腹腔镜下垂直切割闭合直肠远端在直肠低位双吻合中的作用和意义
陈少骥 吴云云2 韩善亮 莫秦良 马远明 赵宏
1 苏州大学附属第一医院普外科,江苏 苏州,215000 ;
2 苏州市吴江区第一人民医院外科,江苏 苏州,215000
腹腔镜下垂直切割闭合直肠远端在直肠低位双吻合中的作用和意义
陈少骥吴云云2韩善亮1莫秦良1马远明1赵宏1
1 苏州大学附属第一医院普外科,江苏 苏州,215000 ;
2 苏州市吴江区第一人民医院外科,江苏 苏州,215000
[摘要]背景与目的:中低位直肠癌根治术中行直肠低位双吻合,术后易发生吻合口瘘及“直肠低位前切除术后综合征”等并发症,如何降低这些并发症的发生,目前临床仍处于探索之中。本研究的目的是观察、探讨腹腔镜下垂直切割闭合直肠远端在改进直肠低位双吻合中的作用和意义。方法:将2010年2月—2014年6月在苏州大学附属第一医院普外科完成腹腔镜下直肠癌根治术的120例中低位直肠癌患者,随机分为A、B两组。以性别、年龄、肿瘤大小、下缘离齿状线距离及肿瘤分期等为指标,逐一配对。其中A组(观察组)55例,在进行“第一吻合”时,将常规的直肠远端切割闭合,由水平方向改为垂直方向;行“第二吻合”时,行肠-肠“端-角”吻合,去除直肠远侧闭合线上端角部(“狗耳”);血管夹夹闭去除下端“狗耳”;加强缝合“端-角”吻合后形成的一处钉合线“T”形交汇处(“危险三角”)。B组(对照组)65例,按直肠低位双吻合常规操作完成手术,两只“狗耳”及两处“危险三角”不作任何处理。将两组患者进行对比分析。结果:A组在垂直切割闭合直肠远端后,“狗耳”及“危险三角”均位于同一垂直线上,便于观察和处理。“端-角”吻合后远近端肠管轴线形成一定交角,远端直肠腔形成类似“壶腹”样膨隆;无“狗耳”存在,一处“危险三角”得以缝合加强。B组完成“端-端”吻合后远近端肠管在同一轴线上,留有两只“狗耳”及两处“危险三角”。两组患者的一般临床资料差异无统计学意义(P>0.05)。两组患者术中出血量、术后引流量、术后吻合口出血、肛门排气时间和住院时间差异无统计学意义(P>0.05)。手术耗时、术后吻合口瘘的发生数、排便次数、里急后重、术后再次手术造瘘差异有统计学意义(P<0.05)。结论:直肠低位双吻合时垂直切割闭合远侧直肠,使双吻合后肠管的走行和形态更接近直肠的生理弯曲和形态;同时方便了术中去除“狗耳”和“危险三角”的加强缝合;术后并发症发生率显著降低。
[关键词]中低位直肠癌;直肠低位双吻合;垂直切割闭合;术后并发症
中低位直肠癌在腹腔镜下完成根治性手术时,直肠低位双吻合(double stapling technique,DST)是整个手术的难点和成败的关键[1-2],它与患者术后的功能恢复、并发症的发生具有直接的相关性。现有资料显示,目前直肠低位双吻合口瘘的发生率一般在4%~20%[3];近年来“直肠低位前切除术后综合征”正越来越多地引起的重视[4],该综合征与双吻合口憩室炎等的相关性也正逐渐被国内外学者认识[5]。为方便操作,降低双吻合口术后并发症的发生,本研究将常规双吻合时直肠远端的水平切割闭合改为垂直切割闭合,使直肠低位双吻合的操作变得简捷、方便,并取得了较好的临床效果。
1 资料和方法
1.1一般资料
选择2010年2月—2014年6月在苏州大学附属第一医院普外科收治的中低位直肠癌患者中随机抽取腹腔镜下完成直肠前切除的120例患者,分为观察组(A组)55例,其中男性37例,女性18例;年龄34~88岁,平均60.5岁;肿瘤下缘距齿状线≥5 cm者14例,<5 cm者41例;组织学类型:高分化腺癌8例,中分化腺癌32例,低分化腺癌13例,其他病理类型2例;术后病理上下切缘均为阴性。Dukes分期:A期8例,B期21例,C期26例。对照组(B组)65例,其中男性39例,女性26例;年龄31~80岁,平均59.5岁;肿瘤下缘距齿状线≥5 cm者18例,<5 cm者47例;组织学类型:高分化腺癌9例,中分化腺癌39例,低分化腺癌14例,其他病理类型3例;术后病理上下切缘均阴性。Dukes分期:A期2例,B期34例,C期29例。
1.2手术方式
