人工关节假体重建肘部肿瘤切除后骨缺损
郭卫 汤小东
通讯作者:郭卫,Email:bonetumor@163.com
【摘要】目的肘关节周围肿瘤切除后骨缺损的重建较为困难。本文回顾在肘关节周围肿瘤切除术后行全肘关节成型假体重建的病例,明确这种手术的疗效、功能及并发症。方法1998年至2010年,共有24例高度或低度恶性肿瘤患者在北京大学人民医院接受了肿瘤切除后全肘关节置换术,其中男性14例,女性10例;平均年龄42.6岁。病理诊断:骨肉瘤6例,尤文肉瘤4例,恶性纤维组织细胞瘤3例,骨巨细胞瘤2例,淋巴瘤、滑膜肉瘤、骨的硬纤维瘤各1例,转移癌6例。肿瘤累及肱骨远端12例,累及尺骨近端7例,肱骨远端及尺骨近端均受累5例。骨缺损重建采用定制型绞链式人工肘关节。术后鼓励患者主动活动手部,肘关节制动至伤口愈合后。切除标本进行病理分析确定外科边界,15例广泛切除,9例边缘性切除。对所有患者进行规律随访,记录生存、转移、复发、功能及假体并发症情况。采用Mayo肘关节功能评分(Mayo elbow performance scorce,MEPS)及肌肉骨骼肿瘤协会(MSTS)功能评分系统评估患者的术后功能。结果1例患者失随访,其余23例患者均至少随访1年或随访至死亡(平均随访37个月)。在随访期间,11例患者无瘤生存;4例转移癌、1例骨肉瘤及1例尤文肉瘤患者分别死于术后2年内;2例尤文肉瘤、1例恶性纤维组织细胞瘤、1例骨肉瘤发生肺转移以及2例转移瘤患者带瘤生存。6例骨肉瘤中,失随访、死亡、肺转移带瘤生存各1例,其余3例无瘤存活;4例尤文肉瘤中,1例死于肿瘤转移,2例肺转移带瘤生存,其余1例无瘤存活。肿瘤局部复发3例(13%)。6例患者出现并发症,发生率26.1%,包括桡神经牵拉伤1例,伤口不愈合2例,无菌性松动及假体柄穿出骨皮质共3例。术后MSTS评分:5例关节外肿瘤切除患者平均25分,18例关节内切除患者平均25.9分。MEPS评分平均80分。肘关节的平均屈伸范围73°(范围:55°~105°)。结论肘部肿瘤切除、人工关节假体重建术可以提供良好的肿瘤学检查结果,并发症发生率较低,术后功能恢复良好。
【关键词】 人工肘关节; 成形术; 肿瘤; 保肢
【Abstract】BackgroundThe tumors at the elbow bone account for 1% of the bone tumors of the whole body. Lymphoma is the most common malignant tumor and osteoid osteomais is the most common benign tumor. In the past, the treatment of elbow malignant tumors is amputation, which results in loss of limb after surgery. With the development of surgery and the technology of radiation and chemotherapy, it is possible to partially excise the tumors and retain upper limbs. However, due to the important anatomical structures of elbow, partial excision of tumor leads to instability and poor function of the joint of elbow, wrist and hand. Before the total endoprosthesis of elbow appeared, there were only several reconstruction methods to rebuild stable functional elbow after tumor resection. Arthrodesis or excisional arthroplasty of the elbow has their respective disadvantage:arthrodesis results in limited elbow motion, and excisional arthroplasty results in joint instability. At present, there are rare literatures guiding the elbow reconstruction after the tumor resection. Therefore, This study presented our results of limb salvage surgery using custom-made prostheses for reconstruction of the elbow after tumor excision. The oncologic results, complications, and functional outcomes were further discussed.Methods(1)General information:The elbow tumor surgery cases from June 1998 to June 2010 were retrospectively collected in Peking University People′s Hospital. The inclusion criteria were as follows:malignant tumor involving the proximal ulna and distal humerus or benign invasive tumor, tumor excision with prostheses for reconstruction of the elbow. The benign tumors, revision and complete humerus surgery patients should be ruled out.There are 24 patients in this study,14 men and 10 women, with a mean age of 42.6 year-old. Pathological diagnosis of these cases were:6 cases of osteosarcoma,4 cases of Ewing′s sarcoma,3 cases of malignant fibrous histiocytoma,2 cases of giant cell tumor, each 1 case of lymphoma, synovial sarcoma and bone of desmoid tumor,6 cases of metastatic carcinoma (3 cases of lung cancer, and each 1 case of melanoma, ovarian cancer and rectal cancer). 12 tumors were in distal humerus, 7 in proximal ulna, 5 in humerus and 5 in ulna. Patients with osteosarcoma, Ewing′s sarcoma and malignant lymphoma received standard chemotherapy preoperatively and postoperatively. Malignant fibrous histiocytoma and lymphoma patients received radiotherapy postoperatively.(2)Prosthesis design Patients underwent reconstruction of elbow joint with custom-made hinged type artificial elbow endoprosthetic (ChunLiZhengDa medical equipment company, Beijing, China). In order to increase the fixation effect of the bone cement, all prostheses were cement type and ulna prosthesis handles were screw type. In order to strengthen the stability, the surface of the prosthesis that contact with proximal humerus and distal ulna were coated by titanium paste or made of granular surface coating. Due to the smaller diameter of ulnar canal and curved shape, the ulnar prosthetic handle diameter was 6 to 7 mm, and length was about 6 to 8 cm.