Acute brucellosis as unusual cause of immune thrombocytopenia: a case report and review of the literature
Tajeldin Mohammedien Abdallah, Omer Mohammed Abd elbagi, Abuelgasim OsmanKaroum, Abdel Aziem Abdallah Ali
1Department of Medicine, Faculty of Medicine, Kassala University, Kassala, Sudan
2Faculty of Medicine, Gezira University, Wad Medani, Sudan
Acute brucellosis as unusual cause of immune thrombocytopenia: a case report and review of the literature
Tajeldin Mohammedien Abdallah1*, Omer Mohammed Abd elbagi2, Abuelgasim OsmanKaroum1, Abdel Aziem Abdallah Ali1
1Department of Medicine, Faculty of Medicine, Kassala University, Kassala, Sudan
2Faculty of Medicine, Gezira University, Wad Medani, Sudan
PEER REVIEW
Peer reviewer
Dr. Mamoun Magzoub Mohamed, PhD, Assistant Professor Department of Microbiology and Parasitology, Faculty of Medicine, (West Bank of Gash River) University of Kassala, Kassala, Sudan. Fax: 00249411823501
Tel: 00249912913999
E-mail: mosmanmm@hotmail.com
Comments
This is the an interesting case of brucellosis as unusual cause of immune thrombocytopenia, the interesting observation the patient did not respond to the treatment of brucellosis firstly and later diagnosed as immune thrombocytopenia then after treating with prednisolone, platelet count rose, epistaxis and gingival bleeding were subsided. The study explained that brucellosis is the possible cause of immune thrombocytopenia.
Details on Page 753
A 25 year-old male patient was admitted to the causality with complaints of fever, joints pain, epistaxis and gingival bleeding, for the last week, the complete blood count revealed pancytopenia. Serological test for brucella was reported positive as 1/320, but the patient failed to respond to brucella treatment for 4 d. On day 5th the diagnosis of immune thrombocytopenia was confirmed after bone marrow aspiration. Steroid was initiated on 6th day after admission and on the 3rd day of steroid therapy thrombocytes count was raised to 55×109/L and came up to 180×109/L on 12th day after admission. Brucella-induced immune thrombocytopenia should be considered in patient presenting with bleeding and febrile illness especially in endemic region.
Brucella, Thrombocytopenia, Tone marrow
1. Introduction
Brucellosis is a zoonotic disease caused by coccobacilli of the genusBrucellaand transmitted to the human through ingestion of animal products such as raw milk, cheese, meat, or through direct contact with infected animals, or animal excreta[1,2]. It has been estimated that 500 000 new cases of brucellosis reported each year worldwide[3]. The vast majority of reported cases were from Mediterranean and Middle East regions[4]. Brucella is endemic in the Sudan and the prevalence of the disease ranging between 8.9%-18%[5,6].Brucella melitensisis the most virulent form of the disease with wide range of clinical manifestations and multi organ affection[2,7]. Although Anemia and leukopeniaare the most common hematological complications of acute Brucellosis, immune-mediated thrombocytopenia, pancytopenia and disseminated intravascular coagulation have been occasionally reported[6-9]. Thrombocytopenia in acute brucellosis might be attributable to bone marrow suppression, hypersplenism and immune mechanism[8,10]. Here by we presented patient with the history of fever, bleeding manifestations (epistaxis, gingival bleeding and hematurea) and pancytopenia. The patient was initially diagnosed as acute brucellosis and started doxycycline and refampicin, but no repose achieved, on day 5th after admission the bone aspiration support a diagnosis of immune thrombocytopenia.
2. Case report
A 25 year-old shepherd male patient was brought to the emergency room at Kassala teaching hospital with complaints of epistaxis, gingival bleeding and fever which is intermittent in nature associated with rigor and drenching sweating for the last week, he had no history of bleeding from other site and he denied any family history of bleeding disorders, but he had history of joint pain, weight loss and headache. The latter symptoms had begun two weeks prior to admission. He had been diagnosed as malaria two weeks previously and treated with artemether injection and paracetamol tablets. On arrival to the causality he was ill febrile with body temperature of 39 °C, arterial blood pressure 100/70 mmHg, heart rate 94/min, and respiratory rate 16/min, slightly pale. His physical examinations regarding the cardiovascular, respiratory and central nervous systems were normal, his abdominal examination revealed hepato- s plenomegaly.
