The St.George’s Respiratory Questionnaire in Lymphangioleiomyomatosis△
Kai-feng Xu*,Lan Wang,Xin-lun Tian,Yao-song Gui,Min Peng,Bai-qiang Cai,and Yuan-jue Zhu
Department of Respiratory Medicine,Peking Union Medical College Hospital,Chinese Academy of Medical Sciences &Peking Union Medical College,Beijing 100730,China
LYMPHANGIOLEIOMYOMATOSIS (LAM) is a rare progressive multi-system disease characterized by diffuse cystic changes in lung with an estimated prevalence of one in 400 000 adult women.1,2It affects mainly young females with an average age at diagnosis around forty years.The onset is usually insidious;however,dyspnea could develop abruptly in the case of pulmonary complications such as pneumothorax or chylothorax.Pulmonary function deteriorates progressively until,in the late stage,patients depend on oxygen and require lung transplantation.Sporadic LAM shares similar mutations of TSC2 or TSC1 genes with LAM associated with tuberous sclerosis complex (TSC).2Dysfunction of TSC1/TSC2 complex activates mammalian target of rapamycin (mTOR),resulting in abnormal growth of smooth muscle-like cells in lung,kidney,and other organs.
The health-related quality of life in LAM patients is greatly affected.National Heart,Lung,and Blood Institute(NHLBI) LAM Registry study suggested that quality of life,measured by SF-36 and St.George’s Respiratory Questionnaire (SGRQ),was decreased in LAM patients and related to symptoms and lung function.3The quality of life could therefore be an important measurement in evaluation of this rare and chronically progressive disease.In this study,we compared the scores of SGRQ in confirmed LAM patients,reflecting the quality of life,with the results of the most commonly used physiological measures,so as to evaluate the applicability of SGRQ in LAM.
PATIENTS AND METHODS
Patients
In June 2007,the SGRQ was introduced into evaluation of LAM in Peking Union Medical College Hospital.Since then and up to November 2009,38 patients have been diagnosed as LAM and hence included in this retrospective analysis.Confirmation of diagnosis in this study required typical clinical presentation,in combination with either pathological diagnosis,angiomyolipoma,or TSC.Patients received lung transplantation were excluded.
Measurements
The common physiological measures involved in the analysis included the Borg scale of breathlessness at rest,6-minute walking distance (6MWD),arterial blood gas analysis at rest,and pulmonary function tests.All the results of those tests and SGRQ for each patient were obtained at the same visit.Only data of the first test were used for correlation analysis if a test was performed several times for a same subject.
The Chinese version of self-administered SGRQ comprises three components:symptoms,activity,and impacts.4,5The total score and the score of each of the three components range from 0 to 100,reflecting a cline from the best to the worst condition.Subjects answered all the questions following the standard procedure required for SGRQ.4The Borg scale,estimating patient’s sense of breathlessness at rest,was answered along with the SGRQ.The Borg scale is recorded from 0 to 10,zero meaning no breathlessness at all and 10 meaning maximum difficulty in breathing.6MWD was performed according to the American Thoracic Society (ATS) statement.6Samples for arterial blood gas analysis were drawn at rest in room atmosphere.Pulmonary function tests were performed in accordance with ATS standards and comprised of forced expiratory volume in one second (FEV1),forced vital capacity(FVC),residual volume (RV),total lung capacity (TLC),and diffusion capacity of lung for carbon monoxide (DLCO).
Treatment
Ten cases of LAM patients received off-label treatment of sirolimus (Rapamune produced by Wyeth Pharmaceuticals,or Yi-Xin-Ke produced by North China Pharmaceutical Group Corp.,China),upon the written consent from the patients and the approval from the Ethical Committee of our hospital.The patients were administrated with an oral dose of 2 mg per day.The blood concentration of sirolimus was not measured during treatment unless dose adjustment was needed in the case of dissatisfactory clinical response.Only one patient had trough blood concentration (12.9 ng/mL)tested.The SGRQ scores before and after treatment were collected.Other measurements were not included for analysis because of incompleteness of the data.
Other therapies received by the patients included oxygen,inhaled bronchodialators when necessary,with or without inhaled corticosteroids.
