xu Cui, and Bao-sheng Wang
Department of General Surgery, Shengjing Hospital of China Medical University, Shenyang 110004, China
PANCREATIC tuberculosis (TB) is a rare disease and its diagnosis is difficult because of the lack of specific clinical manifestations. Computed tomography (CT) and magnetic resonance imaging (MRI) have some diagnostic values in this disease, but it is easy to misdiagnose pancreatic TB as a pancreatic tumor.1In this article, we present a case of non-immunocompromised patient developing an isolated pancreatic TB, report the CT and MRI findings, and the surgical procedure for it.
CASE DESCRIPTION
A 34-year-old man visited our hospital, complaining of abdominal distension and weight loss. The patient reported no history of cough or fever, or immunocompromise. On physical examination, the patient was afebrile, skin and sclera were stained yellow, slight tenderness was present in the upper abdomen, and bowel sounds were normal. Laboratory investigation revealed slightly elevated levels of total bilirubin (39.33 μmol/L) and conjugated bilirubin (27.36 μmol/L). The level of γ-glutamyl transpeptidase (1194.1 U/L) was above the normal range (9-64 U/L). The levels of aspartate aminotransferase (112.3 U/L), alanine aminotransferase (205.5 U/L), and alkaline phosphatase (727.9 U/L) all exceeded the normal ranges. Serum levels of carbohydrate antigen 19-9 and carcinoem- bryonic antigen were within normal limits. Amylase, white blood cell count, and blood glucose level were also within normal ranges. Lung X-ray detected no abnormal signs.
CT revealed a mass of 6.4 cm × 3.8 cm in the neck of the pancreas, with focal hypodense lesion and irregular borders surrounding the common hepatic artery. The distal pancreatic duct was not dilated. Enlarged gallbladder and dilated intrahepatic duct were found. These findings indicated pancreatic tumor and bile duct obstruction. The mass was not enhanced in contrast-enhanced CT (Fig. 1).
MRI revealed an irregular mass of 5.4 cm× 4.2 cm in the neck of the pancreas. The lesion had slightly increased signal intensities on fat-suppressed T1-weighted images. T2-weighted images showed heterogeneous intensity of the lesion with areas of slightly increased signal intensity. The pancreatic segment of the common bile duct was not shown clearly. A dilated intrahepatic duct was found on magnetic resonance cholangiopancreatography (Fig. 2). These findings indicated a pancreatic tumor causing bile duct obstruction.
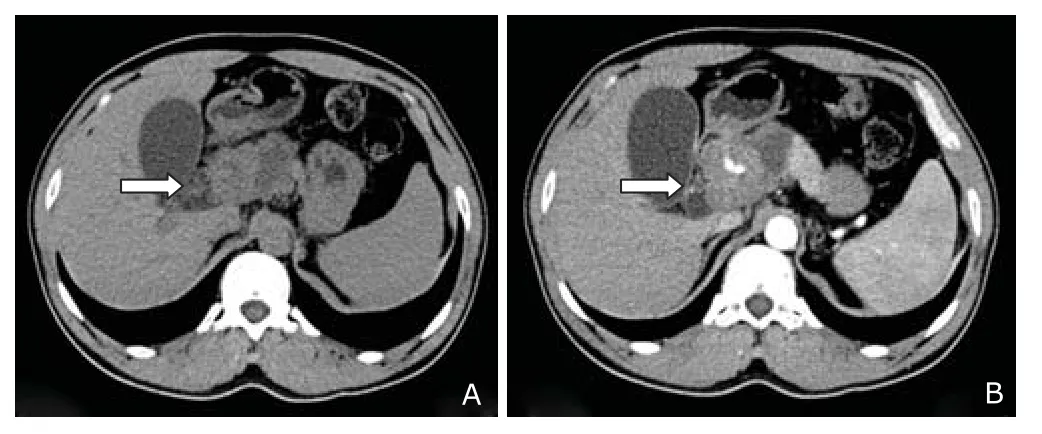
Figure 1. Computed tomography (CT) reveals a mass of 6.4 cm × 3.8 cm in the neck of the pancreas with focal hypodense lesion and irregular borders, surrounding the common hepatic artery (arrow, A). In contrast-enhanced CT, the mass is not enhanced (arrow, B).

Figure 2. Magnetic resonance imaging reveals an irregular mass in the neck of the pancreas. The lesion shows slightly increased signal intensity on fat-suppressed, T1-weighted images (arrow, A). The T2-weighted image shows heterogeneous intensity of the lesion with areas of slightly increased signal intensity (arrow, B). The pancreatic segment of the common bile duct is not shown clearly. A dilated intrahepatic duct is found on magnetic resonance cholangiopancreatography (C).

Figure 3. Pathological photomicrograph of the resected pancreatic tissue shows epithelioid granuloma, caseous necrosis, and Langhans giant cells. (HE, 100×)
Pancreatic TB was confirmed following pancreatoduo- denectomy. Exploratory laparotomy revealed a mass of 6 cm×4 cm at the head of the pancreas, close to the neck of the pancreas. The mass compressed the common bile duct and invaded the common hepatic artery, but was easily separable from the artery. We resected the head of the pancreas, duodenum, gallbladder, common bile duct, part of distal stomach, and a 10-cm section of the jejunum. We employed the sequence of pancreaticoenterostomy, choledochojejunostomy, gastrojejunostomy for anasto- moses after resection. In pancreaticoenterostomy, the jejunum was overlapped to the pancreas, with a silicone tube in the pancreatic duct. The pathological photomicro- graph showed epithelioid granuloma, caseous necrosis, and Langhans giant cells (Fig. 3).