(3)Surgical technique:The elbow posterior approach was commonly used. All of the patients underwent en-bloc resection, 5 patients underwent the joint resection for their tumors were involved in the articular cavity, the remaining cases received intra-articular resection. Those patients with distal humerus tumors needed to reflect the triceps muscle. If possible, we tried to keep the ulna olecranon and triceps tendon attachment points. After removal of the tumor, we repaired to the greatest extent the forearm flexion and extension as well as pronation after spin muscle group attachment points. For cases of proximal ulna, we kept humerus medial condyle and lateral condyle as much as possible, embedding the humerus part of prosthesis into the fossa intercondyloidea. When installing the joints, humerus and ulna part of prosthesis were fixed in the medullary cavity with bone cement, respectively, and then the hinge was connected. The average operation time of the patients was about 120 min, the mean volume of blood loss was 400 ml, and the average time for the use of tourniquet was 80 min.(4)Postoperative recovery and follow-up:Active hand movement was encouraged after operation. Elbow joint cannot be moved until the wound healed. Pathological analysis of the resection specimen was conducted to determine the surgical boundary. 15 cases received wide resection, and 9 cases received borderline resection. Regular follow-up was performed for all patients to record the situation of survival, metastasis, recurrence, function and implant complications. The scoring systems of Mayo elbow joint function (MEPS) and MSTS joint function were used to assess the patient′s postoperative function.ResultsOne patient was lost to follow up, the rest 23 patients were followed up for at least one year or until to death (mean,37 months). During the follow-up,11 patients were tumor-free survivals. 4 with metastatic carcinoma, one with osteosarcoma and one with Ewing′s sarcoma died within two years after the operation, respectively. Two cases of Ewing′s sarcoma, one of malignant fibrous histiocytoma, one of osteosarcoma with lung metastasis, and two of metastatic tumor, survived with tumor. Among the 6 patients with osteosarcoma, one lost to follow up, one died and one survived with lung metastasis, the other three were tumor-free survivals. In the 4 cases of Ewing′s sarcoma, one patient died of tumor metastasis, two survived with lung metastasis, and one was tumor-free survival.Tumors recurred locally in 3 cases (13%).The incidence of complication was 26.1% (6/23), including one patient with pull injury of radial nerve that recovered during the 6 months after operation. The wound was difficult to heal in 2 cases, and cured after debridement. Among 3 patients suffering implant complications,2 patients′ prosthesis handle pricked the bone cortex and one patient′s prosthesis was aseptic loose. These three obtained good function after the operation of prosthesis revision.Postoperative MSTS score were as follows:the score of 5 cases with the whole tumor resection outside the joint and artificial elbow joint replacement was 25 points on average, the mean score of 18 cases with tumor resection inside the joint and artificial elbow joint replacement was 25.9 points.The operation effects of 18 cases were satisfactory (18/23,78.3%) and 5 cases were acceptable (5/23,21.7%). The average MEPS score of all the patients was 80 points. The mean flexion range of elbow was improved from 29 ° to 73 ° (range, 55 °-105 °).DiscussionExcisional arthroplasty or arthrodesis of the elbow always leads to poor function and is difficult for patients with bone loss. The options for reconstruction after excision of the tumor around the elbow are technically difficult and limited. This study presented our results of limb salvage surgery using custom-made prostheses for reconstruction of the elbow after tumor excision, and discussed the oncologic results, complications, and functional outcome.