Statistical analysis
The collected data were processed with SPSS 11.0.Numerical values were expressed as means±SD.The correlations were expressed as Pearson’s correlation coefficient(r).Pairedt-tests were carried out to compare values before and after treatment.APvalue less than 0.05 was considered statistically significant.
RESULTS
The mean age of the included 38 LAM patients was 38.58±8.98 years (range,22.00-54.00).Of those patients,36 were sporadic LAM and 2 were associated with TSC.Angiomyolipoma was seen in 21 of the sporadic LAM cases(58.3%) and both of the TSC associated LAM.
The physiological measurements and available test results of all patients included in this study are listed in Table 1.All available data were collected,but some of them were incomplete because of the nature of retrospective case review.All the patients finished the SGRQ and the Borg scale.The numbers of patients completing 6MWD,blood gas analysis,spirometry,and spirometry plus RV/TLC/DLCO were 10,20,21,and 17 respectively.Figure 1 shows the SGRQ total score distribution in all the 38 cases of LAM.
All three components and total scores of SGRQ were found significantly correlated with the Borg scale of breathlessness,6MWD,arterial partial pressure of oxygen(PaO2),alveolar-arterial oxygen gradient [P(A-a)O2],FEV1,and FEV1/FVC (allP<0.05) (Table 2,Fig.2).The SGRQ total,activity,and impacts,but not symptoms,were correlated with FVC and DLCO.The SGRQ total and activity,but not symptoms and impacts,were correlated with RV/TLC ratio.Two pulmonary function indices,RV and TLC,were not found correlated with the quality of life measured by SGRQ.It seems that the scores of activity and impacts in SGRQ might correlated more closely with the physiological measures than symptoms score does.The strongest correlation was found between the SGRQ total score and the Borg scale of breathlessness (r=0.90,P<0.01).
Some patients in this study received off-label use of sirolimus.Ten cases with data of both baseline and after treatment were analyzed.Figure 3A shows SGRQ total scores at different time points after sirolimus treatment(n=10).Paired comparison between baseline and 101-200 days after sirolimus treatment found all three components and total scores of SGRQ were significantly improved (Fig.3B,n=6,allP<0.05).The Borg scale was also significantly improved from 5.33±1.51 to 3.67±1.86 (P<0.05).

Table 1.Physiological measurement results and SGRQ scores in 38 female LAM patients
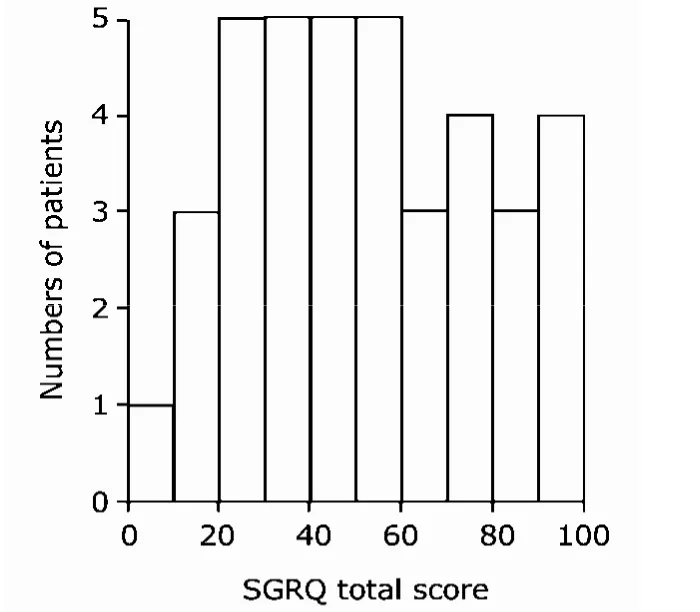
Figure 1.Distribution histogram of the SGRQ total scores of 38 LAM patients.
