老年糖尿病合并稳定型心绞痛患者糖基化产物水平与冠状动脉介入治疗预后的关系
刘丽丽, 李贤峰, 刘 敏, 刘振华, 何疆春
老年糖尿病合并稳定型心绞痛患者糖基化产物水平与冠状动脉介入治疗预后的关系
刘丽丽1*, 李贤峰2, 刘 敏3, 刘振华4, 何疆春2
(海军总医院:1航空潜水医学专科中心,2心血管内科,3检验科, 北京 100048;4解放军总参管理保障部保健处, 北京 100034)
检测冠心病稳定型心绞痛合并2型糖尿病老年患者冠状动脉介入术前的血糖及糖基化产物水平,了解其与介入治疗短期预后的关系。连续选取2010年1月至2012年12月于海军总医院住院接受冠状动脉介入治疗的稳定型心绞痛合并2型糖尿病老年患者188例,根据是否出现缺血并发症如复发心绞痛、心肌梗死及死亡,将患者分为事件组和对照组;观察两组心血管病术前临床危险因素、血糖、糖基化产物(糖化血红蛋白和糖化血清蛋白)及高敏C反应蛋白水平的差异,评价各组术前危险因素、糖代谢及炎症反应指标的差异。事件组与对照组相比较,年龄、性别、体质量指数、吸烟史、高血压及高脂血症发病率、用药情况以及糖化血红蛋白水平差异均无统计学意义(>0.05);空腹血糖、糖化血清蛋白以及高敏C反应蛋白水平明显增高(<0.01);以220μmol/L为界值,糖化血清蛋白升高患者出现围术期缺血并发症的风险明显增加(OR=2.96,95%CI:1.50~5.81,=0.001)。糖基化产物中,术前糖化血清蛋白水平增高可能是糖尿病合并稳定型心绞痛老年患者冠状动脉介入治疗围术期缺血并发症的危险预测指标。
老年人; 糖尿病; 冠心病; 经皮冠状动脉介入治疗; 血红蛋白A, 糖基化; 糖化血清蛋白
糖尿病患者非酶糖基化产物(non-enzymatic glycation products)水平明显增高,包括糖化血红蛋白(glycosylated hemoglobin A1c,HbA1c)和糖化血清蛋白(glycosylated serum protein,GSP)以及晚期糖基化终末产物(advanced glycation end products,AGEs),由于目前AGEs的测定标准不一,目前临床常用的糖基化产物检测指标主要是HbA1c以及GSP,为了解糖基化产物水平升高是否与老年糖尿病合并稳定型心绞痛患者冠状动脉介入术后缺血并发症相关,本研究选取了2010年至2012年间就诊于海军总医院接受冠状动脉介入治疗的2型糖尿病(type 2 diabetes mellitus,T2DM)合并冠心病稳定型心绞痛的老年患者,对其进行空腹血糖(fasting blood glucose,FBG)、HbA1c、GSP水平的检测,以探讨糖基化产物水平对糖尿病患者冠状动脉介入术后不良预后的关系。
1 对象与方法
1.1 对象及分组