(1)The requirements of prosthesis and the patient in total elbow arthroplasty.The means of limb salvage and application of elbow prosthesis after the tumor resection have rarely been reported before. For total elbow arthroplasty for reconstruction of the elbow, prosthesis and the patient must meet certain requirements. Prosthesis should allow the steady activity of the forearm and hand, its length can make up the bone defects, and its mechanical strength can withstand everyday use. In addition, the prosthesis must be technically easy to install, and ensure stable fixation. In terms of the choice of cases, total elbow arthroplasty can be only applied to the patients with the functional neurovascular bundle, forearm and hand. The total elbow arthroplasty can not be used for the patients, who can be curative after tumor resection, but need to sacrifice margin to secure the implant. The treatment of patients with extensive tumor metastasis and poor prognosis, such as tumor resection, implant replacement surgery, chemotherapy or radiotherapy, need to be performed based on their own conditions. Furthermore, in such case, amputation should be avoided to retain the function of their hand and forearm.(2) Elbow reconstruction after tumor resection.Not many reconstruction methods are reported to rebuild a stable elbow after tumor resection. Arthrodesis or resection arthroplasty is often used for smaller bone defects. Arthrodesis results in limited postoperative elbow movement, and resection arthroplasty leads to postoperative joint instability. The allogeneic elbow transplantation has been applied for the larger defects. Semi-allogeneic transplant articular can make soft tissue attachment to retain muscle function and maintain joint stability, but the rate of postoperative complications can be as high as 70%. Infection, joint instability and dislocation often occur after surgery. Despite the solid internal fixation exists, postoperative bone nonunion occurred frequently ( about 15% ). The other patients may had allogeneic bone resorption. The results of this study showed that the implementation of the whole elbow after tumor resection arthroplasty could significantly reduce the pain and improve the function. Patients with metastases may be treated by this surgical method, especially for whose symptoms can not be relieved by other methods. There is no better method than the artificial elbow replacement for the functional reconstruction after resection of the tumor around the elbow joint. And the incidence of complications after elbow arthroplasty is acceptable.(3)Ensure the success of total elbow arthroplasty:Following points should be noted:①The principles of malignancy wide excision should be followed, otherwise local tumor recurrence might easily appear. ②Soft tissue coverage should be sufficient to avoid incision problems, which could lead to failure of the prosthesis replacement surgery. ③Patients with the tumor of distal humerus should be treated, after removal of the tumor, by the repair of the forearm flexion and extension as well as pronation after spin muscle group start and end points. If possible, partial medial and lateral condyle of humerus should be maintained as far as possible. ④Due to the smaller ulnar canal and less bone cement poured, the intramedullary prosthesis should be designed as the coarse thread type, which helps to cement to prevent the prosthesis rotation and loosening. ⑤For the smaller diameter of ulnar canal and curved shape, the ulnar prosthetic handle must not be too long, with 5-7 cm advisable, otherwise it will be easy to wear a bone cortex; ⑥The medial and lateral condyle of humerus should be kept for patients with the tumor of proximal ulna. And the humerus part of prosthesis between fossa intercondyloidea should be embedded. (4)Function evaluation:All the three groups of patients started functional exercise after the postoperative 3 weeks. After 8 weeks, 70% of patients had a "near normal"-like appearance with the elbow flexion range between 50 degrees to 90 degrees, 5% of patients with an arc of motion of less than 50 degrees,25% of patients with an elbow flexion range of greater than 90 degrees. 90% of the patients could make movements of their elbows without pain; 80% of patients retained the function of the forearm rotation.ConclusionsIn conclusion, local tumor resection together with prosthetic reconstruction of the elbow can provide good surgical outcomes and less complication with oncologic safety for the appropriate patients.