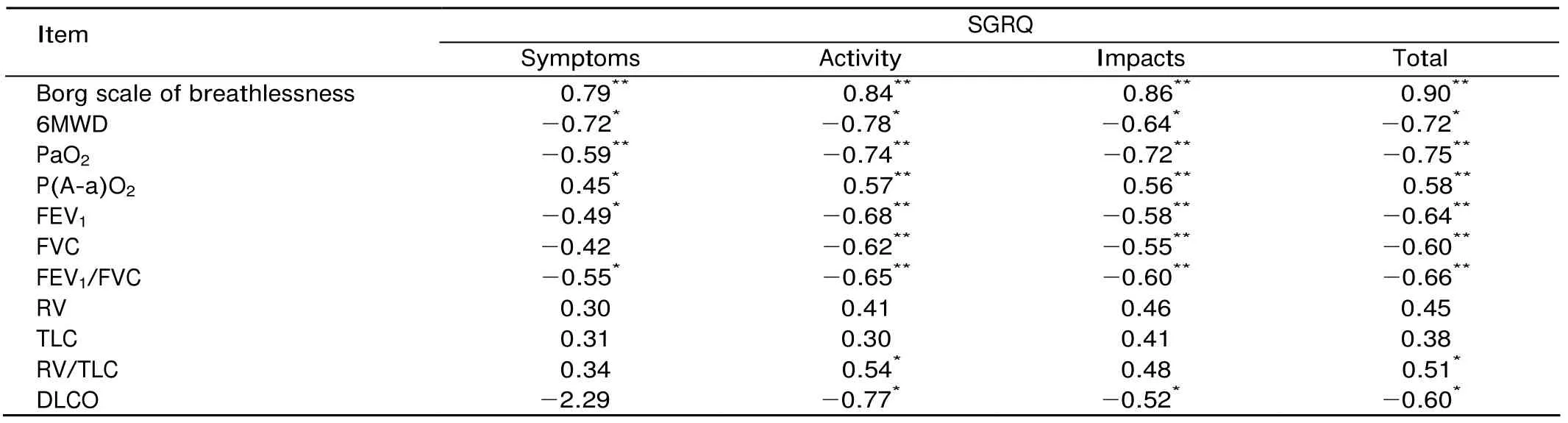
Table 2.Correlations between the SGRQ scores and physiological measures

Figure 2.Regression plot of the SGRQ total score vs.the Borg scale of breathlessness (A),FEV1(B),6MWD (C),and PaO2(D).

Figure 3.The SGRQ score after treatment with sirolimus.
DISCUSSION
The SGRQ was developed to evaluate patients with chronic obstructive pulmonary disease (COPD) and asthma.4Its usage in several different languages including Chinese has been validated.5While the application of the SGRQ in COPD and asthma has been well established,that in rare lung diseases,such as LAM,has not been validated yet.NHLBI LAM Registry study measured quality of life with the SF-36 and the SGRQ for LAM Registry patients.7The physical component score of SF-36 was found correlated with spirometry,diffusion capacity,and symptoms.The three components and total scores in LAM Registry patients were correlated with FEV1and symptoms as well.
It was found in the present study that the quality of life in LAM patients measured by the SGRQ was correlated well with commonly used physiological measurements.The strong correlation between the SGRQ scores and the Borg scale is not surprising as breathlessness is one of the most complained symptoms in LAM patients.5In this retrospective analysis,the SGRQ scores were also found correlated with the degree of limitation of activity (measured by 6MWD),arterial oxygen levels [measured by PaO2and P(A-a)O2],and pulmonary function (measured by FEV1,FVC,and FEV1/FVC).RV and TLC were not correlated with the SGRQ in this analysis although RV/TLC shows correlations with SGRQ activity and total scores.Correlations were also found between diffusion capacity of lung in LAM patients and the SGRQ activity,impacts,and total scores.Overall,the SGRQ measurements were correlated well with the most commonly used clinical physiological measures in LAM patients,especially the Borg scale of breathlessness,6MWD,PaO2,and FEV1.Therefore,it could be concluded that the SGRQ measurements correlated with the disease severity.The average of FEV1was 53.58%±27.16% predicted in our patients,and it was 70.3%±1.6% predicted in NHLBI LAM Registry patients,8suggesting that the LAM patients in this report were probably severer than those in NHLBI LAM Registry.
LAM patients are usually under the stress of physical disability at young age,exacerbated by impaired social relationship,difficulty in access to professional medical advices,lack of effective treatment,and problems in medical costs.In an email survey by LAM China in April,2009,24 patients between age of 25 and 52 responded.Ten of them had quitted their job because of their illness,4 of them worked part-time,and only 10 of them kept a full-time job.Basic medical insurance covered only half of those patients.9Of all the impacts caused by this disease,physical measurements reflect only the degree of physical impairment.The SGRQ could therefore be an important complementary measurement to reveal the psychological,social,and other factors in this chronic,progressive,and rare lung disease.As our observations also suggested the applicability of the SGRQ in LAM,we recommend that this questionnaire could be included in evaluation and follow-up of LAM patients.