该120例患者均在腹腔镜下完成下直肠癌根治术(直肠低位前切除),术中按全直肠系膜切除(total mesoretal excision,TME)原则进行直肠癌根治。A组在进行直肠双吻合“第一吻合”时,将直肠远端切割闭合,由水平方向改成垂直方向从而垂直切割闭合直肠远端(图1A)。圆形吻合器经肛门送入直肠远端,用超声刀切开直肠远侧闭合线上端角部(“狗耳”)尖端,中心杆由此切口伸出(图1B)与抵钉座连接后击发,完成肠-肠“端-角”吻合,从而去除该“狗耳”。闭合线的下端“狗耳”用血管夹夹闭(图1C)用3-0可吸收线加强缝合上述肠-肠“端-角”吻合后形成的一处钉合线“T”交汇处(“危险三角”),完成操作(图1D)。B组按常规直肠低位双吻合的操作方法,水平切割闭合直肠远端,中心杆从该闭合线中份旋出(避开钉合线,以免撕开直肠远侧断端闭合线),行肠-肠“端-端”吻合。双吻口处的两只“狗耳”及两处“危险三角”不作任何处理。
1.3统计学处理
所有资料应用SPSS 17.0软件进行统计学分析,计量资料正态分布采用t检验,偏态分布做秩和检验;计数资料采用χ2检验,P<0.05为差异有统计学意义。

图 1 腹腔镜下垂直切割闭合远端直肠、夹闭下“狗耳”、缝合“危险三角”Fig. 1 A novel approach for double stapling technique: laparoscopic vertical cutting of the closed distal rectum, remove the lower corner (“dog ear”), strengthen “dangerous triangle”
2 结 果
A组在垂直切割闭合直肠远端后,两只“狗耳”及一处“危险三角”处于上下位置,便于观察和处理。“端-角”吻合后肠管轴线形成一定交角,远端直肠腔形成类似“壶腹”样膨隆。无“狗耳”存在,一处“危险三角”较方便地予以缝合加强。B组完成“端-端”吻合后远近端肠管在同一轴线上,留有两只“狗耳”及两处“危险三角”。
两组均无死亡患者。对比A、B两组患者在性别、年龄、肿瘤位置、组织学类型、Dukes分期等临床一般资料差异无统计学意义(P>0.05,表1)。两组患者手术耗时[(211.18±90.55)min vs (173.82±57.43)min]差异有统计学意义、术后排便次数[(1.98±1.05)次 vs (2.65±1.08)次]差异有统计学意义(P=0.010,P=0.001)。术中出血量、术后引流量、肛门排气时间、住院时间两组差异无统计学意义(P>0.05,表2)。两组术后吻合口瘘的发生率(1.8% vs 12.3%,P=0.030)、里急后重(3.6% vs 13.8%,P=0.047)、术后再次手术造瘘(0 vs 10.7%,P=0.031)显著低于对照组,而术后吻合口出血两组差异无统计学意义(1.8% vs 4.6%,P=0.734,表3)。

表 1 A组与B组一般临床资料比较Tab. 1 Patient characteristics

表 2 两组患者术中术后情况比较Tab. 2 The comparison of the conditions of the patients from 2 groups after surgery(x±s)
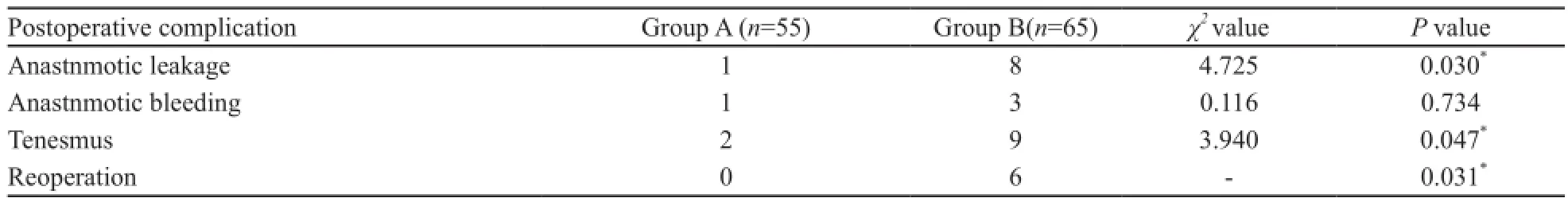
表 3 两组患者术后并发症情况比较Tab. 3 Postoperative outcomes
3 讨 论
“直肠低位双吻合技术”大幅提高了中低位直肠癌患者的保肛率[6],但术后吻合口瘘的发生率并无明显改善[7],原因除了目前公认的吻合口肠管血运、吻合口张力等种种因素外[8],观察常规双吻合口的结构和形态,笔者认为还可能与以下几点密切相关:①双吻合口留有直肠远侧闭合线两端的“狗耳”尖部。该处肠管在切割闭合后受压榨造成的组织损伤相对较重(肠管在此处折返重叠),所以“狗耳”尖部的组织结构相对较为薄弱。这可能是术后瘘的解剖及组织学基础。目前有对“狗耳”予以缝合加强的报道[9];也有将两角部用缝线拉入吻合器“钉仓”内进行肠-肠“端-端”吻合,使吻合后不留“狗耳”的研究[10]。但对“狗耳”的报道更多的是“憩室炎”方面的研究[11],其在直肠低位双吻合后发生瘘的解剖及组织学相关研究则很少。②双吻合后形成的两个钉合线“T”形交汇处。该处是隐性的组织缺如区,也是瘘的好发区。虽然已有不少学者注意到它的危险性[12],并有学者称其为“危险三角”,但只见到提及加强缝合吻合口的文献[13],并未见到针对这两个“危险三角”予以确切缝合加强的具体描述。③目前对于“直肠低位双吻合口发生瘘是不可避免的”观点,业内已达成共识。国内外瘘的发生率报道差别很大;这些是否与手术设计以及操作有某种因果关系有待进一步研究。④临床手术中,亦很少见到对这两个危险区域进行预防性处理的操作。就其原因有:对吻合器械的依赖,操作医师的自信或侥幸心理等,另一个重要原因是:在腹腔镜下对上述两个危险区域进行操作时,难度大,而且费时费力。