【Keywords】 Endoprosthesis of elbow; Arthroplasty; Neoplasm; Limb salvage
肘部骨肿瘤占全身骨肿瘤发病率的1%。其中,淋巴瘤是最常见的恶性肿瘤,骨样骨瘤是最常见的良性肿瘤[1]。在过去,治疗肘部恶性肿瘤多需要截肢,造成术后肢体功能丧失。随着外科及放化疗技术的进展,使得局部切除肿瘤、保留上肢成为可能。然而,由于肘部重要的解剖结构密集,肿瘤局部切除术后会导致肘、腕及手部关节不稳定、功能丧失。在人工全肘关节出现以前,肿瘤切除术后要重建功能稳定的肘关节,仅有为数不多的几种重建方法可供选择[1-3]。关节融合术或切除成形术各自存在弊端:关节融合术导致肘关节运动受限,切除成形术导致关节不稳定。目前,指导肿瘤切除后的全肘关节重建方面的文献甚少。为此,我们对肘关节周围肿瘤切除术后人工肘关节置换术患者的临床资料进行回顾性分析,以探讨这种手术的疗效、并发症及术后功能。
材料和方法
一、一般资料
回顾性收集1998年6月至2010年6月在北京大学人民医院接受肘部肿瘤手术的病例资料。纳入标准:累及尺骨近端及肱骨远端的恶性或良性侵袭性肿瘤;接受肿瘤切除全肘人工关节假体重建。良性肿瘤、接受翻修及全肱骨手术的患者被排除。共有24例患者纳入研究,其中男性14例,女性10例;年龄15~71岁,平均42.6岁;病理诊断:骨肉瘤6例,尤文肉瘤4例,恶性纤维组织细胞瘤3例,骨巨细胞瘤2例,淋巴瘤、滑膜肉瘤、骨的硬纤维瘤各1例,转移癌6例(肺癌3例,黑色素瘤、卵巢癌、直肠癌各1例);累及部位包括肱骨远端12例,尺骨近端7例,肱骨远端及尺骨近端均受累5例。术前术后,骨肉瘤、尤文肉瘤及恶性淋巴瘤病例均接受规范化疗;恶性纤维组织细胞瘤及淋巴瘤病例均进行了术后放疗。
二、假体设计
患者使用研究者设计的定制型绞链式人工肘关节(春立正达医疗器械公司,中国北京)进行重建,所有假体均为骨水泥固定型,尺骨假体柄为螺纹式,以增加骨水泥固定效果。为了加强稳定性,假体近端肱骨及远端尺骨与骨接触部分表面喷涂钛浆涂层或制成粒状表面。由于尺骨髓腔直径较小、形状弯曲,因而尺骨髓腔内的假体柄直径一般为6~7 mm,长度约6~8 cm。
三、手术技术
常规采用肘关节后侧入路。本组病例均行整块切除,其中5例患者因肿瘤累及关节腔,采用关节外切除(图1,2),其余病例采取关节内切除。对于肱骨远端肿瘤病例,需形成肱三头肌肌瓣,如可能,应尽量保留尺骨鹰嘴及肱三头肌肌腱止点,切除肿瘤后,尽量修复前臂屈伸及旋前旋后肌群的起止点;对于尺骨近端病例,尽量保留肱骨内外侧髁,将肱骨部分假体嵌入髁间窝部位。关节安装时,先将假体肱骨及尺骨部分分别采用骨水泥固定于髓腔,而后连接中间铰链。本组平均手术时间约为120 min,平均失血量为400 ml,平均用止血带的时间为80 min。
四、术后恢复及随访
术后鼓励患者主动活动手部,肘关节制动至伤口愈合后。切除标本进行病理分析确定外科边界,15例广泛切除,9例边缘性切除。对所有患者进行规律随访,记录生存、转移、复发、功能及假体并发症情况。采用Mayo肘关节功能评分(Mayo elbow performance scorce,MEPS)(表1)及肌肉骨骼肿瘤协会(MSTS)关节功能评分系统评估患者的术后功能[1,4]。
