Predictors of re-hospitalization over a two-year follow-up period among patients with schizophrenia enrolled in a community management program in Chengdu, China
Yinbo ZHANG*, Guangzhi DAI
· Research Article ·
Predictors of re-hospitalization over a two-year follow-up period among patients with schizophrenia enrolled in a community management program in Chengdu, China
Yinbo ZHANG*, Guangzhi DAI
Community; Schizophrenia; Re-hospitalization; Factor analysis; Prospective study
1.Introduction
In many western countries the de-institutionalization movement of the 1960s resulted in the gradual expansion of community mental health services. The focus of services changed from controlling the mentally ill in large specialized institutions to the communitybased prevention, treatment and rehabilitation of mental illnesses[1]. But the level of community services varied by region[2,3]and the effectiveness of such services in reducing the frequency and duration of psychiatric hospitalization remained controversial[4-7].
In China community mental health services were under-developed until the government recently decided to integrate mental health care with the expanding community-based public health services[8]. Over the last decade community management and rehabilitation of persons with schizophrenia has become one of the core activities of the new community-based general health services. But it is uncertain whether or not the changed focus of services is, in fact, having an effect onhospitalization rates. Most previous studies about rehospitalization and relapse of schizophrenia in China use inpatient samples and do not consider the potential role of community-based services[9-11]. The current paper aims to identify factors influencing re-hospitalization among patients who are currently receiving community services.
2.Subjects and methods
2.1 Subjects
The enrollment and follow-up of subjects is shown in Figure 1. Patients who meet diagnostic criteria of schizophrenia (based on the third revision of the Chinese Classification of Mental Disorders[12]),who participated in the Community Treatment and Management Network at 24 Community Health Centers in two urban districts of Chengdu (the capital of Sichuan Province) in May 2009, and who had had at least one prior psychiatric hospitalization were enrolled.Some patients officially categorized as suffering from schizophrenia in the community program did not have their diagnosis confirmed by a psychiatrist, so only those subjects with a prior psychiatric hospitalization(who, therefore, had a confirmed diagnosis) were included in this analysis. A total of 1,027 patients were enrolled in this follow-up project. All the patients or their guardians signed informed consent to participate in the management network.
2.2 Methods
Enrolled patients were followed for two years.Enrollment evaluations were conducted by four psychiatrists and follow-up evaluations were conducted by 32 community-based general physicians who had had additional training in mental health and were responsible for the management of mentally ill patients at the Community Health Centers (these centers are general health clinics, not specialized psychiatric clinics).
Intake assessment included collection of information on basic demographic characteristics: gender age,years of schooling, living situation, marital status,and employment status over the last six months(dichotomized as stable employment or no stable employment). During the follow-up period the community management services involved at least one telephone contact per month and at least one face-toface interview at the Community Health Center every three months. Every month the community physician assessed the patient’s status by administering the 33-item Positive and Negative Syndrome Scale, (PANSS)[13]and the 10-item the Social Disability Screening Schedule(SDSS)[14]. During follow-up visits the number of days taking medications as prescribed and the number of days in hospital since the previous follow-up visit were also recorded.
2.3 Statistical analysis
Data were analyzed using SPSS software, version13.0. Univariate comparison of the characteristics of those who did and did not complete follow-up and of those who did and did not get re-hospitalized during follow-up used Chi-squared tests for dichotomous variables and t-tests for continuous variables. Logistic regression and stepwise logistic regression were used to identify factors associated with rehospitalization.