有研究认为,直肠低位前切除术后综合征的解剖基础是由于低位双吻合后的“狗耳”产生憩室效应[5],发生炎性反应,从而使患者术后出现肛门直肠的激惹症状,并影响术后直肠的储便及排便功能。术后患者会出现里急后重、排便次数增加等表现。因此,如果去除了“狗耳”,理论上对降低“直肠低位前切除术后综合征”有积极的作用。
综合上述理论和现实的原因,本研究设计了将常规双吻合的直肠远端切割闭合线由水平方向改为垂直方向,使两“狗耳”处于远侧直肠闭合线的上下端,从而方便了对“狗耳”的观察和操作。吻合器的中心杆由上端“狗耳”尖部穿出,行肠-肠“端-角”吻合后,直接去除了上端“狗耳”。同时由于该“端-角”吻合是在直肠远端闭合线的上端完成,使钉合线仅存一个“T”形交汇处(“危险三角”),从而降低了“危险三角”的个数。垂直方向切割闭合直肠远端使“危险三角”和下端“狗耳”在垂直线的上下位置,使显露、观察和操作较为方便。从而“危险三角”能予以确切加强缝合,下端“狗耳”可方便提起,血管夹夹闭。这样达到了加强“狗耳”及钉合线“T”形交汇处的组织薄弱点,同时消除了“狗耳”的憩室腔,为降低术后吻合口瘘及直肠低位前切除术后综合征的发生提供了组织及结构学基础。
本研究数据显示,A组患者瘘的发生、里急后重、排便次数明显优于B组。差异有统计学意义,显然与A组去除了“狗耳”并加强缝合了“危险三角”这些瘘的易发点相关。由于种种临床原因,术后出现了吻合口瘘,我们不能做肠镜或造影观察瘘口位置及状况,仅限于引流、冲洗或积极的临时造瘘改道进行对症处理(为了安全,本研究中虽不进行预防性回肠造瘘,但如一旦发生了吻合口瘘,即以积极干预为原则,这也是B组进行临时造瘘手术偏多的主要原因,A组中的1例吻合口瘘因在术后5 d时出现,且局部症状轻,故行保守治疗。虽然瘘的确切位置还不清楚,但去除这些双吻合口中的薄弱、危险区域,无疑是降低吻合口瘘的一个积极措施。本研究中手术耗时A组显著长于B组,确实与操作难度和操作量有关,但随着操作技术的熟练,操作流程的优化,手术耗时已逐渐缩短,因此未来在该操作的推广上不会受到手术耗时的明显限制。
A组“端-角”吻合完成后,近段肠管在远侧肠管闭合端的上后方,形成一定的前倾角,产生了类似直肠生理弯曲的走形;同时吻合口远侧直肠腔还形成一个类似“直肠壶腹”样的膨隆。这些对术后储便及排便功能会有什么影响,有待进一步研究。
[2]安靖如:《当代儒家政治哲学:进步儒学发凡》,韩华译,南昌:江西人民出版社,2015年,第193-198页。
值得一提的是,阴道直肠瘘本是直肠低位双吻合术后一种常见并发症,本组研究中并未出现,当然有可能与该组患者数较少有关外,更可能与操作者在腹腔镜下的确切辨认、精细分离有关,尤其重要的是,要求操作者进行肠-肠吻合时,必须在直视下确认吻合口内无阴道后壁等组织夹入后方可完成击发。本研究中将直肠远端水平切割闭合改为垂直切割闭合,由于骨盆的原因,使直肠远端闭合线呈15~20度左右的前倾,因此直肠前壁得到稍多保留,在对近切端组织行术中快速切片证实为阴性后,方可行肠-肠“端-角”吻合,否则需行直肠癌迈尔斯根治术。这也可能是本组即使是低位直肠吻合,亦未出现相关的阴道及前列腺相关并发症的原因。在保证切缘阴性的前提下,注意远端肠管尤其是其前壁的裸化和保留,近端肠管的张力和血运,肠-肠“端-角”吻合的确切可靠,是本手术成败的几个主要关键步续。
总之,本研究在腹腔镜下进行直肠低位双吻合时,垂直方向切割闭合直肠远端,对去除两个“狗耳”、减少吻合后“危险三角”的数目;方便术中对“危险三角”和下端“狗耳”的观察和操作,都起到积极作用。吻合后导致的肠管走行和形态更接近直肠的生理弯曲形态,其意义有待进一步研究观察。临床对照研究显示,本方法对降低直肠低位双吻合后并发症有较好的效果。
[参考文献]
[1] KNIGHT C D, GRIFFE F D. An improved technique for low anterior resection of the rectum using the EEA stapler[J]. Surgery, 1980, 88(5): 710-714.