2010年1月至2012年12月,于海军总医院心血管内科住院拟择期行冠状动脉介入治疗的T2DM合并冠心病稳定型心绞痛的老年患者共188例,年龄65~86(71±5)岁,所有患者均排除可能会影响GSP水平的以下伴随疾病:肝、肾功能不全,低蛋白血症,异常血红蛋白血症,溶血性贫血,缺血性心肌病。其中冠心病及稳定型心绞痛诊断符合2007年美国心脏病学会(ACC)与美国心脏联合会(AHA)指南,T2DM符合2009年美国糖尿病协会诊断标准。患者接受冠状动脉介入治疗后,于术后24和72h行心肌酶检测并观察术后1周内心绞痛发生情况;根据是否出现术后不良事件(心绞痛、心肌梗死及死亡)将患者分为事件组(出现不良预后事件)及对照组(无不良预后事件)。
1.2 流行病学指标采集
入院时采用问卷形式,进行一般情况及心血管病危险因素的采集,包括:年龄,性别,身高,体质量,相关疾病史(高血压、高脂血症史),吸烟史(>5支/d、持续5年以上),用药情况[胰岛素、β受体阻滞剂、他汀类、血管紧张素转换酶抑制剂(angiotensin converting enzyme inhibitor,ACEI)/血管紧张素受体拮抗剂(angiotensin receptor blocker,ARB)]等。
1.3 空腹血糖、糖基化蛋白、炎症指标及心肌酶检测
于入院后次日晨起空腹采集静脉血标本检测患者FBG、HbA1c、GSP、高敏C反应蛋白(high sensitivity C reactive protein,hs-CRP)、肌酸激酶同工酶(creatine kinase isoenzyme,CK-MB)等;于术后24h和72h分别抽取静脉血标本,检测CK-MB水平;介入术后心肌梗死定义为,术后CK-MB升高至正常值上限3倍以上。
1.4 统计学处理
采用SPSS13.0软件进行数据统计学分析。计量资料采用均数±标准差表示,两组间计量资料的平均值比较采用检验;计数资料采用百分率表示,两组间计数资料比较采用2检验。<0.05为差异有统计学意义。
2 结 果
2.1 两组流行病学指标比较
接受冠状动脉介入治疗的糖尿病合并冠心病稳定型心绞痛的老年患者中,共有48例出现围术期不良事件,占本试验人群的25.5%,其中35例出现介入术后心绞痛,12例出现介入术后心肌梗死,1例死亡;事件组与对照组比较,其年龄、性别、体质量指数(body mass index,BMI)、吸烟史、高血压及高脂血症发病率、采用胰岛素治疗比例及主要合并用药情况差异均无统计学意义(>0.05;表1)。
2.2 事件组与对照组糖代谢、炎症指标及介入治疗相关指标比较
与对照组比较,事件组患者HbA1c水平差异无统计学意义(>0.05),晨起FBG、GSP以及hs-CRP水平明显增高(<0.05,<0.01;表2)。
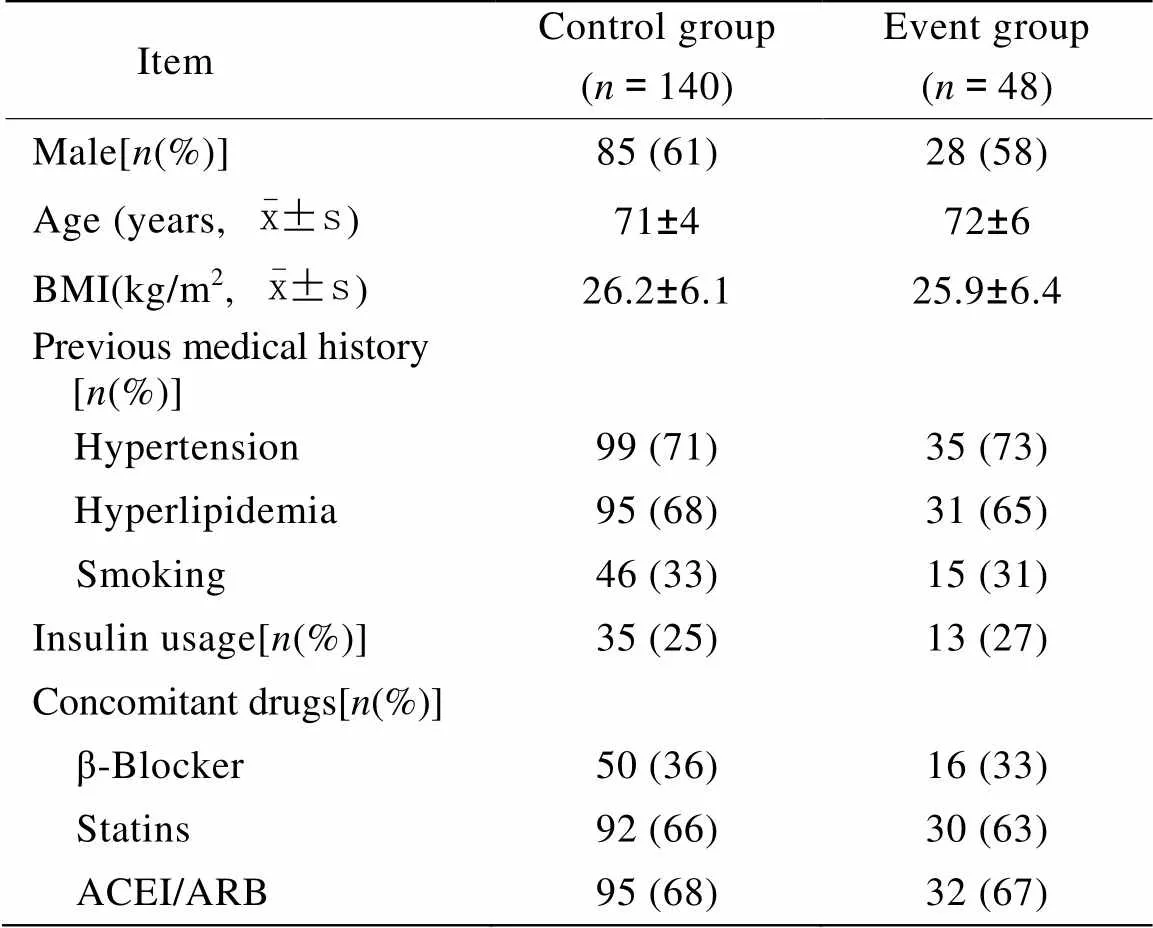
表1 两组患者流行病学指标比较
BMI: body mass index; ACEI: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker
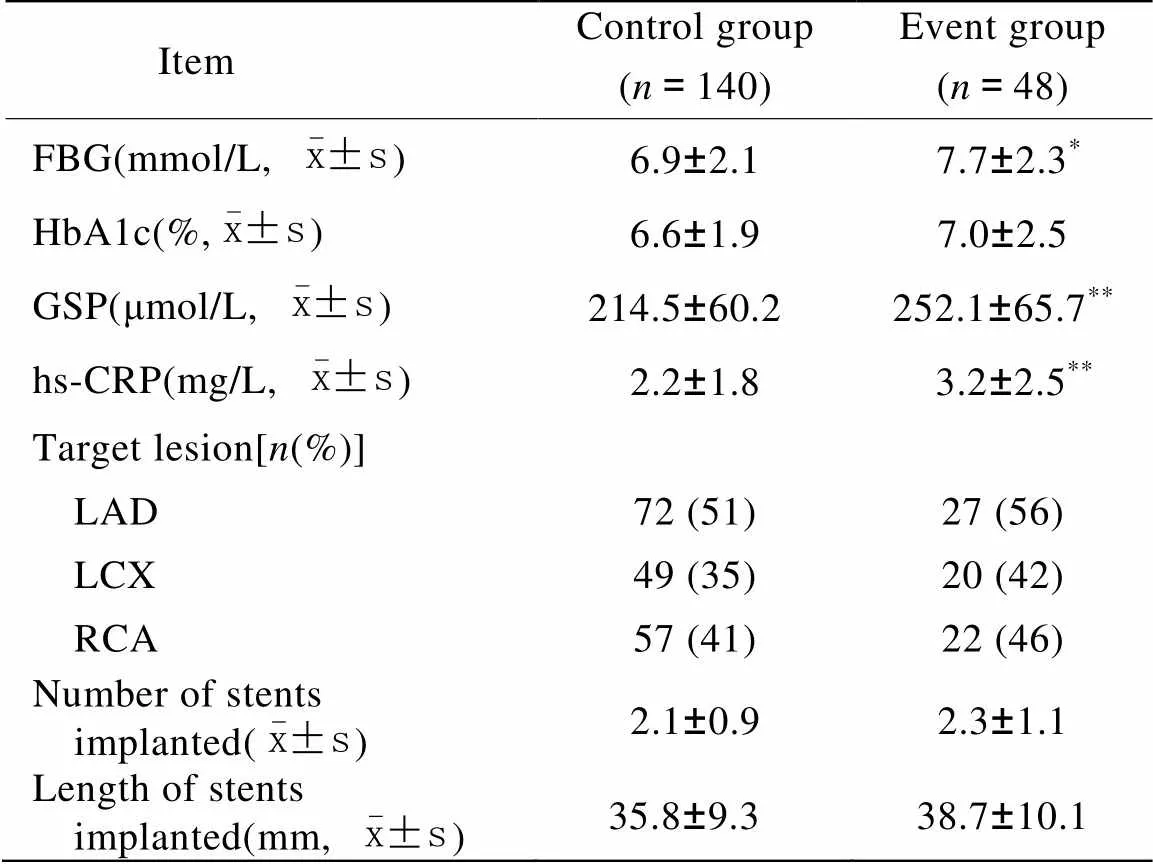
表2 两组糖代谢、炎症指标及介入治疗相关指标比较
FBG: fasting blood glucose; HbA1c: glycosylated hemoglobin A1c; GSP: glycosylated serum protein; hs-CRP: high sensitivity C reactive protein; LAD: left anterior descending branch; LCX: left circumflex artery; RCA: right coronary artery. Compared with control group,*<0.05,**<0.01
2.3 GSP升高对T2DM合并冠心病患者发生介入术后院内不良预后事件风险的影响
本研究将T2DM患者的GSP值以10μmol/L分层,发现GSP>220μmol/L时,T2DM患者发生冠状动脉介入围术期的不良预后事件的相对风险明显升高;GSP>220μmol/L的患者行冠状动脉介入治疗共66例,其中26例(39%)出现术后缺血并发症,GSP≤220μmol/L的患者共122例,其中22例(18%)出现术后缺血并发症,以GSP220μmol/L作为分界点,GSP升高患者发生术后缺血事件的相对风险OR为2.96(2=10.28,95% CI:1.50~5.81,=0.001)。
3 讨 论
糖尿病患者体内葡萄糖与各种蛋白发生非酶糖化反应,形成Amadori产物,其中包括HbAlc和GSP。Amadori产物再通过一系列反应最终生成晚期AGEs。糖尿病合并冠心病患者接受冠状动脉介入治疗,与无糖尿病的患者相比,其手术相关的并发症发生率明显增加,术后近期及远期预后明显变差[1,2]。有研究发现,血糖控制不佳可能是预后不良的危险因素,围术期加强血糖控制有助于改善患者预后[3−5],血糖控制不佳,同样也会导致患者糖基化产物水平显著增高。
HbA1c作为最广泛检测的糖基化产物,既往有研究认为,其水平增高与冠状动脉介入术后支架再狭窄、血栓形成等密切相关[6],但近年来的几项研究表明,HbA1c增高对冠状动脉介入治疗预后的影响作用并不明显[7,8],而其他糖基化产物水平如GSP、AGEs等对预后的预测作用越来越受到临床重视[9−11],本研究发现,接受冠状动脉介入治疗出现围术期不良预后事件的糖尿病患者,其FBG明显升高,HbA1c水平虽存在差异,但差异无统计学意义,而GSP水平有显著差异。由于GSP的波动与近期(2~3周)血糖变化有关,而HbA1c反映过去2~3个月的血糖平均水平,此结果提示,与慢性血糖控制不良因素相比,短期血糖波动可能是更能诱发急性冠状动脉斑块不稳定的危险因素。另一方面,炎症活动同样也能够导致短期的血糖波动,导致糖基化产物水平增高,而糖基化产物也会加速炎症过程;两者相互作用,加速糖尿病患者血管并发症的发生和进展[12−14]。本研究发现事件组的患者hs-CRP水平明显升高,这提示体内急性炎症活动频繁,诱发不良事件的同时导致应激性血糖波动,致使两组空腹血糖及GSP水平出现显著差异,这可能是患者不良预后的主要原因。