Complete blood count revealed Hb 10.1 g/dL, WBCs 3.100/μL with 62% polymorphs, 29% lymphocytes, and 9% monocytes, platelet 10×109/L, prothrombin time, activated partial thromboplastin time were normal, renal and liver function tests were normal, HBsAg and HCAbs were negative, standard tube agglutination test was reported as 1:320 forBrucella melitensis, widal for enteric fever, screening for dengue infection and blood film for malaria were negatives. Peripheral blood picture showed giant platelets, the patient received one units of fresh blood and two unit of platelet on the first and the second days of his admission. On day second after admission the patient commented on doxycycline, streptomycin in spite of that the patient still having epistaxis and gingival bleeding and the platelets came down to 8×109/L. On day 4th after admission, the patient transfused with two units of platelets, on day five, bone marrow aspiration was performed which revealed hyper cellular with increased megakaryocyte(Figures 1 and 2) which is highly suggestive of immune thrombocytopenia, then prednisolone tablets 50 mg daily was commenced on day 6th, on day 8th the platelet count rose to 55×109/ L, epistaxis and gingival bleeding were subsided and the patient discharged on day 12th in a good condition with the platelet count of 180×109/L and advised to continue anti brucella for 6 weeks. On the first visit (day 30th) after discharge the patient was quite healthy; splenomegaly and hepatomegaly were not detected clinically and the platelet increased to 250×109. The regular follow up of the patient till 6th month after discharge showed no evidence of relapse or hematological abnormalities.

Figure 1. Active marrow with increased megakaryocytes (Arrows).
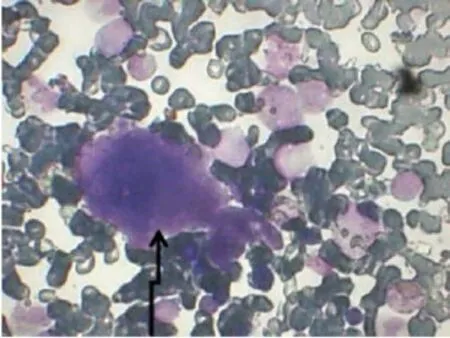
Figure 2. Active megakaryocytes.
3. Discussion
Human brucellosis is a systemic disease with wide clinicalpresentation, brucellosis constitutes to be a major health problem in the developing countries including Sudan[5]. Hematological complications of brucellosis have been documented and they were ranging between mild anemia, leucopenia, disseminated intravascular coagulation, pancytopenia and severe thrombocytopenia[8,9]. Brucellaassociated thrombocytopenia might be attributable to hypersplenism, bone marrow suppression, granuloma in the bone marrow, hemophagcytosis, disseminated intravascular coagulation and immune mediated thrombocytopenia[8,11-13]. The frequency of isolated thrombocytopenia was observed in 2.6% of patients with active brucellosis[14]. Although the study case was initially diagnosed as brucellosis, thrombocytopenia and epistaxis did not respond to antibiotics (refampicin and doxycycline) for 5 d, however the bleeding manifestations resolved and thrombocytes count increased to 55×109/L within 3 d after commencement of prednisolone at a dose of 1 mg/kg/d. The rapid response to steroid observed in the study case supports the diagnosis of Brucella-associated immune mediated thrombocytopenia, Similar to our case Tunccanet al.presented a case of a patient with epistaxis and severe thrombocytopenia who responded to steroid therapy[12]. By contrast EL-mas Dalet alreported a case with thrombocytes count of 4×109/L who diagnosed as immune thrombocytopenia associated with Brucellosis, that did not show any response to steroid[15], the difference between this case and the presented patient may be due to implication of other factors such as socio-demographic characteristics and mode of clinical presentation. The presence of splenomegaly and hematological findings(pancytopenia) firstly raise the possibility of hypersplenism, however the result obtained from the bone marrow aspiration as well as resolution of thrombocytopenia after the administration of steroid are consistent with immune-mediated thrombocytopenia. Moreover the hematological abnormalities reverted to normal level earlier than the resolution of splenomegaly, thus hypersplenism was unlikely to be implicated as the cause of pancytopenia in our patient. Furthermore leukopenia and anemia have been frequently encountered in patients with acute brucellosis[16]. Immune-induced Thrombocytes destruction can be caused by anti-platelets antibodies, however negatives assay for anti-platelets does not ruled out the presence of immune thrombocytopenia[10]. Epistaxis and gingival bleeding are the main hemorrhagic manifestations in the presented patient, similarly Younget al.have reviewed a total of 41 patient with Brucella -induced thrombocytopenia and reported principal sites for mucosal bleeding as epistaxis 64%, gigivorrhea 44% and hematurea 64%[17].Brucella melitensis-induced Hemorrhagic manifestations detected in our patient was documented earlier by Citaket al[18]. In our experience of patient with brucellosis, hemorrhagic features are unexpected for acute brucellosis, therefore other differential diagnosis such as Dengue hemorrhagic fever, severe malaria and enteric fever, have been considered in the differential diagnosis. The diagnosis of brucellosis was made according to the patient’s history (occupational hazard), physical findings and the result of serological tests (agglutination test). Anti-platelets antibodies, bone marrow culture and blood culture were not obtained because they are not available in the study area.