[2] AKIYOSHI T, KUROYANAGI H, OYA M, et al. Factors affecting the difficulty of laparoscopic total mesorectal excision with double stapling technique anastomosis for low rectal cancer[J]. Surgery, 2009, 146(3): 483-489.
[3] AKIYOSHI T, UENO M, FUKUNAGA Y, et al. Incidence and risk factors for anastomotic leakage after laparoscopic anterior resection with intracorporeal rectal transection and doublestapling technique anastomosis for rectal cancer[J]. Am J Surg, 2011, 202(3): 259-264.
[4] ZIV Y, ZBAR A, BAR-SHAVIT Y, et al. Low anterior resection syndrome (LARS): cause and effect and reconstructive considerations[J]. Tech Coloproctol, 2013, 17(2): 151-162.
[5] ROMANISZYN M, RICHTER P, WALEGA P, et al. Lowanterior-resection syndrome. How does neoadjuvant radiotherapy and low resection of the rectum influence the function of anal sphincters in patients with rectal cancer? Preliminary results of a functional assessment study [J]. Pol Przegl Chi, 2012, 84(4): 177-183.
[6] 谈凯, 谢敏, 阮戈, 等. 双吻合器在低位直肠癌保肛手术中的临床应用[J].中国普通外科杂志, 2011, 20(9): 1002-1004.
[7] REILLY F, BURKE J P, APPELMANS E, et al. Incidence, risks and outcome of radiological leak following early contrast enema after anterior resection[J]. Int J Colorectal Dis, 2014, 29(4): 453-458.
[8] YANG L, HUANG X E, ZHOU J N. Risk assessment on anastomotic leakage after rectal cancer surgery: an analysis of 753 patients [J]. Asian Pac J Cancer Prev, 2013, 14(7): 4447-4453.
[9] BAEK S J, KIM J, KWAK J, et al. Can trans-anal reinforcing sutures after double stapling in lower anterior resection reduce the need for a temporary diverting ostomy?[J]. World J Gastroenterol, 2013, 19(32): 5309-5313.
[10] KANG J, LEE H B, CHA J H, et al. Feasibility and impact on surgical outcomes of modified double-stapling technique for patients undergoing laparoscopic anterior resection [J]. J Gastrointest Surg, 2013, 17(4): 771-775.
