Clinical Analysis of Placenta Previa Complicated with Previous Caesarean Section△
Liang-kun Ma,Na Han,Jian-qiu Yang,Xu-ming Bian,and Jun-tao Liu*
1Department of Obstetrics &Gynecology,Peking Union Medical College Hospital,Chinese Academy of Medical Sciences &Peking Union Medical College,Beijing 100730,China
2Department of Obstetrics &Gynecology,Tongzhou District Maternal and Child Health Hospital,Beijing 101101,China
PLACENTA previa can have seriously adverse conesquences for both mother and baby,including an increased risk of maternal and neonatal mortality,fetal growth restriction and preterm delivery,antenatal and intrapartum hemorrhage,and women may require a blood transfusion or even an emergency hysterectomy.1The adverse outcomes of placenta previa were even worse among women with previous caesarean section (CS).2In this study,we summarized the clinical profile of placental previa with previous CS in our department retrospectively,and compared with the placental previa without previous CS,as well as to investigate the clinical features and treatment of placenta previa complicated with previous CS.
PATIENTS AND METHODS
Patients
This is a retrospective case study carried out in the Department of Obstetrics and Gynecology,Peking Union Medical College Hospital.This study included all the 272 placenta previa patients who delivered from January 2003 to December 2011.A thorough review of the clinical profiles,detailed obstetrical,puerperal,and neonatal information were obtained from the records.They were divided into a repeated CS (RCS) group and a first CS (FCS) group according to a history of previous caesarean section.The demographic,perinatal characteristics (age,gravidity,gestational age,and birth weight),pregnancy complications(gestational diabetes,preeclampsia,placenta increta,placental abruption,uterine rupture,postpartum hemorrhage,and medical complications),and neonatal outcomes of the FCS group and RCS group were extracted from the medical records,and were compared between the two groups.
Statistical analysis
Statistical analysis was conducted with SPSS software(version 11.0 for Windows;Chicago,IL,USA).Data were statistically analyzed with Student’st-test for quantitative variables andChi-squaretest for qualitative variables.Significance was taken atP<0.05.
RESULTS
The incidence of placenta previa among the total number of deliveries in Peking Union Medical College Hospital was 1.4% (272/19 609).There are 29 patients and 243 patients in the RCS group and FCS group respectively.There was no significant difference in age and average gravidity between the RCS group and the FCS group(allP>0.05,Table 1).
Clinical manifestation
All of the 29 patients were diagnosed as placenta previa by ultrasound before CS.Fifteen (51.7%) cases had painless vaginal bleeding during pregnancy in the RCS group.The first onset of vaginal bleeding was ranging from 17 to 35 weeks.The maximal bleeding amount was 800 mL.One patient had hematuria and difficulty with urination and was diagnosed as placenta increta into bladder by ultrasound and cystoscopy at 32 weeks.She had undergone two previous CS in 2003 and 2009,and three abortions in 2004,September 2010,and November 2010.Her last period was December 2010.Another patient was diagnosed with placenta accreta during the CS,and at delivery,she bled 12 500 mL.
A total of 196 (80.7%) cases were diagnosed as placenta previa by ultrasound before CS.The other 47 cases were diagnosed during the CS by the other reasons.There were 162 (66.7%) cases with vaginal bleeding during pregnancy in the FCS group.The first onset of vaginal bleeding ranged from 25 to 36 weeks.The maximal bleeding amount was 600 mL.The average bleeding amount during pregnancy were 212±42 mL and 219±52 mL in the RCS group and FCS group separately(P>0.05).
Maternal pregnancy outcome
The demographic and perinatal characteristics of the two groups are shown in Table 1.There was no case of maternal mortality.The incidences of placenta accreta,preterm birth,uterus packing,transfusion,disseminated intravascular coagulation,hysterectomy,and postpartum complication between two groups were statistically significant (allP<0.05).
Neonatal outcome
There were 30 and 246 neonates in the RCS group and FCS group respectively (that is,1 and 3 twins in each group).The incidences of preterm birth and neonatal apnea between the two groups were statistically significant (allP<0.05,Table 2).
DISCUSSION
There is an increased risk of placenta previa in a subsequent pregnancy after a previous CS.Furthermore,placenta previa in patients with a previous CS is much more dangerous with an increased risk of massive hemorrhage at delivery.