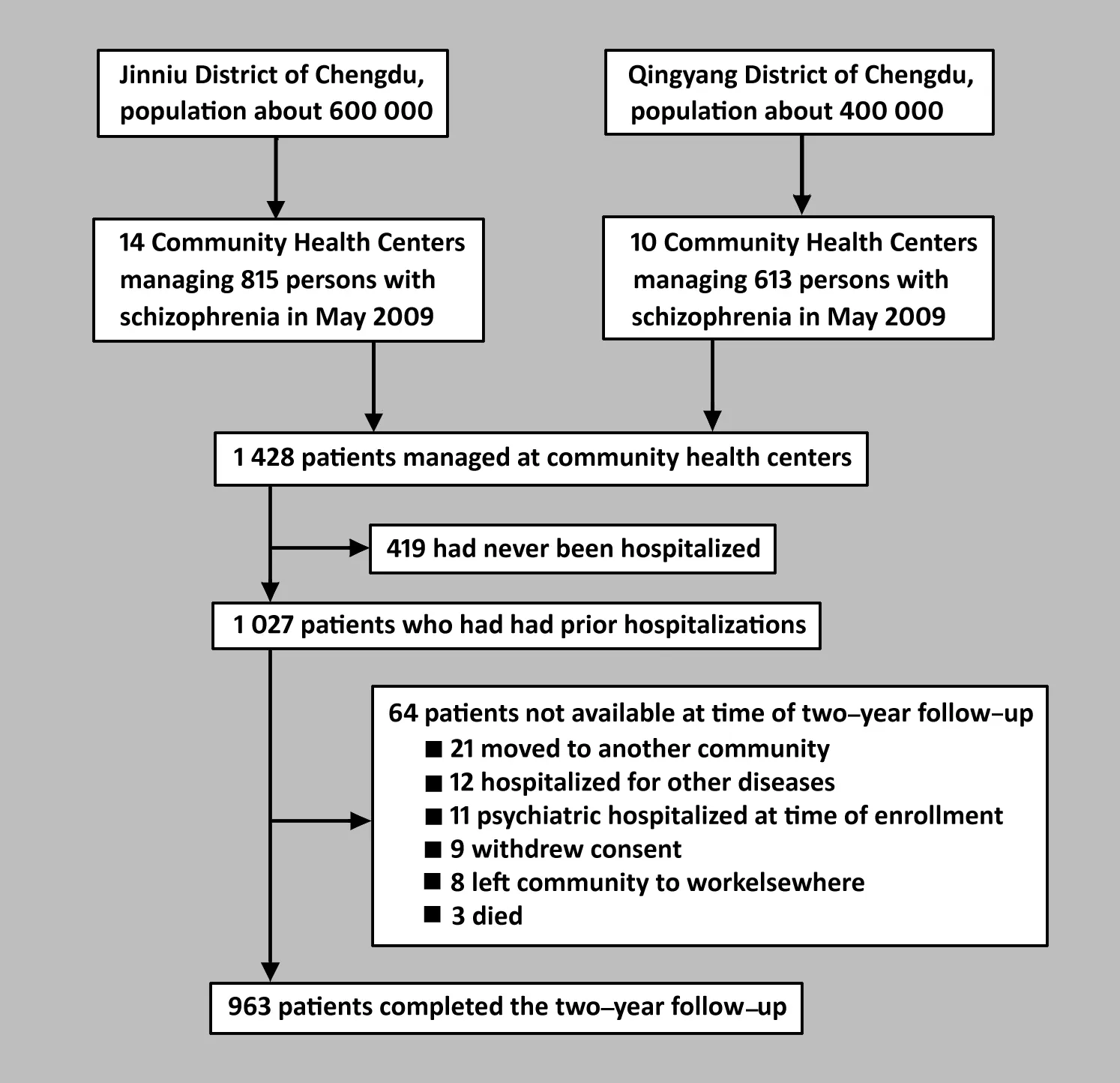
Figure 1. Enrollment and follow-up of subjects
The study was approved by the ethics review board of the Chengdu City Number 4 Peoples Hospital.
3.Results
Baseline characteristics of the 1 027 enrolled patients are presented in Table 1. Most of the patients were middle age unmarried males living with family members who had already been participating in the Community Treatment Management Network for three to four years at the time of enrollment in this follow-up project.
3.1 Comparison of patients who did and did not complete the two-year follow-up
As shown in Figure 1, 963 of the 1 027 (93.8%)enrolled subjects continued to participate in the management network at the end of the two-year follow-up period. The main reasons for dropping out(shown in Figure 1) were moving to another community,chronically hospitalization for physical illnesses, and chronic psychiatric hospitalization starting prior to enrollment and continuing throughout the two-year follow-up period. As shown in Table 1, at the time of enrollment those who did not complete the followup had less education, were less likely to be living with family members and had had more prior psychiatric hospitalizations than those who did complete the follow-up, but, somewhat surprisingly, they had less severe positive symptoms, had been taking medications more regularly in the six months before enrollment and had been hospitalized less over the six months before enrollment.