[11] TSUBAKI M, ITO Y, FUJITA M, et al. Use of the modified double-stapling technique with vertical division of the rectum during a sphincter-preserving operation for the treatment of a rectal tumor [J]. Asian J Surg, 2012, 35(3): 110-112.
[12] KIM H J, CHOI G S, PARK J S, et al. Comparison of intracorporeal single-stapled and double-stapled anastomosis in laparoscopic low anterior resection for rectal cancer: a casecontrol study [J]. Int J Colorectal Dis, 2013, 28(1): 149-156.
[13] DAUSER B, BRAUNSCHMID T, GHAFFARI S, et al. Anastomotic leakage after low anterior resection for rectal cancer: comparison of stapled versus compression anastomosis[J]. Langenbecks Arch Surg, 2013, 398(7): 957-964.
DOI:10.3969/j.issn.1007-3969.2014.11.006
中图分类号:R735.3+7
文献标志码:A
文章编号:1007-3639(2014)11-0830-06
收稿日期:(2014-07-17 修回日期:2014-09-19)
通信作者:吴云云E-mail:doctorwuyunyun@163.com
The significance and role of laparoscopic vertical cutting of the closed distal rectum in dualanastomosis for patients with low rectal cancer
CHEN Shao-ji1, WU Yun-yun2, HAN Shan-liang1, MO
Qin-liang1, MA Yuan-ming1, ZHAO Hong1(1. Department of General Surgery, the First Af fi liated Hospital of Soochow University, Suzhou Jiangsu 215000, China; 2. Department of Surgery, The First People’s Hospital of Wujiang District, Suzhou Jiangsu 215000, China)
Correspondence to: WU Yun-yun E-mail: doctorwuyunyun@163.com
[Abstract]Background and purpose: Anastomotic leakage and low anterior resection syndrome(LARS) are both common complications in dual-anastomosis for patients with low rectal cancer. The aim of this study was to observe and explore the signi fi cance and role of vertical cutting of the closed distal rectum in dual-anastomosis for patients with low rectal cancer. Methods: A total number of 120 patients with mid-low rectal cancer who admitted to and completed laparoscopic rectal cancer resection in the Department of General Surgery, the First Af fi liated Hospital of Soochow University from Feb. 2010 to Jun. 2014 were pair-matched into Groups A and B based on their gender,age, tumor size, the distance of lower edge to the dentate line and tumor staging, etc. For the 55 patients in Group A (observation group), the rectum distal end was closed vertically instead of horizontally while disposing “the fi rst intestinal anastomosis”, intestine-intestine anastomosis was conducted in an “end-corner” approach when dealing with“the second intestinal anastomosis”, upper corner (“dog ear”) of the closed line in the distal end of the rectum was removed, the lower corner (“dog ear”) of the closed line in the distal end of the rectum was removed using vascular occlusion clamp method, and the T-shaped interchanges (“dangerous triangle”) of stapled sutures formed after anastomosis were strengthened with absorbable suture. For the 65 patients in Group B (control group), laparoscopic dual anastomosis was conducted using conventional method, and the two “dog-ears” and “dangerous triangles”were kept without any treatment. The clinical outcomes of the two groups of patients were analyzed retrospectively. Results: In group A, It was convenient to complete the operation when the “dog ears” and “dangerous triangle” on the vertical line after cutting the closed distal rectum vertically by “end-corner” anastomosis. The axis of intestine formed a certain angle making the closed distal rectum into “ampulla” sample without “dog ears”. the “dangerous triangle”were strengthened with absorbable suture. In group B, The distal and proximal intestine located on the same axis after intestine-intestine anastomosis leaving two “dog ears” and a “dangerous triangle”. The general clinical data of patients in the two groups were comparable and not signi fi cantly different (P>0.05). The two groups of patients showed no signi fi cant differences in blood loss, postoperative drainage, postoperative anastomotic bleeding, anal exhaust time, and length of hospital stay (P>0.05). However, the operation time as well as the numbers of anastomotic fi stula occurrence, defecation, tenesmus and post-operation re-ostomy differed significantly (P<0.05). Conclusion: Vertical cutting of the closed distal rectum with dual anastomosis made the “new” intestine closer to the physiological bending and morphology of the rectum, meanwhile, it simpli fi ed the approach of removing “dog ear” and strengthening “dangerous triangle”, fi nally it signi fi cantly reduced the incidence of post-surgical complications.
[Key words]Mid-low rectal cancer; Dual anastomosis for low rectal cancer; Vertical cutting of the closed distal rectum; Post-operation complications