结 果
1例患者失随访,其余23例患者均至少随访1年或随访至死亡(平均随访37个月)。在随访期间,11例患者无瘤生存;4例转移癌,1例骨肉瘤及1例尤文肉瘤患者分别死于术后2年内;2例尤文肉瘤、1例恶性纤维组织细胞瘤、1例骨肉瘤发生肺转移以及2例转移瘤患者带瘤生存。6例骨肉瘤中,失访、死亡、肺转移带瘤生存各1例,其余3例无瘤存活;4例尤文肉瘤中,1例死于肿瘤转移,2例肺转移带瘤生存,其余1例无瘤存活。肿瘤局部复发3例(13 %)。

图1 尺骨近端恶性纤维组织细胞瘤累及肱骨远端检查图像。A图示术前肘关节X线图像;B图示术前 CT图像;C、D图示术后肘关节X线图像;E图示切除标本图像

图2 肱骨远端骨巨细胞瘤检查图像。A、B图示术前X线图像;C、D图示术后X线图像;E图示术中图像
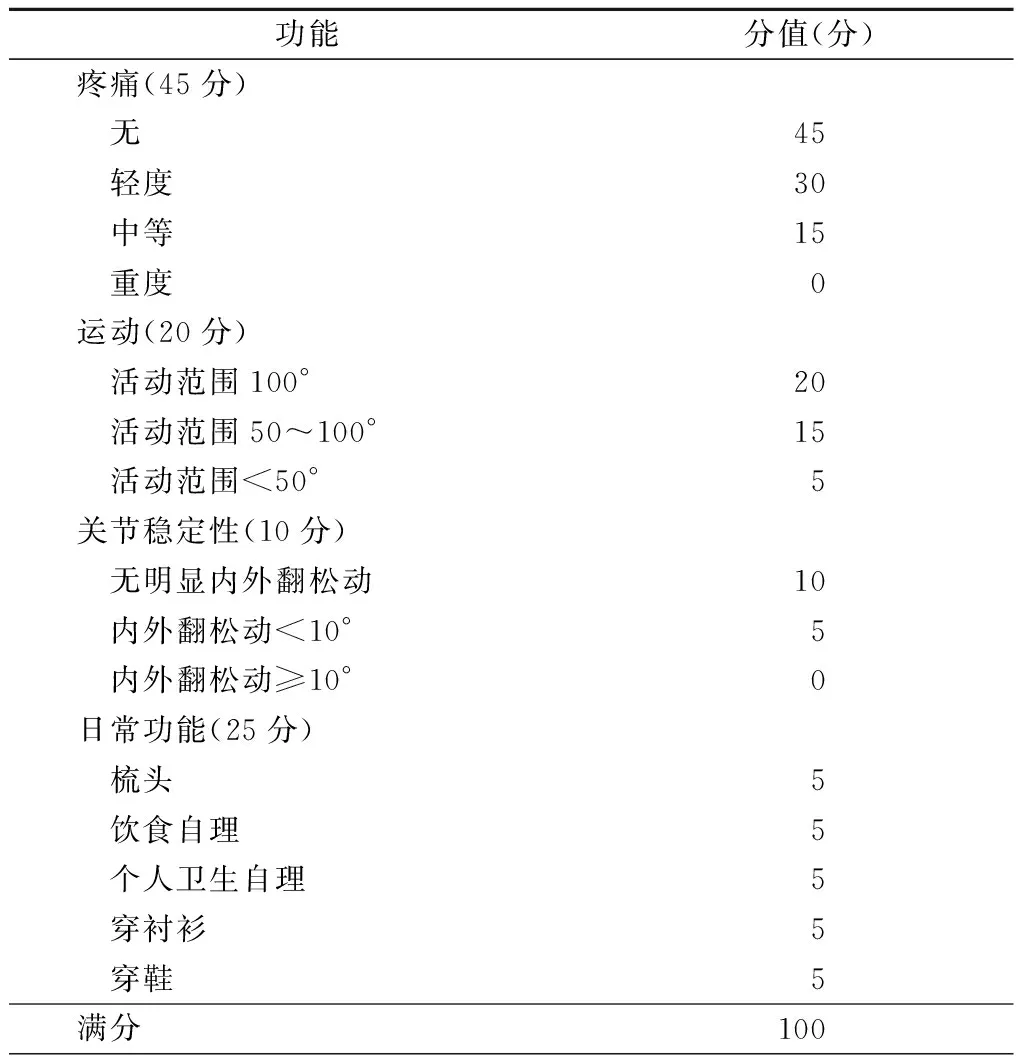
表1 Mayo肘关节功能评分系统
并发症发生率26.1% (6/23),包括桡神经牵拉伤1例,于术后6个月恢复;伤口不愈合2例,经清创好转;假体并发症3例,其中2例假体柄穿出骨皮质(图3),1例无菌性松动,行假体翻修术后均恢复良好功能。

图3 肱骨远端骨肉瘤患者术后4年(假体上端柄穿出骨皮质,进行假体翻修)检查图像和术中所见图像。A图示术前X线图像;B图示术后X线图像
术后MSTS评分:5例关节外肿瘤整块切除、人工肘关节置换的患者平均25分,18例关节内肿瘤切除、人工肘关节置换的患者平均25.9分。18例患者手术效果优良(18/23,78.3%),5例患者手术效果可以接受(5/23,21.7%)。MEPS评分平均80分。肘关节的平均屈伸范围由29°改善为73°(范围:55°~105°)。
讨 论
由于上肢解剖及功能要求特殊,使得肘部肿瘤切除与重建较为困难。切除成形术、关节融合、异体骨移植等曾用于肘关节重建,但都受到较多限制并且功能较差。虽然关节假体在骨肿瘤保肢治疗中已经广泛应用,但在肘部的应用报道较少,其多用于创伤、退行性关节病、类风湿性关节炎[5]。我们对肘关节周围肿瘤切除术后人工肘关节置换术的病例进行了总结,明确这种手术的疗效、并发症及术后功能。
一、全肘关节成形术中假体及病例的要求
在肿瘤切除术后,作为保肢手段而应用肘关节假体的报道很少。1987年,Ross等报道了26例患者因远端肱骨破坏而接受了假体置换术[6],所有植入物均为定制铰链式。接受假体置换术的患者中,12例为骨折或连枷肘,9例为高度恶性肿瘤,5例为低度恶性肿瘤,1例为肘关节转移瘤。肘关节的屈伸范围平均增加85°,但31%的患者出现神经损伤(多数发生在远端肱骨切除的病例)。本组全肘关节置换的病例中,仅1例出现神经损伤并发症。肱骨远端恶性肿瘤向外生长形成软组织包块时,行肿瘤广泛切除容易损伤桡神经,术中应注意游离出桡神经予以保护,如果肿瘤生长包裹桡神经则应选择切除神经。