4. Conclusion
The diagnosis of immune thrombocytopenia should be considered among patient with brucellosis who presented with severe thrombocytopenia and did not respond to antibrucellosis treatment. Starting steroid therapy is the main stay in the treatment of bleeding due to Brucella inducedthrombocytopenia.
Conflict of interest statement
We declare that we have no conflict of interest.
Acknowledgements
We are very grateful to Dr. Amna Saadook and Dr. Mohammed Eisa for their assistance. This work was financially supported by Kassala University, Sudan, and the Grant No provided as, K-U-2014-1.
Comments
Background
The back ground of the research brucellosis is a multisystem disease with a broad spectrum of clinical manifestations.Brucella melitensisis the most virulent form of the disease with wide range of clinical manifestations and multi organ affection. Haematological abnormalities including anemia, leucopenia, thrombocytopenia and pancytopenia can be encountered during the course of the disease.
Research frontiers
The cutting-edge in the field of the research in this paper This case report revealed brucellosis is the unexpected cause of immune thrombocytopenia which commonly is not considered for most physicians.
Related reports
This is the an interesting case of brucellosis with immune thrombocytopenia, the interesting observation the patient did not respond to the treatment of brucellosis firsly and later diagnosed as immune thrombocytopenia so physician should consider immune thrombocytopenia and its treatment should be administered.
Innovations and breakthroughs
Immune thrombocytopenia associated with brucellosis has been rarely reported in the world literature. This study showed that brucellosis is the one cause of immune thrombocytopenia.
Applications
From the literature anemia and leucopenia are the most common hematological complications of acute brucellosis. But immune-mediated thrombocytopenia, has been occasionally reported.
Peer review
This is the an interesting case of brucellosis as unusual cause of immune thrombocytopenia, the interesting observation the patient did not respond to the treatment of brucellosis firstly and later diagnosed as immune thrombocytopenia then after treating with prednisolone, platelet count rose, epistaxis and gingival bleeding were subsided. The study explained that brucellosis is the possible cause of immune thrombocytopenia.
[1] Ariza J, Bosilkovski M, Cascio A, Colmenero JD, Corbel MJ, Falagas ME, et al. Perspectives for the treatment of brucellosis in the 21st century: the Ioannina recommendations. PLoS Med 2007; 4(12): e317.
[2] Pappas G, Akritidis N, Bosilkovski M, Tsianos E. Brucellosis. N Engl J MED 2005; 352(22): 2325-2336.
[3] Atluri VL, Xavier MN, de Jong MF, den Hartigh AB, Tsolis RM. Interactions of the human pathogenic Brucella species with their hosts. Annu Rev Microbiol 2011; 65: 523-541.
[4] Lopes LB, Nicolino R, Haddad JPA. Brucellosis-risk factors and prevalence: a review. Open Vet Sci J 2010; 4: 72-84.
[5] Mustafa AAA, Hassan SH. Human brucellosis in Khartoum State: a commonly underdiagnosed disease. Sudan JMS 2010; 5(3): 213-216.
[6] Musa MT, Shigidi MT, Saeed OM. Brucellosis in humans associated with animals. Saudi Med J 1999; 20(4): 311-315.
[7] Cornner MM, Ebinger MR, Blanchong JA, Cross BC. Infectious disease in cervids of North America: data, models, and management challenges. Ann N Y Acad Sci 2008; 1134: 146-172.