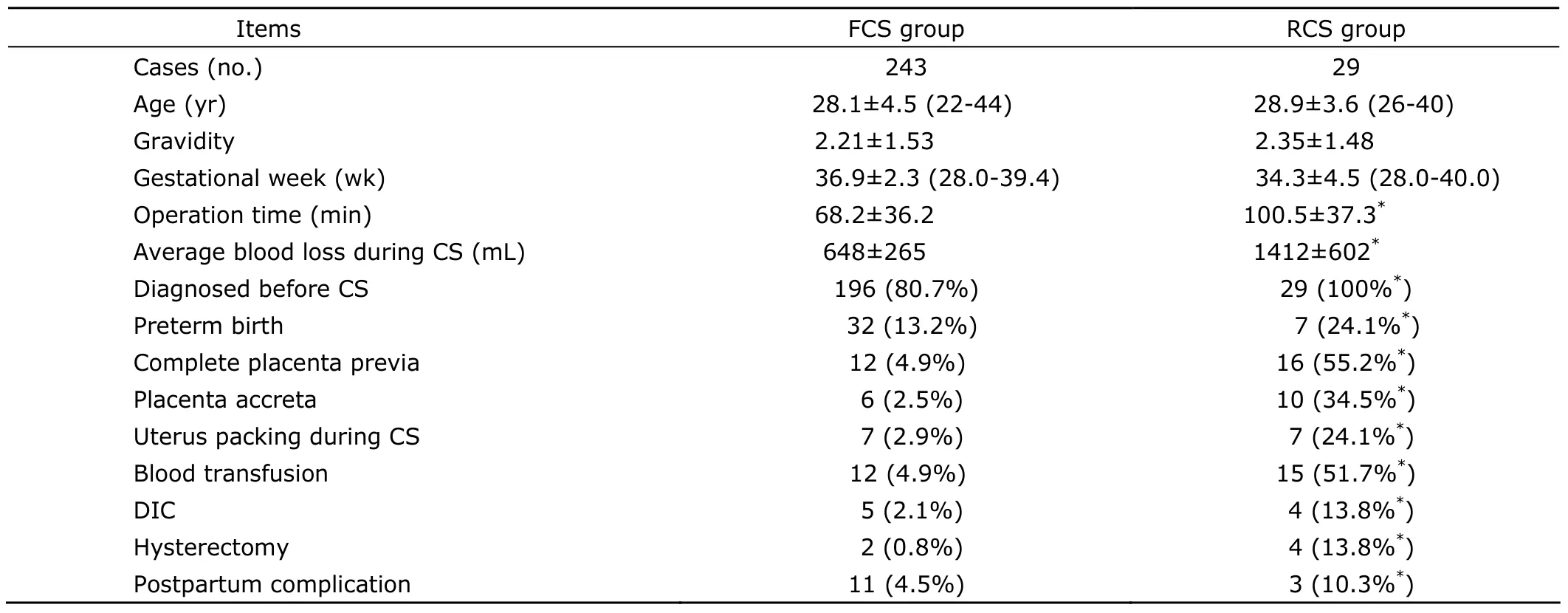
Table 1.Demographic and perinatal characteristics of the two groups
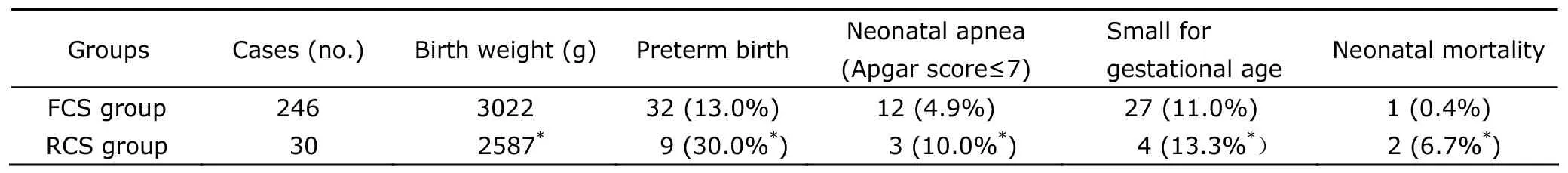
Table 2.Comparisons of neonatal outcome of the two groups
Complete placenta previa and placenta accreta are more common
The abnormal implantation of placenta into the lower segment is called placenta previa.Complete placenta previa is associated with the highest risk of maternal and fetal complication among them.Studies have shown that approximately 90% of second-trimester placenta previa will resolve before term.The apparent movement of the placenta away from the cervix is most likely the consequence of the development of the lower uterine segment,leading to a stationary lower placental edge appearing to move away from the cervix.Recent epidemiological studies have found that the strongest risk factor for placenta previa is a prior CS,3suggesting that a failure of decidualization in the area of a previous uterine scar can have an impact on both implantation and placentation.Ultrasound studies of uterine CS scar have shown the large and deep myometrial defects which are often associated with absence of re-epithelialisation of the scar area.It has been established that scarring of the endometrium as a consequence of caesarean delivery significantly increases the risk of placenta previa,especially complete placenta previa.4In our case series,the incidences of complete placenta previa were 55.2% and 4.9% in the RCS group and FCS group separately (P<0.05).