选择全肘关节成形术为重建方法时,假体及患者必须满足一定的要求。假体应该允许前臂及手稳定的活动,能够替代骨缺损的长度,力学强度能经得起日常使用;另外,假体必须从技术上容易安装,并且能保证固定牢靠[7]。在病例的选择方面,全肘成形术仅适用于那些血管神经束未被侵犯、前臂及手具有功能的患者。对于可能治愈性切除肿瘤的患者,如果需要牺牲肿瘤切缘来固定植入物,就不能选用全肘关节置换术。对于肿瘤广泛转移,预后较差的患者,可以根据需要选用肿瘤切除术、假体置换术、化疗或者放疗。这种情况下应当避免使用截肢术,以保留手及前臂的功能[1]。
二、肘关节肿瘤切除后重建的方法
肿瘤切除术后要重建功能稳定的肘关节,可供选择的重建方法不多。对于较小的骨缺损,常选用关节融合术或切除成形术。关节融合术导致手术后肘关节运动受限,切除成形术导致术后关节不稳定。对于较大的缺损,有报道应用同种异体肘关节移植。异体半关节移植能让软组织附着,保留肌肉功能,保持关节稳定性,但术后并发症较多,可高达70%[8-9]。术后常发生感染、关节不稳定、脱位。尽管有坚实的内固定,术后出现骨不连机会仍很高(约15%)。另外部分患者可出现异体骨吸收。本研究的结果表明,肿瘤切除后实施全肘关节成形术能够显著的减轻疼痛,改善功能。转移瘤的患者,特别是其他方法均不能缓解症状时,也可以采用这种手术方法。对于肘关节周围的肿瘤切除术后功能重建,目前没有比人工肘关节置换更好的方法。人工肘关节置换术后并发症发生率可以接受。Hanna等[10]报道18例肱骨远端肿瘤行人工肘关节置换的病例,包括12例原发肿瘤及6例转移瘤。并发症包括无菌性松动3例(16.6%)、感染2例(11%)、桡神经损伤1例(5.5%)及假体周围骨折1例(5.5%)。本组患者中,总体并发症发生率26.1%,假体相关并发症仅1例(4.3%)发生无菌性松动,有2例(8.7%)假体柄穿出骨皮质,未发现假体柄折断或假体周围感染的病例。
三、保证人工全肘关节置换术成功的要点
应注意以下几点:1、首先要遵循恶性肿瘤广泛切除的原则,否则易导致肿瘤局部复发;2、肿瘤切除后局部要有充分的软组织覆盖,以免切口出现问题,导致假体置换手术失败;3、对于肱骨远端部位的肿瘤,手术切除肿瘤后,尽量修复前臂屈伸及旋前旋后肌群的起止点。如果可能,术中应尽量保留部分肱骨内、外侧髁;4、由于尺骨髓腔较细,灌入骨水泥较少,因而尺骨髓腔内的假体柄可设计成粗螺纹式,便于骨水泥固定,防止假体旋转及松动;5、由于尺骨有弯曲且髓腔较细,尺骨髓腔内的假体柄一定不要太长,以5~7 cm为宜,否则容易穿出骨皮质;6、对于尺骨近端部位的肿瘤,应保留肱骨内外髁,安装肱骨远端假体时,将肱骨远端髁间窝锯掉,将假体嵌入髁间窝部位。这样,一方面保留了肌肉的起止点,另一方面还能防止假体旋转。
四、功能评价