3.2 Comparison of patients who did and did not get re-hospitalized during the two-year follow-up
Among these 963 patients who completed the twoyear follow-up, 174 (18.1%) were re-hospitalized at least once over the two years. Among them 23 (2.4%)were re-hospitalized more than once over the two-year period. Among these re-hospitalized patients the mean(SD) time from enrollment to the first hospitalization was 41 (21) days and the mean total duration of hospitalization over the two-year follow-up period was 34 (32) days.
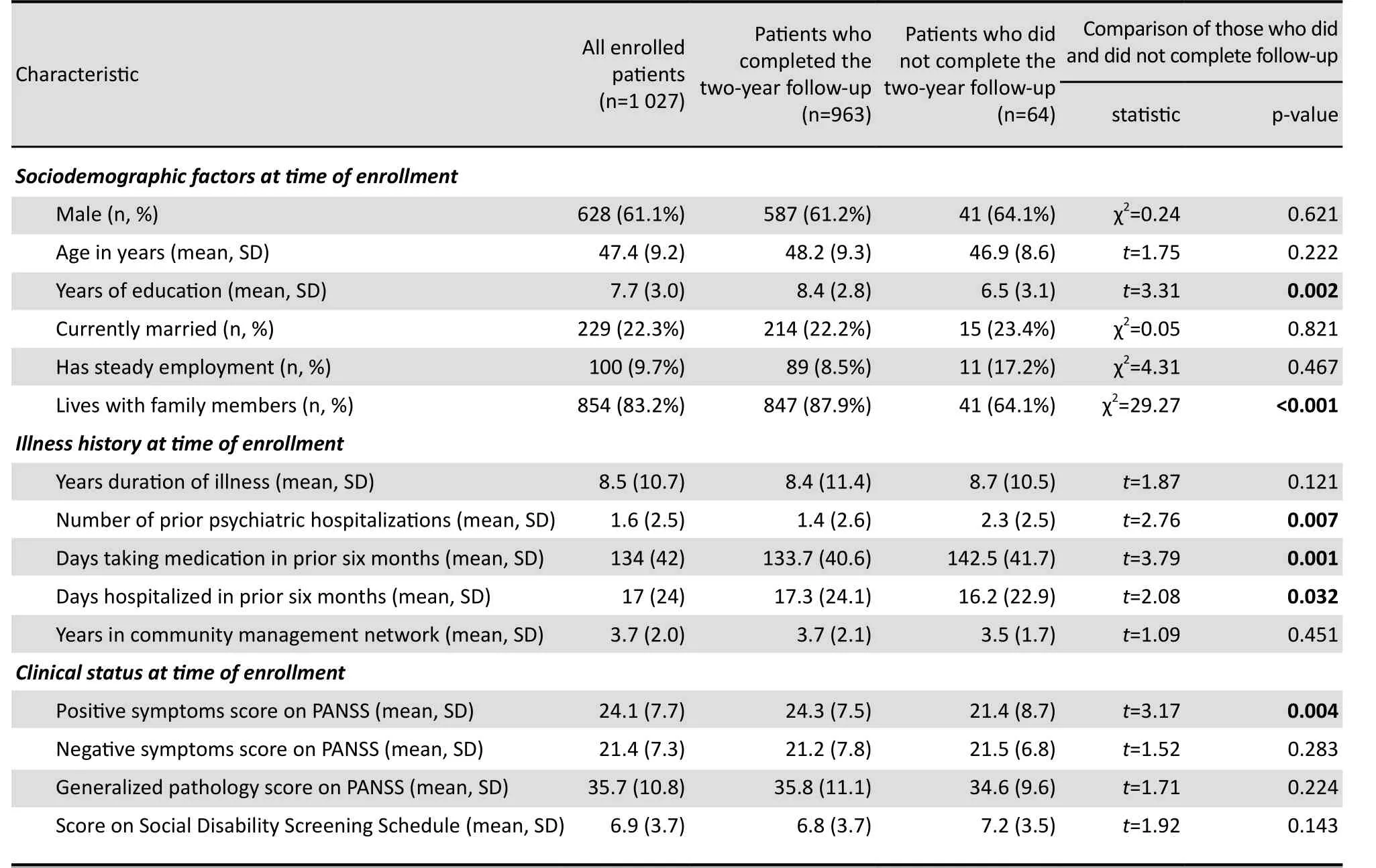
Table 1. Comparison of baseline characteristics of patients with schizophrenia who did and did not complete the two-year follow-up in a community-based program in Chengdu, China
Univariate comparison of the characteristics at thetime of enrollment of individuals who did and did not get re-hospitalized over the two-year follow-up period is shown in Table 2. It shows that patients who were re-hospitalized had a lower level of education, were less likely to be married or living with family members at the time of enrollment, had taken medication less regularly and were hospitalized less in the six months prior to enrollment, and had more severe symptoms and greater social disability at the time of enrollment.