It is also possible for the placenta to invade the muscles of the uterus (placenta accreta) or grow through the uterine wall (placenta percreta).Several concepts have been proposed to explain the abnormal placentation in placenta accreta including a primary defect of the trophoblast function,a secondary basalis defect due to a failure of normal decidualization,and more recently an abnormal vascularisation and tissue oxygenation of the scar area.These findings support the concept of a primary deciduo-myometrium defect in placenta accreta,exposing the myometrium and its vasculature below the junctional zone to the migrating trophoblast.The vast majority of placenta accreta are found in women presenting with a previous history of CS and a placenta praevia.Jauniaux and Jurkovic5have pointed out that the concept of abnormal decidualization and trophoblastic changes of the placental bed in placenta accreta are secondary to the uterine scar and thus entirely iatrogenic.The incidence of placenta accreta was 34.5% (10 cases) in the RCS group,which was higher than that in the FCS group (2.5%) obviously.Placenta accreta should be suspected in women with a prior CS who has a placenta previa in the current pregnancy.
Increased maternal and fetal morbidity and severe postpartum hemorrhage
Placenta previa with previous CS patients increases the risk of severe postpartum hemorrhage because of the increased incidence of complete placenta previa and placenta accreta.The rate of hysterectomy among women with placenta previa following previous CS increases also.Marshallet al6conducted a systematic review including twenty-one studies (2 282 922 deliveries) and concluded that serious maternal morbidity progressively increased as the number of previous caesarean deliveries increased.The risk of transfusion,uterine package,and hysterectomy were higher in the RCS group than those in the FCS group(allP<0.05).
Predicting factors for maternal morbidity of placenta previa include previous CS,placenta position,and cervical length (CL).Janget al7found that the anterior placenta when located beneath the uterine incision is an important predictor of maternal outcomes in placenta previa patients.Fukushimaet al8evaluated the relationship between CL and obstetrical outcome in women with placenta previa and found that shorter CL (less than 30 mm) was a risk factor both for emergent CS,massive estimated blood loss,placental adherence,and caesarean hysterectomy.
Antepartum ultrasonography in particular plays a crucial role in predicting the risk of hysterectomy in patients with placenta previa.These women should have a targeted sonographic examination for evidence of placenta accreta,placenta position,and CL before delivery.
The fetal morbidity of placenta previa with previous CS is mainly because of antepartum bleeding and preterm birth.There is a higher risk of preterm birth,respiratory distress syndrome,and intrauterine growth restriction.The perinatal mortality rate in the RCS group was approximately 15 times that of the FCS group.
Avoiding unnecessary CS and decreasing the CS rate in China
World Health Organization (WHO) reviewed almost 110 000 births in nine Asian countries in 2007-2008 and found that 46% of births reviewed in China were CS which represented the world's highest rate for the procedure.9Clark and Silver10suggested that the risk of morbidity increases with increasing number of caesarean deliveries.The dominant maternal risk in subsequent pregnancies is the spectrum of placenta accreta and its associated complications.Pregnancies following caesarean delivery also have increased risk for other types of abnormal placentation,reduced fetal growth,preterm birth,and possibly stillbirth.Chronic maternal morbidities associated with caesarean delivery include pelvic pain and adhesions.Adverse reproductive effects may include decreased fertility and increased risk of spontaneous abortion and ectopic pregnancy.Among primary caesarean deliveries in China,at least one quarter were not medically necessary.11Doctors should avoid subjective indications (nonreassuring fetal status and arrest of dilation) and absence of indication(caesarean delivery on maternal request).
Solheimet al12built a decision-analytic model to estimate the future annual incidence of placenta previa,placenta accreta,and maternal mortality in America.If primary and secondary caesarean rates continue to rise as they have in recent years,by 2020 the caesarean delivery rate will be 56.2% from 32.9% in 2009,and there will be an additional 6236 placenta previas,4504 placenta accretas,and 130 maternal deaths annually.Gurol-Urganciet al13made a retrospective cohort study of 399 674 women who gave birth to a singleton first and second baby between April 2000 and February 2009 in England and found that there is an increased risk of placenta previa in the subsequent pregnancy after CS delivery at first birth.Given the placenta previa rate in England and the adjusted effect of previous CS,359 deliveries by CS at first birth would result in one additional case of placenta previa in the next pregnancy.Similarly,China will face more patients at risk of placenta previa and accreta with its potentially severe consequences in the future,based on the current high CS rate.The maternal and neonatal mortality will increase.