本组病例中,所有患者术后3周开始功能锻炼。8周后患者肘关节活动接近正常,活动范围在50°~90°者占70%,活动范围<50°者占5%,活动范围>90°者占25%。90%的患者活动时无疼痛,80%的患者术后保留前臂的旋转功能。人工肘关节置换术后的患者应避免手提重物及用力旋转前臂,以免出现假体松动及骨折。定制型人工肘关节的寿命目前尚不清楚,以往文献报道的人工肘关节置换多为类风湿性关节炎或骨性关节炎病例,且多为老年患者,对肘关节的功能要求较低,主要目的是解除疼痛症状。理论上,肘关节肿瘤切除后人工肘关节置换,由于切除范围广、假体节段长、患者年轻及使用频率高,所以并发症相对高,假体寿命短。Weber 等[11]报道23例肘关节肿瘤患者,包括15例原发肿瘤及8例转移瘤患者。其中11例患者采用了肘关节肿瘤切除后人工肘关节置换,平均MSTS评分83%。Kulkarni 等[12]报道10例肱骨远端肿瘤切除、人工肘关节置换患者,所有患者疼痛解除、肘关节功能良好。Schwab 等[13]最近报道了5例肘关节肿瘤、关节外切除患者,平均MSTS评分25.2分。本组病例中,5例关节外肿瘤整块切除重建患者,平均MSTS评分25分,略低于关节内肿瘤切除重建患者。关节外肿瘤切除的病例,往往肿瘤范围广、体积较大,软组织切除较多,因而术后功能受到影响。
综上所述,对于适当的患者进行肘部肿瘤切除、人工关节假体重建可以提供良好的肿瘤学结果,较低的并发症发生率,获得良好的术后功能。
参 考 文 献
[1] Sperling JW, Pritchard DJ, Morrey BF.Total elbow arthroplasty after resection of tumors at the elbow[J]. Clin Orthop Relat Res,1999,(367):256-261.
[2] Urbaniak JR, Black KE. Cadaveric elbow allografts. A six-year experience[J]. Clin Orthop Relat Res,1985,(197):131-140.
[3] Kharrazi FD, Busfield BT, Khorshad DS, et al.Osteoarticular and total elbow allograft reconstruction with severe bone loss[J].Clin Orthop Relat Res,2008,466(1):205-209.
[4] Enneking WF, Dunham W, Gebhardt MC, et al. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system[J]. Clin Orthop Relat Res,1993,(286):241-246.
[5] Aldridge JM 3rd, Lightdale NR, Mallon WJ,et al.Total elbow arthroplasty with the Coonrad/Coonrad-Morrey prosthesis. A 10-to 31-year survival analysis[J].J Bone Joint Surg Br,2006,88(4):509-514.