稳定型心绞痛患者接受择期冠状动脉介入治疗,其围术期风险低于急性冠脉综合征患者,临床上常常忽视对这一群相对低危患者进行术前的危险分层,目前对此类患者也缺乏有效的危险分层因子;本研究发现出现不良预后事件的糖尿病合并稳定型心绞痛患者的FBG及GSP均明显升高,但FBG由于受到饮食、疾病等因素影响,可重复性差,而GSP是血清中蛋白质与葡萄糖发生非酶促反应的产物,其指标不受短期内饮食等因素的影响,较FBG更为稳定,适于作为危险分层的指标。本研究将T2DM患者的GSP值以10μmol/L分层,发现GSP>220μmol/L时,T2DM患者接受冠状动脉介入治疗围术期出现不良预后事件的例数明显增加;所以,在对糖尿病合并稳定型心绞痛的患者进行冠状动脉介入治疗之前,临床医师可将GSP作为危险度分层指标,筛查出可能的围术期高危患者,术后密切观察,必要时强化治疗,从而改善患者预后。
本研究发现糖尿病合并稳定型心绞痛老年患者接受冠状动脉介入治疗前出现GSP升高时,其发生围术期并发症相对风险也明显增加。提示在对糖尿病合并稳定型心绞痛患者进行冠状动脉介入治疗前除常规检查血糖及HbA1c等指标外,测定GSP可能对围术期预后具有危险度分层的作用。
[1] Settler C, Allemann S, Wandel S,. Drug eluting and bare metal stents in people with and without diabetes: collaborative network meta-analysis[J]. BMJ, 2008, 337: a1331.
[2] Sato T, Ono T, Morimoto Y,. Differences in clinical and angiographic outcomes with different drug-eluting stents in Japanese patients with and without diabetes mellitus[J]. J Cardiol, 2012, 60(5): 361−366.
[3] Marfella R, Sasso FC, Siniscalchi M,. Peri-procedural tight glycemic control during early percutaneous coronary intervention is associated with a lower rate of in-stent restenosis in patients with acute ST-elevation myocardial infarction[J]. J Clin Endocrinol Metab, 2012, 97(8): 2862−2871.
[4] Nusca A, Patti G, Marino F,. Prognostic role of preprocedural glucose levels on short- and long-term outcome in patients undergoing percutaneous coronary revascularization[J]. Catheter Cardiovasc Interv, 2012, 80(3): 377−384.
[5] Zhang QY, Li Y, Guan SY,. Incidence and predictors of definite stent thrombosis after coronary stent implantation[J]. Chin Med J (Engl), 2012, 125(9): 1547−1551.
[6] Corpus RA, George PB, House JA,. Optimal glycemic control is associated with a lower rate of target vessel revascularization in treated typeⅡ diabetic patients undergoing elective percutaneous coronary intervention[J]. J Am Coll Cardiol, 2004, 43(1): 8−14.
[7] Lima-Filho MO, Figueiredo GL, Foss-Freitas MC,. Predictors of restenosis after percutaneous coronary intervention using bare-metal stents: a comparison between patients with and without dysglycemia[J]. Braz J Med Biol Res, 2010, 43(6): 572−579.
[8] Lemesle G, Bonello L, de Labriolle A,. Prognostic value of hemoglobin A1C levels in patients with diabetes mellitus undergoing percutaneous coronary intervention with stent implantation[J]. Am J Cardiol, 2009, 104(1): 41−45.