Results of the logistic regression analysis to identify factors independently associated with re-hospitalization are presented in Table 3. It shows that when all the factors are included in the model re-hospitalization over the two year follow-up is more common in patients who were not married or not living with family members at the time of enrollment, who had used medication less in the six months prior to enrollment, and who had more prominent positive and negative symptoms at the time of enrollment. A subsequent analysis using stepwise forward entry of variables found that the following variables remained significantly associated with re-hospitalization: not living with family members(OR=3.23, 95% CI=1.92-3.57), using psychiatric mediation for a shorter time in the six months prior to enrollment (OR=2.13, CI=1.35-2.44), and having more prominent positive symptoms (OR=2.27, CI=2.19-3.21)or negative symptoms (OR=1.88, CI=1.64-3.01) at thetime of enrolment. A parallel multiple logistic regression analysis to identify factors associated with multiple (i.e.,two or more) admissions over the two-year follow-up found that prominent negative symptoms at the time of admission (0R=2.02, CI=1.96-2.27) and shorter time using medication in the six months prior to enrollment were significantly associated with multiple admissions.
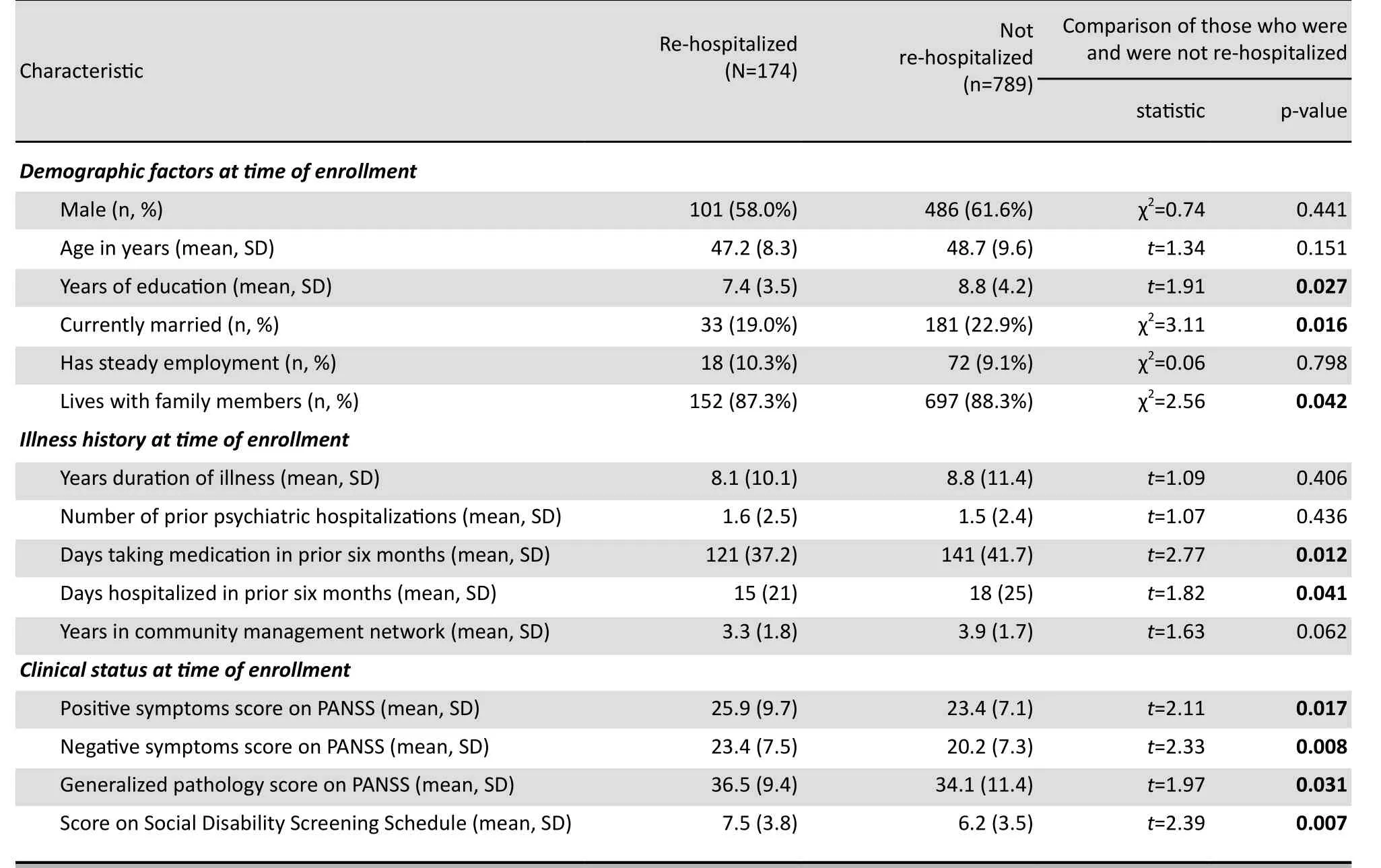
Table 2. Comparison of baseline characteristics of 963 patients with schizophrenia who did and did not get re-hospitalized during a two-year community-based follow-up program in Chengdu, China
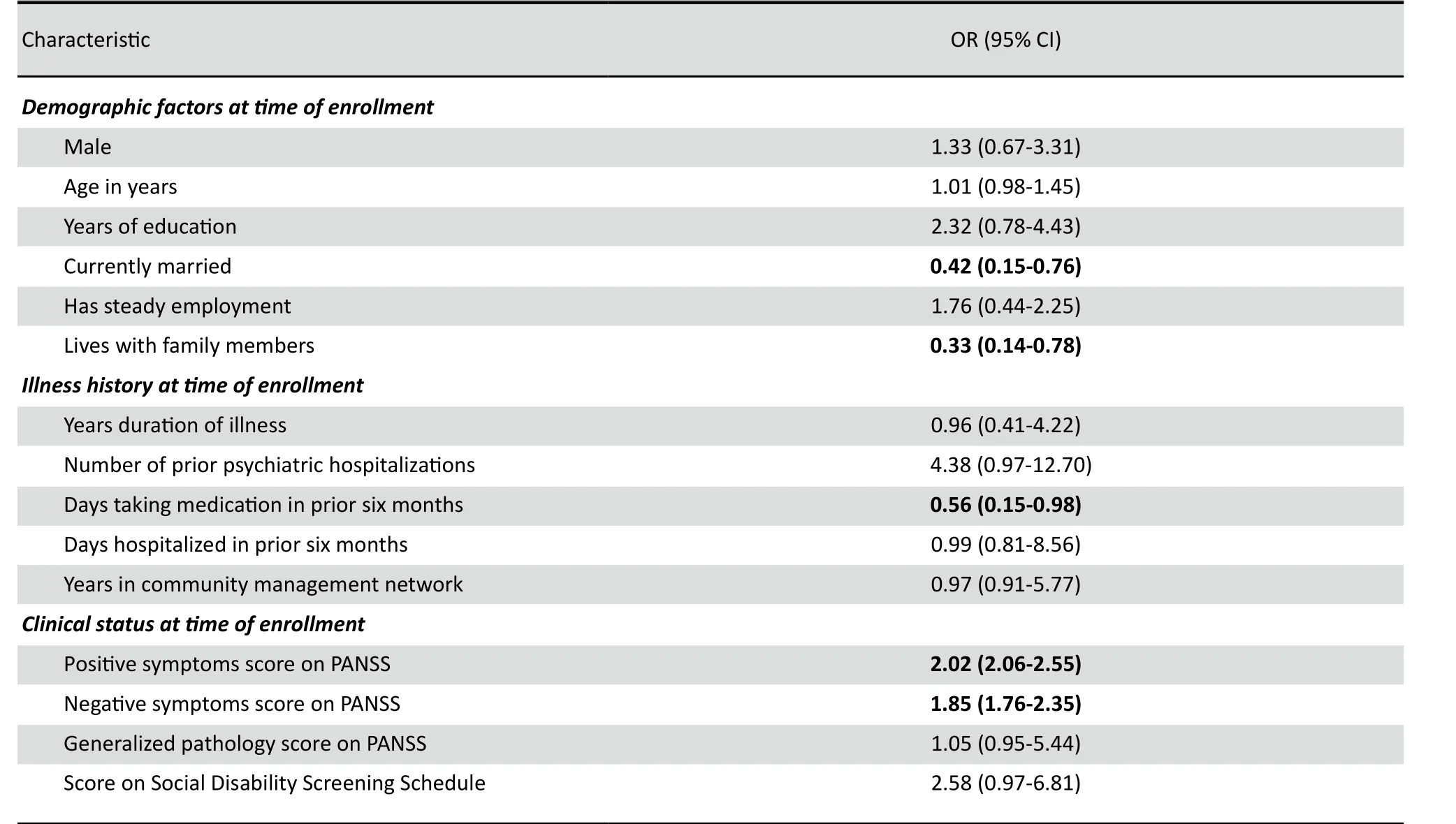
Table 3. Logistic regression analysis of predictors of re-hospitalization over a two-year follow-up period among 963 patients with schizophrenia enrolled in a community management program in Chengdu, China
4.Discussion
4.1 Main findings