The patient recovered well with no complications, such as pancreatic fistula or infection. Anti-tubercular drugs including isoniazide and rifampin were administrated for a year. In the following 2 years, TB was not relapsed.
DISCUSSION
Pancreatic TB is a rare disease, accounting for 2% of all the TB discovered in autopsy.2Solitary pancreatic involvement of TB in non-immunocompromised patients is even more unusual,3because the pancreas is biologically protected from being infected by Mycobacterium tuberculosis.4Pancreatic TB may mimic pancreatic carcinoma clinically and radiologically.5Anti-tubercular therapy is curative in the majority of pancreatic TB cases and the course of treatment is 6 months to 1 year, with good prognosis. The reliable diagnostic method is biopsy. If misdiagnosed as malignancy, however, pancreatectomy would be inevitable, so careful recognition of pancreatic TB is vital.6
The CT characteristic of pancreatic TB is a hypodense mass with irregular margins and peripheral enhancement, occasionally mimicking pancreatic carcinoma,7whereas in this case, CT showed no enhancement of the mass, possibly suggesting that the mass was not malignant.
To our knowledge, there are few reports on the MRI findings of TB involvement of the pancreas. De Backer et al8described 3 MRI features of pancreatic TB: in 2 patients, T1-weighted images showed a hypointense lesion and heterogeneous signal intensities, with areas of increased and decreased signal intensity in T2-weighted images; in 1 patient, diffuse enlargement of the pancreatic gland was associated with increased signal intensity in T2-weighted images, and heterogeneous decreased signal intensity in T1-weighted images. In the present case, the MRI features were not the same: the lesion had slightly increased signal intensity in both T1-weighted and T2-weighted images.
The patient in this case demonstrated no evidence of other foci of TB. Pancreatic TB should be suspected in patients having a pancreatic mass, particularly if the patient is young, or the erythrocyte sedimentation rate is abnormal, or the patient is known to have been exposed to TB.9When CT and MR cannot confirm the diagnosis, fine-needle aspiration cytology of the pancreatic lesion should be performed, such as endoscopic ultrasound- guided biopsy or CT-guided percutaneous biopsy,10to avoid unnecessary explorative laparotomy, because almost all the cases with pancreatic TB could be treated with medical management.11
1. Sportes A, Kpossou R, Bernardin S. Isolated pancreatic tuberculosis mimicking inoperable pancreatic cancer: a diagnostic challenge resolved using endoscopic ultrasound- guided fine-needle aspiration. Can J Gastroenterol 2013; 27:445-7.
2. Assenza M, Simonelli L, Romeo V, et al. Isolated pancreatic tuberculosis: a diagnostic challenge. Clin Ter 2012; 163: e327-9.
3. Ladas SD, Vaidakis E, Lariou C, et al. Pancreatic tuberculosis in non-immunocompromised patients: reports of two cases, and a literature review. Eur J Gastroenterol Hepatol 1998; 10:973-6.
4. Huang CT, Lo CY, Lee TH. Isolated peripancreatic tuberculous lymphadenopathy: a rare manifestation of abdominal tuberculosis mimicking pancreatic cystic neoplasm. J Dig Dis 2013; 14:105-8.
5. Weiss ES, Klein WM, Yeo CJ. Peripancreatic tuberculosis mimicking pancreatic neoplasia. J Gastrointestinal Surg 2005; 9:254-62.
6. Dang S, Atiq M, Saccente M, et al. Isolated tuberculosis of the pancreas: a case report. JOP 2009; 10:64-6.
7. Sinan T, Sheikh M, Ramadan S. CT features in abdominal tuberculosis: 20 years experience. BMC Med Imaging 2002; 2:3.
8. De Backer AI, Mortelé KJ, Bomans P, et al. Tuberculosis of the pancreas: MRI features. Am J Roentgenol 2005; 184:50-4.
9. Ozkan F, Bulbuloglu E, Inci MF, et al. Isolated pancreatic tuberculosis mimicking malignancy and causing obstructive jaundice. J Gastrointest Cancer 2013; 44:118-20.
10. Khaniya S, Koirala R, Shakya VC, et al. Isolated pancreatic tuberculosis mimicking as carcinoma: a case report and review of the literature. Cases J 2010; 3:18.
11. Ilhan E. Fine needle aspiration biopsy and/or tissue biopsy for avoiding surgery complication in patients with peripan- creatic tuberculosis. JOP 2009; 10:341-2.
 Chinese Medical Sciences Journal2014年1期
Chinese Medical Sciences Journal2014年1期
- Chinese Medical Sciences Journal的其它文章
- Laryngo-tracheobronchial Amyloidosis: a Case Report and Review of Literature
- Factors Associated with Coronary Artery Disease in Young Population (Age≤40): Analysis with 217 Cases
- Bloodstream Infection with Carbapenem-resistant Klebsiella Pneumoniae and Multidrug-resistant Acinetobacter Baumannii: a Case Report
- Comparison of the Outcomes of Monopolar and Bipolar Radiofrequency Ablation in Surgical Treatment of Atrial Fibrillation
- Palliative Local Radiotherapy in the Treatment of Tumor-stage Cutaneous T-cell Lymphoma/ Mycosis Fungoides
- Reversible Posterior Leukoencephalopathy Syndrome in Children with Nephrotic Syndrome: a Case Report