[8] Erkurt MA, Sari I, Gul HC, Coskun O, Eyigun CP, Beyan C. The first documented case of brucellosis manifested with pancytopenia and capillary leak syndrome. Intern Med 2008; 47(9): 863-865.
[9] Yilmaz M, Tiryaki O, Namiduru M, Okan V, Oguz A, Buyukhatipoglu H, et al. Brucellosis-induced immune thrombocytopenia mimicking ITP: a report of seven cases. Int J Lab Hematol 2007; 29(6): 442-445.
[10] Pappas G, Kitsanou M, Christou L, Tsianos E. Immune thrombocytopenia attributed to brucellosis and other mechanisms of brucella-induced thrombo-cytopenia. Am J Hematol 2004; 75(3): 139-141.
[11] Demir C, Karahocagil MK, Esen R, Atmaca M, Gönüllü H, Akdeniz H. Bone marrow biopsy findings in brucellosis patients with hematologic abnormalities. Chin Med J (Engl) 2012; 125(11): 1871-1876.
[12] Tunccan OG, Dizbay M, Senol E, Aki Z, Ozdemir K. Isolated severe immune thrombocytopenia due to acute brucellosis. Indian J Hematol Blood Transfus 2013; doi: 10.1007/s12288-012-0222-3.
[13] Erduran E, Makuloglu M, Mutlu M. A rare hematological manifestations of brucellosis reactive haemophagocytic syndrome. J Microbiol Immunol Infect 2010; 43(2): 159-162.
[14] Akbayram S, Dogan M, Akgun C, Peker E, Parlak M, Oner AF. An analysis of children with brucellosis associated with isolated thrombocytopenia. Clin Appl Thromb Hemost 2011; 17(6): E36-8.
[15] Elmas Dal S, Ersoy Y, Ali Erkurt M, Yetkin F, Kuzucu C, Akdogan O. An uncommon case of acute brucellosis presenting with severe thrombocytopenia. Intern Med 2012; 51(23): 3291-3293.
[16] El-Koumi MA, Afify M, Al-Zahrani SH. A prospective study of brucellosis in children: relative frequency of pancytopenia. Mediterr J Hematol Infect Dis 2013; 5(1): e2013011.
[17] Young EJ, Tarry A, Genta RM, Ayden N, Gotuzzo E. Thrombocytopenic purpura associated with brucellosis: report of 2 cases and literature review. Clin Infect Dis 2000; 31(4): 904-909.
[18] Citak EC, Citak FE, Tanyeri B, Arman D. Hematologic manifestations of brucellosis in children: 5 years experience of an anatolian center. J Pediatr Hematol Oncol 2010; 32(2): 137-140.
10.12980/APJTB.4.2014C1324
*Corresponding author: Tajeldin M. Abdallah, Department of Medicine, Faculty of Medicine, Kassala University, Kassala, Sudan.
Tel: +249912820929
Fax: +249411823501
E-mail: tajeldinmm@yahoo.com
Foundation Project: Supported by Kassala University, Sudan, and the Grant No provided as, K-U-2014-1.
Article history:
Received 25 Dec 2013
Received in revised form 13 Jan, 2nd revised form 27 Feb, 3rd revised form 16 Mar 2014
Accepted 23 May 2014
Available online 3 Sep 2014
 Asian Pacific Journal of Tropical Biomedicine2014年9期
Asian Pacific Journal of Tropical Biomedicine2014年9期
- Asian Pacific Journal of Tropical Biomedicine的其它文章
- A case report of cutaneous larva migrans in a Mexican population of high marginalization
- Chemical composition and larvicidal activity of essential oil of Origanum majorana (Lamiaceae) cultivated in Morocco against Culex pipiens (Diptera: Culicidae)
- Hematological and serum biochemical aspects associated with a camel (Camelus dromedarius) naturally infected by Trypanosoma evansi with severe parasitemia in Semnan, Iran
- Phytochemical screening and antioxidant activity of ethanol extract of Tithonia diversifolia (Hemsl) A. Gray dry flowers
- Rate of carcass and offal condemnation in animals slaughtered at Yazd Slaughterhouse, central Iran
- Formulation and evaluation of novel stomach specific floating microspheres bearing famotidine for treatment of gastric ulcer and their radiographic study