This two-year prospective study is part of the accumulating literature[15,16]on the effectiveness of the community-based management program that is starting to evolve in urban centers around China. The 94% twoyear retention rate of patients in the program is quite high compared to Western programs; it is probably related to the high proportion of patients that were living in the communities with family members (83%).Patients with lower levels of education who had had multiple prior admissions and who were not living with family members were at greatest risk for dropping out of the community management network.
The 18% two-year re-hospitalization rate among patients with schizophrenia under community management identified in this study is within the 12%-38% range of re-hospitalization rates reported from similar studies in Western countries[17-19]. The factors that predicted re-hospitalization included not living with family members, using less antipsychotic medications prior to enrollment, and having more prominent psychotic symptoms and social disability at the time of enrollment.
4.2 Limitations
Schizophrenia is usually a chronic, life-long illness so a two-year follow-up does not necessarily reflect the long-term effects of any intervention. The Community Treatment and Management Network is just starting to evolve in urban China so longer-term assessments will be needed to determine its ultimate value.
We included all patients with a prior psychiatric hospitalization in the Network at 24 Community Health Centers in two districts of Chengdu. It is not possible to say how representative these subjects are of patients participating in the new community management network in different parts of the country. And different communities are managing the networks in different ways so we do not know how generalizable these results would be to other parts of the country. The health care network in rural China is quite different so parallel studies would be needed to demonstrate the effectiveness of community management networks in rural areas.
The exclusion of patients who had never been hospitalized makes it impossible to determine whether or not the community management program can prevent initial hospitalizations of individuals with schizophrenia; this issue will need to be addressed in subsequent studies.