[6] Ross AC, Sneath RS, Scales JT. Endoprosthetic replacement of the humerus and elbow joint[J]. J Bone Joint Surg Br,1987,69(4):652-655.
[7] Morrey BF, Bryan RS, Dobyns JH, et al. Total elbow arthroplasty. A five-year experience at the Mayo Clinic[J]. J Bone Joint Surg Am,1981,63(7):1050-1063.
[8] Dean GS, Holliger EH 4th, Urbaniak JR.Elbow allograft for reconstruction of the elbow with massive bone loss. Long term results [J]. Clin Orthop Relat Res,1997,(341):12-22.
[9] Mankin HJ, Gebhardt MC, Jennings LC, et al. Long-term results of allograft replacement in the management of bone tumors[J]. Clin Orthop Relat Res,1996,(324):86-97.
[10] Hanna SA, David LA, Aston WJ, et al. Endoprosthetic replacement of the distal humerus following resection of bone tumours[J]. J Bone Joint Surg Br,2007,89(11):1498-1503.
[11] Weber KL, Lin PP, Yasko AW. Complex segmental elbow Reconstruction after tumor resection[J]. Clin Orthop Relat Res,2003,(415):31-44.
[12] Kulkarni A, Fiorenza F, Grimer RJ, et al. The results of endoprosthetic replacement for tumours of the distal humerus[J]. J Bone Joint Surg Br,2003,85(2):240-243.
[13] Schwab JH, Healey JH, Athanasian EA. Wide en bloc extra-articular excision of the elbow for sarcoma with complex Reconstruction[J]. J Bone Joint Surg Br,2008,90(1):78-83.