[9] Pfutzner A, Marx N, Lubben G,. Improvement of cardiovascular risk markers by pioglitazone is independent from glycemic control: results from the pioneer study[J]. J Am Coll Cardiol, 2005, 45(12): 1925−1931.
[10] Park HJ, Seo SM, Shin WS,. Soluble receptor for advanced glycation end products is associated with in-stent restenosis in patients with type 2 diabetes with drug-eluting coronary stents[J]. Coron Artery Dis, 2011, 22(1): 12−17.
[11] Lu L, Jin Pu L, Chen QJ,. Increased glycated albumin and decreased esRAGE concentrations are associated with in-stent restenosis in Chinese diabetic patients[J]. Clin Chim Acta, 2008, 396(1−2): 33−37.
[12] Xie Y, You SJ, Zhang YL,. Protective role of autophagy in AGE-induced early injury of human vascular endothelial cells[J]. Mol Med Report, 2011, 4(3): 459−464.
[13] Schalkwijk CG, Lieuw-a-Fa M, van Hinsbergh VW,. Pathophysiological role of Amadori-glycated proteins in diabetic microangiopathy[J]. Semin Vasc Med, 2002, 2(2): 191−197.
[14] Fukushima Y, Daida H, Morimoto T,. Relationship between advanced glycation end products and plaque progression in patients with acute coronary syndrome: the JAPAN-ACS Sub-study[J]. Cardiovasc Diabetol, 2013, 12: 5.
(编辑: 周宇红)
Relationship of serum levels of glycosylated products with prognosis in elderly type 2 diabetic patients after percutaneous coronary intervention for stable angina
LIU Li-Li1*, LI Xian-Feng2, LIU Min3, LIU Zhen-Hua4, HE Jiang-Chun2
(1Center for Naval Aviation and Diving Medicine,2Department of Cardiology,3Department of Clinical Laboratory, Navy General Hospital, Beijing 100048, China;4Division of Healthcare, Department of Management and Logistic Support, Headquarters of General Staff of PLA, Beijing 100034, China)
To investigate the pre-operative serum levels of glycosylated products in the elderly type 2 diabetes mellitus patients with stable angina undergoing selective percutaneous coronary intervention(PCI), and evaluate the relationship between the levels and short-term outcomes.A total of 188 elderly patients with diabetes and stable angina who were treated with PCI in our hospital from January 2010 to December 2012 were consecutively enrolled in this study. The patients were divided into 2 groups according to onset of post-procedure outcome events, the control group(no event) and the event group(ischemic events: post-procedure angina, myocardial infarction and death). The profiles of clinical cardiovascular risk factors, levels of fasting blood glucose, glycosylated products [glycosylated hemoglobin A1c(HbA1c) and glycosylated serum protein(GSP)] and high sensitivity C reactive protein(hs-CRP) were collected before PCI and compared between 2 groups.There was no significant difference in the age, gender, body mass index, history of smoking, incidences of hypertension and hyperlipidemia, medication, and serum HbA1c level between 2 groups(>0.05). However, the patients in event group had significantly higher levels of fasting blood glucose, GSP and hs-CRP than those in control group(<0.01). The risk of complicating post-procedure ischemic events in the patients with higher GSP levels(>220μmol/L) was much higher than that in patients having lower GSP levels(OR=2.96, 95% CI=1.50-5.81,=0.001).Elevated GSP level before PCI may be a risk factor of post-procedure ischemic events in the elderly patients with diabetes and stable angina undergoing selective PCI.
aged; diabetes mellitus; coronary heart disease; percutaneous coronary intervention; hemoglobin A, glycosylated; glycosylated serum protein
(BHJ09JD08).
R541.4; R592
A
10.3724/SP.J.1264.2013.00192
2013−07−30;
2013−08−13
海后卫生部科研课题(BHJ09JD08)
刘丽丽, E-mail: xuliuown@hotmail.com