The study only considers one outcome variable,re-hospitalization. And several factors that could be related to re-hospitalization (e.g., negative life events,family economic status, etc.) were not considered in the analysis. More importantly, there are many other factors that may be more important to patients and family members in the re-hospitalization such as control of symptoms, social integration, employment, overall well-being, and so forth. Other studies in China[15,16]have assessed quality of life and social functioning in patients participating in the new communitybased programs. A comprehensive assessment of the community management network must also include follow-up and assessment of changes in all of these variables.
Finally, this was not a controlled study so its impossible to be certain whether or not the relatively low re-hospitalization rates have anything to do with the community management network. And data on re-hospitalization rates prior to the initiation of the management network is not reliable so its not possible to conduct a before-versus-after analysis. It would be necessary to identify similar communities that have not started the community management network and compare the course of individuals with schizophrenia in the two types of communities to definitively demonstrate the effectiveness of the community management networks.
4.3 Significance
Low retention is one of the factors that seriously undermines the effectiveness of community-based programs for patients with schizophrenia in other countries so the very high two-year retention rate in this study (94%) indicates that this approach to the management of patients with schizophrenia in urban China has the potential of being quite successful. The relatively low re-hospitalization rate of 18% suggests that the program is effective, but there is no control group and other—perhaps more important—outcome measures such as social integration and quality of life have not been assessed so it is premature to claim success.