Clinicians and patients need to be aware of the longterm risks associated with caesarean delivery so that they can be considered when determining the method of delivery for first and subsequent births.
In conclusion,there are more complete placenta previa and placenta accreta,postpartum hemorrhage,transfusion,uterine packing,obstetric hysterectomy,and perinatal morbidity in the placenta previa with previous CS patients.The doctors should inform the patients of the risks of CS and avoid unnecessary procedures.
We thank all the women who took part in the study and also the research staff involved.We thank Dr.Masoud Afnan,the chief of the Department of Obstetrics &Gynecology,Beijing United Family Hospital and Clinics,with great effort in revising the paper in English.
1.Royal College of Obstetricians and Gynaecologists.Placenta praevia∶diagnosis and management (Green-top 27).[2012-04-24].http∶//www.rcog.org.uk/womens-health/clinical-guidance/placenta-praevia-and-placenta-praeviaaccreta-diagnosis-and-manageme.
2.Oppenheimer L.Society of Obstetricians and Gynaecologists of Canada.Diagnosis and Management of Placenta Previa.J Obstet Gynaecol Can 2007;29∶261-73.
3.Gilliam M,Rosenberg D,Davis F.The likelihood of placenta previa with greater number of cesarean deliveries and higher parity.Obstet Gynecol 2002;99∶976-80.
4.Silver RM,Landon MB,Rouse DJ,et al.Maternal morbidity associated with multiple repeat cesarean deliveries.Obstet Gynecol 2006;107∶1226-32.
5.Jauniaux E,Jurkovic D.Placenta accreta∶pathogenesis of a 20th century iatrogenic uterine disease.Placenta 2012;33∶244-51.
6.Marshall NE,Fu R,Guise JM.Impact of multiple cesarean deliveries on maternal morbidity∶a systematic review.Am J Obstet Gynecol 2011;205∶262.e1-8.
7.Jang DG,We JS,Shin JU,et al.Maternal outcomes according to placental position in placental previa.Int J Med Sci 2011;8∶439-44.
8.Fukushima K,Fujiwara A,Anami A,et al.Cervical length predicts placental adherence and massive hemorrhage in placenta previa.J Obstet Gynaecol Res 2012;38∶192-7.
9.Lumbiganon P,Laopaiboon M,Gülmezoglu AM,et al.Method of delivery and pregnancy outcomes in Asia∶the WHO global survey on maternal and perinatal health 2007-08.Lancet 2010;375∶490-9.
10.Clark EA,Silver RM.Long term maternal morbidity associated with repeated cesarean delivery.Am J Obstet Gynecol 2011;205∶S2-10.
11.Feng XL,Xu L,Guo Y,et al.Factors influencing rising caesarean section rates in China between 1988 and 2008.Bull World Health Organ 2012;90∶30-9.
12.Solheim KN,Esakoff TF,Little SE,et al.The effect of cesarean delivery rates on the future incidence of placenta previa,placenta accrete,and maternal mortality.J Matern Fetal Neonatal Med 2011;24∶1341-6.
13.Gurol-Urganci I,Cromwell DA,Edozien LC,et al.Risk of placenta previa in second birth after first birth cesarean section∶a population-based study and meta-analysis.BMC Pregnancy Childbirth 2011;21∶95-8.
 Chinese Medical Sciences Journal2012年3期
Chinese Medical Sciences Journal2012年3期
- Chinese Medical Sciences Journal的其它文章
- Hypercalcemia Appeared in a Patient with Glucagonoma Treated with Octreotide Acetate Long-acting Release
- Zinc Finger Protein-activating Transcription Factor Up-regulates Vascular Endothelial Growth Factor-A Expression in Vitro△
- Comparison of Clinical Effects of Au-Pt Based and Ni-Cr Based Porcelain Crowns
- Hipbone Biomechanical Finite Element Analysis and Clinical Study after the Resection of Ischiopubic Tumors△
- Accuracy Validation for Medical Image Registration Algorithms:a Review△
- Nucleotide-binding Oligomerization Domain-1 Ligand Induces Inflammation and Attenuates Glucose Uptake in Human Adipocytes△