Apart from reflecting the severity of LAM,the measurement of quality of life could be applied as a parameter in evaluating the effects of intervention as well.In this retrospective analysis,the SGRQ scores enabled us to look at the effects of sirolimus on the quality of life.In a nested observation of sirolimus in treating angiomyolipoma,sirolimus improved FEV1,FVC,and RV in 11 patients with LAM,but not 6MWD and DLCO.7In the 10 cases received sirolimus in the present study,that mTOR inhibitor improved quality of life.In the 6 patients with available data of both baseline and 101-200 days after sirolimus treatment,all three components and total scores of SGRQ were significantly improved.The Borg scale of breathlessness was also improved significantly.However,we could not conclude whether the improved quality of life was accompanied by less limited activity,elevated blood oxygen level,or improved pulmonary function,due to the lack of corresponding data from 6MWD,blood oxygen,and spirometry.In addition,given the absence of control in this analysis,placebo effect could not be ruled out.The ongoing clinical trial of MILES,a randomized,placebo-controlled trial of sirolimus in patients with LAM,is expected to shed more light on the potential effects of sirolimus in treating LAM (ClinicalTrial.org,Identifier:NCT00414648).
In summary,the SGRQ scores are correlated well with commonly used clinical measures in LAM,such as the Borg scale of breathlessness,6MWD,blood oxygen levels,and pulmonary functions.Based on these findings,the SGRQ could be corporated in evaluation of patients with LAM and evaluation of efficacy of novel treatment.
ACKNOWLEDGEMENT
We thank LAM China (http://www.lamchina.org) and all the patients participating in this study.
1.McCormack FX.Lymphangioleiomyomatosis,a clinical update.Chest2008;133:507-16.
2.Johnson SR,Cordier JF,Lazor R,et al.European Respiratory Society guidelines for the diagnosis and management of lymphangioleiomyomatosis.Eur Respir J 2010;5:14-26.
3.Ryu JH,Moss J,Beck GJ,et al.The NHLBI lymphangioleiomyomatosis registry.Characteristics of 230 patients at enrollment.Am J Respir Crit Care Med 2006;173:105-11.
4.Jones PW,Quirk FH,Baveystock CM.The St.George’s Respiratory Questionnaire.Respir Med 1991;85:25-31.
5.Lu WX,Zhang YJ,Hu B,et al.Application of St.George’s respiratory questionnaire in evaluating the life quality of Chinese patients with chronic obstructive pulmonary disease.Chin J Tuberc Respir Dis 2003;26:195-8.
6.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories.ATS statement:guidelines for the six-minute walk test.Am J Respir Crit Care Med 2002;166:111-7.
7.Bissler JJ,McCormack FX,Young LR,et al.Sirolimus for angiomyolipoma in tuberous sclerosis complex or lymphangioleiomyomatosis.N Engl J Med2008;358:140-51.
8.Juvet SC,McCormack FX,Kwiatkowski DJ,et al.Molecular pathogenesis of lymphangioleiomyomatosis:lessons learned from orphans.Am J Respir Cell Mol Biol2007;36:398-408.
9.Xu KF.Follow-up of LAM patients in April 2009.[cited 2010 Jul 23].Available from:http://www.lamchina.org/lamnews.asp?articleid=228.
 Chinese Medical Sciences Journal2010年3期
Chinese Medical Sciences Journal2010年3期
- Chinese Medical Sciences Journal的其它文章
- Cicatricial Pemphigoid in Accompany with Rheumatoid Arthritis:a Case Report
- Non-Hodgkin’s Lymphoma Primarily Presenting with Fanconi Syndrome and Acute Kidney Injury
- Laparoscopic Partial Splenectomy for Giant Hemangioma Misdiagnosed as Splenic Cyst:a Case Report
- Clinical and Pathological Features of Riedel’s Thyroiditis
- Diagnosis and Treatment of Infective Endocarditis in Chronic Hemodialysis Patients△
- Effects of Acute Normovolemic Hemodilution on Perioperative Coagulation and Fibrinolysis in Elderly Patients Undergoing Hepatic Carcinectomy△