As expected the analysis confirmed that prominent psychotic symptoms and greater social disability at the time of enrollment and less adherence to pharmacotherapy prior to enrollment were associated with re-hospitalization over the subsequent two years so close monitoring of medication use is essential to maintaining patients in the community. One of the key factors that was related both to drop-out from the community management network and to rehospitalization was not living with family members.Clearly this is a high-risk group of patients for whom more specialized or intensive follow-up services are needed. Similarly, prominent negative symptoms at the time of enrollment were associated with multiple hospitalizations over the two-year follow-up period so this is another high-risk group. To reduce rehospitalization rates even further, the community network program needs to develop different types of interventions for different cohorts of patients.
Standardization of the intervention (methods of training community providers, amount of psychiatric involvement, medication algorithms, management of psychiatric crises, etc.) and longer follow-ups considering the full range of factors relevant to the wellbeing of patients with schizophrenia will be needed to demonstrate the effectiveness of this community service network, to adapt the approach to the circumstances of different communities, and to start to individualize the interventions to the needs of different types of patients.
Confict of interest
The authors report no conflicts of interest.
Funding
The study was funded by as part of the funding for the ‘Management and Treatment of Serious Psychiatric Diseases’ project for Chengdu.
1. Killaspy H. From the asylum to community care: learning from experience. Br Med Bull, 2006, 79-80: 245-258.
2. Torrey EF. Jails and prisons—America’s new mental hospitals. Am J Public Health, 1995, 85 (12):1611-1613.
3. Sledge WH, Astrachan B, Thompson K, Rakfeldt J, Leaf P. Case management in psychiatry: an analysis of tasks. Am J Psychiatry,1995, 152 (9):1259-1265.
4. Gerson S, Bassuk E. Psychiatric emergencies: an overview. Am J Psychiatry, 1980, 137(1): 1-11.
5. Wan TT, Ozcan YA. Determinants of psychiatric rehospitalization:a social area analysis. Community Ment Health J, 1991, 27(1):3-16.
6. Oiesvold T, Saarento O, Sytema S, Vinding H, Göstas G,Lönnerberg O, et al. Determinants for readmission risk of new patients: the Nordic Comparative Study on Sectorized Psychiatry.Acta Psychiatrica Scandinavica, 2000, 101: 367-373.
7. Owen C, Rutherford V, Jones M, Tennant C, Smallman A.Noncompliance in psychiatric aftercare. Community Ment Health J, 1997, 33 (1): 25-34.
8. Implementation plan for the recent priorities of the health care system reform (2009-2011). (2009-4-8).http://www.gov.cn/test/2009-04/08/content_1280057.htm. [Accessed 24 December, 2010] (in Chinese)
9. Xie JL, Lü HB. Factors for rehospitalization of schizophrenic patients. Medical Journal of Chinese People’s Health, 2005,17(3): 182-183. (in Chinese)
10. Jin QL. Research on 100 re-onset patients with schizophrenia.Shanghai Arch Psychiatry, 2002, 14(4): 223-225. (in Chinese)
11. Wang YJ. Clinical analysis of 125 re-onset patients with schizophrenia. Medical Journal of Chinese People’s Health, 2011,23(2): 170. (in Chinese)
12. Psychiatric Branch of Chinese Medical Association. Chinese Classification of Mental Disorders. 3rd ed.(CCMD-3). Jinan:Shandong Science and Technology Press, 2001. (in Chinese)
13. He YL, Zhang MY. Positive and negative syndrome scale and its implication. Journal of Clinical Psychiatry, 1997, 7(6): 353-355. (in Chinese)
14. Zhang MY. Manual of psychiatric rating scales. 2nd ed. Changsha:Hunan Science and Technology Press, 2003: 163-166; 214-217. (in Chinese)
15. Zhang HJ, Jin XX. Effects of community intervention on social function and quality of life in patients with schizophrenia.Journal of Psychiatry, 2009, 22(5): 368-370. (in Chinese)
16. Li SC, Lu ZS, Hu YW, Yang RX, Qin D, Ge XW, et al. Influence of integrated intervention on the quality of life in patients with chronic schizophrenia. Journal of Clinical Psychiatry, 2010, 20(1):46-48. (in Chinese)
17. Olfson M, Mechanic D, Boyer CA, Hansell S, Walkup J, Weiden PJ. Assessing clinical predictions of early rehospitalization in schizophrenia. J Nerv Ment Dis, 1999, 187(12):721-729.
18. Owen C, Rutherford V, Jones M, Tennant C, Smallman A.Psychiatric rehospitalization following hospital discharge.Community Ment Health J, 1997, 33(1):13-24.
19. McIntosh J, Worley N. Beyond discharge: telephone followup and aftercare. J Psychosoc Nurs Ment Health Serv, 1994,32(10):21-27.
成都市社区精神分裂症患者再入院的相关因素
张银波 代光智
成都市精神卫生中心(成都市第四人民医院) 610035;通信作者:张银波,电子信箱 boyinzhang@163.com
背景近年来国内提倡对精神分裂症患者以提供社区防治服务为主,然而评价这种服务模式疗效的相关研究为数不多。
目的对纳入成都市社区防治服务系统的精神分裂症患者,评估其继续接受管理服务的比例以及2年内的再住院比例。
方法对成都市金牛区14个社区和青羊区10个社区建档立卡并曾住院治疗的精神分裂症患者随访2年并进行评估。详细记录患者进入本研究时的人口学资料和临床信息,随访2年中每月评估1次并记录患者是否住院。
结果随访2年内,参与本研究的1 027例患者中有963例(93.8%)坚持接受社区防治服务。受教育程度低、独居的患者相对容易脱落。963例中有174例(18.1%)患者在2年内再次住院。Logistic 回归分析显示与再住院相关的因素为入组时未婚、独居、突出的阳性症状和明显的阴性症状,以及在入组前6个月中治疗药物使用不足。
结论城市居民中94%的精神分裂症患者坚持接受社区防治服务,这一比例相当高。2年内18%的再住院比例要低于其他国家类似服务体系下的数据。独居患者脱落以及再住院的风险高,因此要特别关注这一高危人群。为了明确这一社区防治服务体系的作用,需要全面评估与精神分裂症患者康复相关的各种指标 (包括社会整合功能、生活质量以及再住院),也需要在研究时运用标准化的社区干预方法、设立对照组,并随访更长时间。
社区 精神分裂症 再入院 因素分析 前瞻性研究
Background:China has recently introduced a community-based service network for managing individuals with schizophrenia but there has been relatively little formal evaluation of the effectiveness of this approach.Objective:Assess the retention rate and the two-year re-hospitalization rate of patients who are enrolled in the community management network in Chengdu, China.Methods:Patients with a confirmed diagnosis of schizophrenia who had at least one prior hospitalization and who were enrolled in the service network at the community health clinics in 14 communities in the Jinniu District of Chengdu and 10 communities in the Qingyang District of Chengdu participated in the two-year prospective follow-up assessment.Detailed demographic and clinical information was obtained at the time of intake into the follow-up program and their hospitalization status was recorded during monthly evaluations over the subsequent two years.Results:Of the 1 027 participating patients, 963 (93.8%) remained in the program for the entire two-year period. Patients with a lower level of education and those who did not live with family members were more likely to drop-out of the network. Among the 963 patients who completed the follow-up 174 (18.1%) were re-hospitalized over the two-year period. Multivariate logistic regression identified factors related to re-hospitalization: not married or not living with family members, having more prominent positive and negative symptoms at the time of intake, and using medication less in the six months prior to intake.Conclusion:The 94% two-year retention of patients in this urban community management network for individuals with schizophrenia was excellent and the two-year re-hospitalization rate of 18% is better than that reported in most similar programs in other countries. Patients not living with family members were at higher risk for dropping out of the network and for re-hospitalization so this is a high-risk group that deserves special attention. Standardization of the community interventions and longer follow-up studies with control communities that consider the full range of factors relevant to the well-being of patients with schizophrenia (i.e., social integration, quality of life and re-hospitalization) are needed to definitively demonstrate the effectiveness of this community service network.
10.3969/j.issn.1002-0829.2012.01.004
Chengdu Mental Health Center, Fourth People's Hospital, Chengdu 610035, China
*Correspondence: boyinzhang@163.com
(received: 2011-08-16, accepted: 2011-12-14)
- 上海精神医学的其它文章
- SHANGHAI ARCHIVES OF PSYCHIATRY INSTRUCTIONS TO AUTHORS
- Heterogeneity of treatment effects
- Comparison of family functioning and social support between families with a member who has obsessivecompulsive disorder and control families in Shanghai
- Efficacy of contingency management in improving retention and compliance to methadone maintenance treatment:a random controlled study
- Brainnetome of schizophrenia: focus on impaired cognitive function
- Where is the path to recovery when psychiatric hospitalization becomes too difficult?